Abstract
Aims
Rates of glaucoma surgery have declined in North America and continental Europe in recent years. The aim of this study was to examine trends over time and regional variation in rates of trabeculectomy in England.
Methods
The hospital in-patient enquiry (HIPE), hospital episode statistics (HES), and the Oxford record linkage study (ORLS) were analysed for annual trabeculectomy admissions between 1976 and 2004.
Results
Annual rates of admission for trabeculectomy rose 10-fold from 1976 to 1995: from 3.7 (95% confidence intervals 3.5–3.9) admissions per 100 000 population in 1976 to a peak of 38.7 (38.1–39.3) in 1995. Admission rates then declined sharply and have begun to reach a plateau at around 10.6 (10.3–10.9) in 2004. The highest surgical rates during the period 1997–2004 were found in the 80- to 84-year-old age group. Geographical analysis showed wide variation across local authority areas in annual rates of trabeculectomy, from 4 (2.3–5.2) to 33 (29.0–36.5) people per 100 000 population in 1998–2004. The rate of surgery by local authority showed little or no association with the level of social deprivation in each area.
Conclusions
The rate of patients undergoing trabeculectomy increased substantially over 20 years. This was followed by a profound reduction in rates of trabeculectomy from 1995, which coincides with the introduction of new topical medications to reduce intraocular pressure. Wide regional variation in rates of trabulectomy was found, but there was no evidence of reduced access to glaucoma surgery in deprived areas.
Similar content being viewed by others
Introduction
Glaucoma is one of the most common causes of preventable visual impairment in England and Wales.1 The prevalence of primary open-angle glaucoma is rising and is predicted to increase by one-third in England and Wales over the next 20 years.2 The treatment of glaucoma has traditionally started with medical management followed by filtration surgery, with the option of laser surgery being used in some cases.
Rates of glaucoma surgery have declined in North America and continental Europe in recent years.3, 4, 5, 6, 7, 8, 9, 10 Similarly, two studies have reported reductions in the total number of patients undergoing trabeculectomy in England over the past decade.11, 12 Whittaker et al11 showed from Hospital Episode Statistics (HES, described below) that the annual number of patients undergoing trabeculectomy in England increased year on year from 10 115 (1989–1990) to 18 928 (1995–1996), then decreased year on year to 14 507 (1997–1998). More recently, Fraser et al12 used HES data collected in a newer format to show that the annual number of patients undergoing trabeculectomy decreased year on year from 8622 (1998–9) to 4206 (2003–4).
We have analysed trends over time in national rates of trabeculectomy in England, using routinely collected hospital statistics, to determine the scale of change over the period 1976–2004.
Materials and methods
At the starting date of our analysis, 1976, English national hospital statistics were collected as the hospital in-patient enquiry (HIPE). This comprised a statistical summary of a one-in-ten sample of all hospital discharges. The data were intended, as a random one-in-ten sample, to be representative of hospital care throughout England. The sampling was performed and the data were collected by each of the (then) 14 Regional Health Authorities of England and were collated and analysed nationally by the (then) Office of Population Censuses and Surveys. This system ceased in 1985 and was replaced, though not until 1989, by HES. HES have been collected on all hospital in-patient and day case admissions since then, rather than on a sample of all admissions. Both HIPE and HES are statistical databases of demographic, medical, and administrative information about each episode of hospital care, similar to the data systems known as hospital separation systems in some other countries. For simplicity, we use the term ‘admissions’ to cover episodes of in-patient care and of day case care. HES now include all admissions to NHS hospitals in England and admissions funded by the NHS for treatment elsewhere, including external providers such as Independent Sector Treatment Centres. From 1998, HES also contains linked data relating to successive episodes of care for each person, which means that data about individuals can be traced through multiple episodes of care.
Annual admission rates for trabeculectomy were calculated from HIPE and HES for the years 1976–2004; from 1998 to 2004, rates were calculated distinguishing episodes of care and individual people treated. In addition, annual admission rates for trabeculectomy were calculated while confining the analysis (both numerator and denominator) to people aged 40 years and over, for ease of comparison with previously published research.
The Oxford Record Linkage Study (ORLS) consists of computerised abstracts of HES, including day cases, for all patients treated in the former Oxford Regional Health Authority (ORHA) area. From its start, the ORLS collected linked data (as above for HES from 1998), so that data about individuals can be traced through multiple episodes of care. The ORLS was the source of the Oxford component of the HIPE data from 1976 to 1985; it continued through the period 1985–1988 when national data ceased; and, from 1989, the ORLS and the Oxford component of HES are basically the same data set. The ORLS has had no counterpart in other English regions. The mean population of the ORLS region throughout the study period has been around 2.5 million people, whereas the population of England has been around 50 million; thus, the ORLS data set comprised around 5% of the English total. The university city of Oxford comprises only about 6% of the population covered by the ORLS. In general, the remainder of the ORLS areas may be regarded as reasonably typical ‘middle England’; in particular, the ORLS population is on average slightly healthier and slightly more economically favoured than ‘industrial England’. Admission rates were calculated for the ORLS area, distinguishing episodes of care and individual people treated, from 1976 to 2004.
In the ‘people’ component of the linked analyses—ORLS from 1976, and HES from 1998—individual patients who undergo trabeculectomy are counted once only in each year, even if they have more than one episode of care on which the fact of trabeculectomy is recorded.
English national HES were analysed to produce a geographical profile of hospital admission for trabeculectomy by local authority (LA) between 1998 and 2004. The data were used to construct a map showing the person-based admission rate per 100 000 resident population for each LA, expressed as an average annual rate. The LAs were arranged into quintiles: one-fifth of LAs with the lowest rates are shown with the lightest colour and one-fifth of LAs with the highest rates are shown with the darkest colour. The mean annual rates of trabeculectomy between 1998 and 2004 were also analysed at the level of Government Office Regions (GORs) and were used to construct a map showing the person-based admission rate per 100 000 resident population for each GOR; as above, GORs with the lowest rates are shown with the lightest colour and GORs with highest rates are shown with the darkest colour.
The admission rate for each LA was plotted against its score for the index of multiple deprivation (IMD 2004).13 The IMD is a measure of socioeconomic deprivation, which we used at the level of the LA area. The IMD was developed in England by the Office of the Deputy Prime Minister and the Department for the Environment, Transport, and the Regions. Seven distinct domains of social and economic deprivation are measured separately and the final index is calculated as a weighted measure of the domains. The seven domain indices are: income, employment, health and disability, barriers to housing and services, living environment, crime, and education, skills and training.13
The operative codes used to identify trabeculectomy from the data sets were: 157.4 in the office of population, Censuses and Surveys Classification of Surgical Operations and Procedures, third revision (OPCS3), and C60.1 in OPCS4. Although English national HIPE started in the 1950s, and the ORLS started in 1963, we selected the start date of 1976 for our study because trabeculectomy was not a uniquely coded operation until then.
Results
English national admission rates for trabeculectomy are shown in Figure 1. Annual admission rates for surgery were 3.7 (95% confidence intervals 3.5–3.9) episodes per 100 000 population in the mid-1970s. They increased slowly but steadily over the next 10 years to 9.1 (8.8–9.4) in the mid-1980s. By the time that recording of HES started in 1989, the rate of surgery had already begun to increase sharply: it continued to increase rapidly over the next 5 years from 18.3 (17.9–18.7) episodes per 100 000 population in 1989 to a peak of 38.7 (38.1–39.3) in 1995. Over the past 12 years, the rate of surgery has decreased substantially from 38.7 (38.1–39.3) in 1995 to 10.6 (10.3–10.9) in 2004, though the rate of decline has slowed since 2000. Similarly, linked data demonstrate that the annual admission rate for surgery has decreased from 21.9 (21.7–22.1) people per 100 000 population in 1998 to 9.5 (9.3–9.7) in 2004.
Raw numbers of episodes were analysed to produce population rates, but have not been included for every year in this paper. For the most recent data analysed (2004–5), 5289 episodes of trabeculectomy were recorded in England in the year, which comprised 4756 people who underwent trabeculectomy. By comparison, 18 676 episodes of trabeculectomy were recorded in England at the peak of surgical rates in 1995–1996.
Annual admission rates for trabeculectomy in people aged 40 years and over were 78.0 (76.8–79.2) episodes per 100 000 population in 1994, 83.0 (81.8–84.2) at the peak of surgical activity in 1995, and have since declined to 21.1 (20.5–21.7) in 2004.
ORLS admission rates for trabeculectomy are shown in Figure 2. ORLS rates increased gradually from 1976 to 1988, before rising dramatically from 6.2 episodes per 100 000 population in 1988 to a peak of 34.7 (32.4–37.0) in 1994. Since then, surgical rates have fallen substantially to 11.6 (10.3–12.9) in 2004, though the rate of decline has again slowed over recent years. ORLS rates reached a peak 1 year earlier than national rates, but otherwise followed national trends closely.
ORLS data, and HES data from 1998, show rates based on the number of people admitted to hospital for trabeculectomy as well as the number of episodes of care for surgery (episodes of separate admission and/or transfers within an admission). These data show that the scale of multiple admissions per person was small, although a small increase in multiple recording in the ORLS data is evident in the mid-1990s, shown by the modest divergence between the rates for episodes and people (Figure 2). The ORLS data confirm that the large changes in hospital episodes in the 1990s represent large changes in the number of individuals treated. They also show, more accurately than the national figures (which omit data for 1986–1988), that the time of rapid increase in surgery was about 1988–1989. The linked national data confirm that the significant decrease in hospital episodes from 1998 to 2004 represents a significant decline in the number of individuals undergoing surgery.
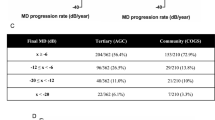
Using HIPE and HES data, national admission rates for trabeculectomy were analysed by age and sex over three time periods and are presented in Figure 3. The first period (1976–1985) represented a time of low surgical rates, whereas the second period (1989–1996) was a time of rapidly increasing rates and the third period (1997–2004) a time of decreasing rates. For both sexes and all age groups over 40 years, surgical rates were lowest in 1976–1985, highest in 1989–1996, and intermediate in 1997–2004. Surgical rates were higher in women than men for all age groups over all the three time periods. In 1976–1985, the highest rate of surgery was found in the 75- to 79-year-old age group; by 1997–2004, the highest surgical rate had shifted to the 80—to 84-year-old group. From 1989–1996 to 1997–2004, surgical rates have decreased least in the age group over 85 years.
Figure 4 shows a geographical profile of the annual rate of trabeculectomy by LA, analysed using HES data. LAs showed a wide variation in rates of trabeculectomy, ranging from 4 (2.3–5.2) to 33 (29.0–36.5) people per 100 000 population in 1998–2004. Figure 5 illustrates the scale of variation; it shows that wide variation is attributable not just to small numbers of atypical outlying areas, but that there is a general gradation of highly varying rates across the country. As seen in the error bars, the variation is highly statistically significant. The rate of surgery by LA showed little or no correlation with the IMD (r2=0.038), as illustrated in Figure 6. Figure 7 shows a geographical profile of the annual rate of trabeculectomy by GOR, analysed using HES data. This demonstrates that the South West is the region with the highest surgical rates (13.0 people per 100 000 population), with London being the next highest (12.8) and West Midlands the lowest (10.0).
Discussion
National rates of trabeculectomy in England increased dramatically from the late 1980s to reach a peak in the mid-1990s. Similarly, the Oxford data showed a fivefold increase from 1988 to 1994. During this period, there were surgical advances and refinements in technique that improved safety and reduced postoperative complications. The success rate was improved by the use of antimetabolites. The increase in surgical activity may also have resulted from studies that suggested that surgical management of glaucoma produced better results than medical therapy.14, 15 It is also possible that the increase may have represented a backlog of unoperated glaucoma patients, analogous to the bulge in cataract operations observed when phacoemulsification and local anaesthesia were introduced in the late 1980s.16
Trabeculectomy rates have declined steeply from the mid-1990s, and have begun to reach a plateau at around 10 episodes per 100 000 population. This has occurred despite the introduction of more sensitive methods of glaucoma detection and monitoring, and the introduction of low target pressures. The major factor responsible for this change is a growing tendency for ophthalmologists to use medical therapy in the treatment of glaucoma. Primary care data show that the population prevalence of medical therapy for glaucoma in the United Kingdom has increased from 1.7% (1994) to 2.3% (2003).3 New agents with improved control of intraocular pressure were introduced in the 1990s and the volume of prescribing has increased dramatically in Britain over the past decade.4, 5, 6, 12 In particular, topical prostaglandin analogues were licensed in 1996, which coincides with the rapid decline in the rates of trabeculectomy; they are now typically first-line agents for open-angle glaucoma, and several other classes of topical agents may be added long before surgery is indicated.
HES are limited by the exclusion of surgery conducted in the private sector. As the use of private health care has generally increased over the study period, it can be assumed that the increase in trabeculectomy in the NHS is an underestimate of the real increase in England over the same time period. However, for similar reasons, the subsequent decrease in trabeculectomy in the NHS may be an overestimate of the real decrease in England.
Our data show surgical rates per 100 000 population rather than the numbers of operations, and therefore provide a more consistent picture of trends against demographic changes such as an expanding and ageing population. However, we have included some data on number of operations, which may be useful in the consideration of service provision in ophthalmology. We also analysed linked ORLS data for the whole study period, and linked HES data from 1998, which distinguish the number of patients undergoing surgery from the number of episodes of care. These linked data validate the HES episode data by confirming that the observed changes represent real changes in the number of patients undergoing surgery. ORLS data also provide a more consistent and complete historical record of surgical activity than HES data.
Rates of trabeculectomy have been declining throughout Britain. In Scotland, the annual rate of trabeculectomy has decreased year on year from around 33 operations per 100 000 population in 1994 to around 13 in 2004.4 This decline is similar to that seen in England (36 episodes per 100 000 population in 1994 to 11 in 2004), though slightly less steep. Analysed in another way, the annual rate of trabeculectomy in Scotland has decreased year on year from 46 operations per 1000 population aged 40 years and over likely to have glaucoma in 1994 to 15 in 2004.4 In addition, surgical rates and prescribing rates of glaucoma have been compared in four geographical areas in Scotland: the rate of trabeculectomy decreased by 46% from 1994 to 1999, in association with a 25% increase in rates of prescribed items.5 Similarly, the number of patients undergoing trabeculectomy performed in Ireland decreased by over 60% from 1996 to 2003, in association with a 30% (Northern Ireland) and 59% (Republic of Ireland) increase in prescription items, causing an increase of 227% in the cost of medical therapy in the Republic of Ireland.6
Other European countries have experienced variable decreases in rates of trabeculectomy over recent years. In the Netherlands, the annual number of glaucoma operations in patients with open-angle glaucoma or ocular hypertension has decreased from 2400 (1995) to 1350 (2003).7 In France, the number of people on topical antihypertensive therapy has increased from 410 000 (1997) to 734 000 (2000), in association with a small decrease of 5% in the total number of surgical interventions for glaucoma.8
In Ontario, the rate of trabeculectomy decreased from 46 (1996) to 38 (2004) per 1000 population at risk of primary open-angle glaucoma; the decrease in surgical rates over this time period correlated strongly (P<0.001) with an increase in the use of prostaglandin analogues, which were introduced in 1996.10 In the United States, the number of patients with open-angle glaucoma undergoing trabeculectomy under Medicare provision decreased by 72% (in-patient) and 42% (outpatient) from 1994 to 1999, despite a stable prevalence of Medicare patients diagnosed with glaucoma.17 In Australia, the rate of trabeculectomy has decreased by 58% from 1994 to 2003, whereas the total number of prescriptions for glaucoma increased from 1.9 million to 3.3 million.9 Interestingly, the rate of secondary procedures (repeat trabeculectomy, implantation of drainage device, or cycloablation) remained stable, with some variation between states.9
The role of trabeculectomy has changed dramatically over the past decade since the introduction of the prostaglandin analogues. Before 1996, the main indications for trabeculectomy in the United Kingdom were failure of medication to control intraocular pressure (57% of patients) and progressive visual field loss (27% of patients), and over half of the patients had advanced visual field damage by the time of listing for surgery.18 Since the introduction of new topical agents, fewer patients may now fall into the first category. Appropriate indications for trabeculectomy may now include progressive visual field loss as a consequence of suboptimal intraocular pressure control on medical therapy, as well as intolerance of multiple medications or poor compliance. Although it is possible that the rate will increase again in time, particularly in the context of lower target intraocular pressures, this is not yet evident.
Rates of trabeculectomy differed widely among LAs in England, but this variation showed little or no association with the degree of socioeconomic deprivation in each LA. This suggests that there is no reduction in access to glaucoma surgery in areas with high levels of social deprivation. However, confounding factors must be considered: for example, areas with higher social deprivation might have higher prevalence of glaucoma, for example, through a higher concentration of people at risk of glaucoma because of ethnic origin. In addition, referral patterns and subspecialisation in glaucoma surgery may have an effect on regional variation. Trabeculectomy is increasingly performed in specialist centres with higher surgical turnover; these are typically found in cities where levels of deprivation are coincidentally higher.
The number of annual admissions for trabeculectomy has decreased from 18 676 episodes in 1995 to 5289 in 2004. This most recent figure represents the lowest number of trabeculectomy operations performed per year in England for at least 16 years. This significant decline has important implications for service provision in ophthalmology, in particular the number of ophthalmologists and glaucoma surgeons required in the future. Together with increased specialisation in glaucoma surgery, it also means that fewer cases are now suitable for trainees to operate on. The data presented on trends over time and regional variation in glaucoma surgery should be helpful in matching capacity to demand for surgery across the country, as well as in planning resource allocation for medical and surgical therapy.
References
Bunce C, Wormald R . Leading causes of certification for blindness and partial sight in England and Wales. BMC Public Health 2006; 6: 58.
Tuck MW, Crick RP . The projected increase in glaucoma due to an ageing population. Ophthalmic Physiol Opt 2003; 23 (2): 175–179.
Owen CG, Carey IM, De Wilde S, Whincup PH, Wormald R, Cook DG . The epidemiology of medical treatment for glaucoma and ocular hypertension in the United Kingdom: 1994 to 2003. Br J Ophthalmol 2006; 90 (7): 861–868.
MacLeod SM, Clark R, Forrest J, Bain M, Bateman N, Azuara-Blanco A . A review of glaucoma treatment in Scotland 1994–2004. Eye 2008; 22: 251–255.
Bateman DN, Clark R, Azuara-Blanco A, Bain M, Forrest J . The effects of new topical treatments on management of glaucoma in Scotland: an examination of ophthalmological health care. Br J Ophthalmol 2002; 86 (5): 551–554.
Knox FA, Barry M, McGowan B, O'Brien C . The rising cost of glaucoma drugs in Ireland 1996–2003. Br J Ophthalmol 2006; 90 (2): 162–165.
van der Valk R, Schouten JS, Webers CA, Beckers HJ, van Amelsvoort LG, Schouten HJ et al. The impact of a nationwide introduction of new drugs and a treatment protocol for glaucoma on the number of glaucoma surgeries. J Glaucoma 2005; 14 (3): 239–242.
Baudouin C, Rouland JF, Le Pen C . Changes in medical and surgical treatments of glaucoma between 1997 and 2000 in France. Eur J Ophthalmol 2003; 13 (Suppl 4): S53–S60.
Walland MJ . Glaucoma treatment in Australia: changing patterns of therapy 1994–2003. Clin Experiment Ophthalmol 2004; 32 (6): 590–596.
Rachmiel R, Trope GE, Chipman ML, Gouws P, Buys YM . Effect of medical therapy on glaucoma filtration surgery rates in Ontario. Arch Ophthalmol 2006; 124 (10): 1472–1477.
Whittaker KW, Gillow JT, Cunliffe IA . Is the role of trabeculectomy in glaucoma management changing? Eye 2001; 15 (4): 449–452.
Fraser SG, Wormald RP . Hospital episode statistics and changing trends in glaucoma surgery. Eye 2008; 22: 3–7.
Noble M, Wright G, Dibben C, Smith GAN, McLennan D, Antilla C et al. Index of Multiple Deprivation 2004. Office of the Deputy Prime Minister: London, 2004.
Jay JL, Murray SB . Early trabeculectomy versus conventional management in primary open angle glaucoma. Br J Ophthalmol 1988; 72 (12): 881–889.
Migdal C, Hitchings R . Control of chronic simple glaucoma with primary medical, surgical and laser treatment. Trans Ophthalmol Soc UK 1986; 105 (6): 653–656.
Keenan TD, Rosen P, Yeates D, Goldacre MJ . Time trends and geographical variation in cataract surgery rates in England: study of surgical workload. Online First Br J Ophthalmol 2007; 91: 901–904.
Strutton DR, Walt JG . Trends in glaucoma surgery before and after the introduction of new topical glaucoma pharmacotherapies. J Glaucoma 2004; 13 (3): 221–226.
Edmunds B, Thompson JR, Salmon JF, Wormald RP . The National Survey of Trabeculectomy. I. Sample and methods. Eye 1999; 13 (4): 524–530.
Acknowledgements
Geographical atlases of surgical rates were produced using data provided through EDINA UKBORDERS with the support of the Economic and Social Research Council (ESRC) and the Joint Information Systemic Committee (JISC) together with boundary material, which is copyright of the Crown.
Funding: The Unit of Health-Care Epidemiology is funded to undertake research on the regional and national hospital databases by the English NHS National Coordinating Centre for Research Capacity Development. Researchers are independent of funders.
Ethical approval: The data sets are anonymised. Approval to analyse them in a programme of research undertaken by the Unit of Health-Care Epidemiology, Oxford University has been obtained through the NHS Central Office for Research Ethics Committees (reference 04/Q2006/176).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Keenan, T., Salmon, J., Yeates, D. et al. Trends in rates of trabeculectomy in England. Eye 23, 1141–1149 (2009). https://doi.org/10.1038/eye.2008.195
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.195
Keywords
This article is cited by
-
Global rates of glaucoma surgery
Graefe's Archive for Clinical and Experimental Ophthalmology (2013)
-
Recent trends in the rate of trabeculectomy in England
Eye (2011)
-
Trends in the rate of trabeculectomy
Eye (2010)