Abstract
The basic route and mechanism for diapedesis has not yet to be fully defined. Here we present evidence that "cell-cell separation" between endothelial cells (ECs) may provide a route for leukocyte diapedesis. We unexpectedly found that extensive interaction between peripheral blood leukocytes and ECs that were activated by TNF-α induced the opening of EC contacts and, surprisingly, resulted in cell-cell separation. This event was specific to the intercellular adhesion molecules-1 (ICAM-1)/leukocyte function-associated antigen-1 interaction, as demonstrated by the following: (1) ICAM-1 expression correlated with increased EC contraction; and (2) the blocking of ICAM-1 selectively inhibited EC separation. Thus, we suggest that "cell-cell separation" could be a mechanism for diapedesis in situations that may require massive leukocyte infiltration.
Similar content being viewed by others
Introduction
Leukocyte extravasation is a critical event in immune surveillance (Springer, 1994). This phenomenon occurs by migration of leukocytes either directly through individual microvascular endothelial cells (ECs) (transcellular route) or between them, at interendothelial cell junctions (papacelluar route) (Greenwood et al., 1994; Feng et al., 1998). In both cases, the process is characterized by sequential events: arrest from rolling mediated by selectin, integrin-dependent firm adhesion, and transmigration across the endothelium (Springer, 1994). However, some fundamental aspects of diapedesis remain incompletely understood. For example, large numbers of leukocytes need to rapidly migrate from blood vessels to inflamed tissue during acute inflammation (Godaly et al., 2001). Previous studies have only provided a limited explanation of this rapid and excessive transmigration.
In the present study, we unexpectedly found that the binding of a large number of peripheral blood leukocytes (PBLs) to cultured endothelium induced a cascade of events in ECs; contraction of ECs, opening of EC contacts, and, eventually, endothelial cell-cell separation. This observation led to the hypothesis that the induction of cell-cell separation by leukocyte-EC interaction is a novel regulatory mechanism for leukocyte transendothelial migration (TEM), especially, in situations that require massive infiltration of immune cells. In fact, it has been demonstrated that an early event of acute inflammation is coupled with the alterations of EC shape and cell junctions, described as "retraction" or "contraction", and viewed as inter-endothelial gap formation, respectively (Majno and Palade, 1961; Majno et al., 1969; Wysolmerski and Lagunoff, 1990; McDonald et al., 1999). However, none of these previous studies reported the phenomenon that leukocyte-EC interaction induces endothelial cell-cell separation.
The intercellular adhesion molecules-1 (ICAM-1)/leukocyte function-associated antigen-1 (LFA-1) interaction has been considered one of the major pairs of adhesion molecules contributing to the different steps of leukocyte migration across the endothelium (Gahmberg et al., 1997; Hogg et al., 2003). Recent studies have demonstrated that in addition to its role as an adhesion molecule, ICAM-1 has a functional role in ECs during diapedesis. For instance, ligation of ICAM-1 is known to promote opening of EC contacts by inducing an increase in intracellular free calcium [Ca2+]i. ICAM-1 is also known to enhance EC contraction by activating myosin light-kinase and, subsequently, p38-MAPK and Rho-GTPase (Hixenbaugh et al., 1997; Greenwood et al., 2003; Muller, 2003; Ley et al., 2007; Oh et al., 2007). In the present study, we investigated whether ICAM-1/LFA-1-mediated EC contraction is coupled with endothelial cell-cell separation.
Results
Leukocyte binding to ECs resulted in cell-cell separation
In the underflow adhesion and migration assay, HUVECs under physiologic shear stress, both with and without TNF-α stimulation, appeared static when viewed macroscopically (Figure 1A and B). Addition of a small number of SDF-1α (100 ng/ml)-treated PBLs (approximately 2 × 105 cells/200 µl) also did not significantly induce morphological changes of HUVECs (Figure 1A and B). However, when higher numbers of SDF-1α-treated PBLs (approximately 1 × 106 cells/200 µl) were added onto TNF-α-activated HUVECs, increased leukocyte-EC interactions facilitated contraction of ECs, opening of EC contacts, and, eventually, endothelial cell-cell separation (Figure 1C). After EC separation some PBLs separated from the contracted ECs and migrated toward the separating region of the ECs. In HUVECs without TNF-α stimulation, addition of even higher numbers of SDF-1α-treated PBLs did not induce cell-cell separation (data not shown), suggesting that PBL-induced endothelial cell-cell separation needs activation of HUVECs.
Dynamic behavior of HUVECs during the interaction with leukocytes under shear-flow condition. (A) Experimental scheme for live-cell dynamic imaging as described in Methods. (B) Dynamic behavior of endothelial cells under a shear-flow condition. Upper panels show time-lapse images of non-activated HUVECs with and without interaction with PBLs (2 × 105 cells/200 µl). Lower panels show time-lapse images of TNF-α activated HUVECs under the same experimental conditions. (C) Increased number of PBLs (1 × 106 cells/200 µl) were flowed on TNF-α activated HUVECs and resulted in "cell-cell separation" between HUVECs.
Increased EC contraction parallels ICAM-1 levels
Stimulation of ECs with TNF-α results in dramatic phenotypic and functional alterations including induction of cell adhesion molecule ICAM-1 (Pfau et al., 1995). We next explored whether endothelial cell-cell separation is dependent on adhesion molecules between ECs and leukocytes, and if so, what molecules are involved. To explore this we examined the expression and distribution pattern of adhesion molecules (ICAM-1 and CD31 (PECAM-1)) and a junctional protein zona occludens 1 (ZO-1) on HUVECs before and after TNF-α stimulation (10 ng/ml, 24 h). We found that the expression level of the ICAM-1 protein varied in TNF-α-stimulated HUVECs. Interestingly, the increased ICAM-1 level was paralleled by the increased EC contraction (Figure 2A). ICAM-1 was highly enriched in the contracting microspikes of the F-actin structure in TNF-α-activated HUVECs (Figure 2A). In contrast to the ICAM-1, ZO-1 and PECAM-1 redistributed from the cell-cell junctional areas to other areas of the cell; this redistribution occurred without a change in the expression levels of the proteins when endothelial-cell junctional contacts were disrupted by the activation of HUVECs (Figure 2A).
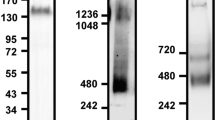
Effects of ICAM-1 expression on EC height and contractility. (A) The monolayers of HUVECs were incubated with TNF-α for 0 h or 24 h at 37℃. Cells were fixed and stained with ICAM-1 (R6.5; green), ZO-1 (green), PECAM-1 (green) and actin (phallodin-TRITC; red) and subjected to confocal microscopy with reconstitution in the z-axis. (B) The expression level of the ICAM-1 varied in TNF-α stimulated HUVECs for 24 h. The EC height of EC expressing low level of ICAM-1 (IC1lo), high level of ICAM-1 (IC1hi) and contracted EC expressing high level of (IC1hi-C) was analyzed, respectively (a and b). The EC height of HUVECs stimulated or unstimulated with TNF-α for 24 h was measured, respectively (c and d). The crossline (yellow) represents the site for the indicated orthogonal view. EC height was calculated by the sum of the z-axes in an orthogonal view (height of combined Z-sections) using FLUOVIEW software.
As shown in Figure 2B(a), the orthogonal view (z-axis) of EC images revealed that contracted ECs that expressed high levels of ICAM-1 (IC1hi-C) showed greater z-axis height that ECs that expressed low level of ICAM-1 (IC1lo). This result raised a question about whether ICAM-1 by itself directly contributes to the increase in cell height or the increased height of the EC is just due to the contraction of the cell. We first compared the relationship between the expression level of ICAM-1 and the height of the z-axis. As shown in Figure 2B(b), the height of the z-axis correlated with the levels of ICAM-1 expression, thereby suggesting that ICAM-1 not only contributes to the increase in cell height but is also required for the EC contraction, even in the absence of ligand engagement. This result was further corroborated by comparing the height of ECs before and after TNF-α stimulation (Figure 2B(c, d)).
ICAM-1/LFA-1 interaction is critical for cell-cell separation
Based on the fact that ICAM-1 expression correlated with the increased cell height and EC contraction, we next tested whether engagement of ICAM-1 with LFA-1 stimulates EC contractility and thereby induces endothelial cell-cell separation. We also considered the effect of shear stress on the cell-cell separation induced by leukocyte/EC interaction. To this end, we monitored the behavior of inactivated or TNF-α-activated HUVECs during interaction with PBLs under the static flow condition. Without TNF-α stimulation, addition of PBLs did not induce EC contractility in either the presence or absence of SDF-1α (Figure 3). In contrast, after TNF-α stimulation, HUVECs revealed enhanced contractility in response to the interaction with the SDF-1α-treated PBLs (Figure 3). Even though shear stress has been shown to promote leukocyte transmigration (Cinamon et al., 2001), we observed that this endothelial cell-cell separation phenomenon is not dependent on shear stress.
ICAM-1/LFA-1 interaction is essential for leukocyte-induced cell-cell separation between ECs. PBLs (5 × 105 cells) stimulated with SDF-α were incubated on monolayers of HUVECs with or without TNF-α stimulation and monitored by time-lapse microscopy. The cells were treated with R6.5 antibody (10 µg/ml) to block the interaction of ICAM-1 with LFA-1. Selected images are shown at 0, 10, 30, 50 and 60 min of incubation from a representative experiment. White dot lines represent the border line of cell membranes and the arrow heads indicate a change of direction between contraction and respreading.
Another cellular event that we found out in the present experiment was that activated HUVECs underwent a "contraction-and-respreading" cycle during interaction with the leukocytes without shear forces (Figure 3). Relaxation to its original phenotype was only occurred within 10-20 min after initial contraction of ECs (Figure 3, white dot lines and arrow heads). This result suggests that ECs can actively participate in controlling diapedesis, and this control is primarily initiated by the engagement of leukocytes. More interestingly, EC separation was significantly inhibited by an antibody that blocked ICAM-1/LFA-1 interaction (i.e., R6.5). This finding indicates that engagement of ICAM-1 with LFA-1 is critical for stimulating endothelial cell-cell separation induced by leukocyte/endothelial interaction (Figure 3). Taken together, these results demonstrate that EC contractility and subsequent cell-cell separation events are mediated by a specific interaction of ICAM-1/LFA-1, whereas shear stress has little effect on endothelial contraction.
Discussion
Crossing endothelial barriers is required for leukocyte trafficking and immune surveillance. By using a simplified in vitro model to monitor endothelial behavior under either static or flow conditions, we unexpectedly found that enhanced endothelial contraction stimulated by leukocyte binding results in "cell-cell separation". We explored the effects of ICAM-1 expression on EC contractility and height induction and found that ICAM-1/LFA-1 interaction is critical for the initiation of the EC contraction and the subsequent cell-cell separation. We also found that leukocyte-activated ECs underwent a cycling of "contraction-and-respreading" during the period of time-lapse microscopic monitoring. These results strongly suggest that the EC is not static but dynamic enough to actively guide and control leukocyte TEM. Based on these results, we also suggest that endothelial cell-cell separation, which is distinct from junctional separation or disruption between cell-cell borders (Ley et al., 2007), may provide a novel physical route for leukocytes to migrate through endothelial barriers.
The route taken by blood leukocytes as they cross the EC is of critical mechanistic and regulatory importance. Leukocyte migration through paracellular route is well characterized mechanism of diapedesis (Ley et al., 2007). Migration through this route is associated with the opening of endothelial-cell contacts via the activation of myosin light-chain kinase and subsequent endothelial-cell contraction (Ley et al., 2007). In addition, this route requires redistribution of junctional molecules in a way that favors TEM (Yang, 2002). Endothelial junctional molecules such as PECAM-1 and JAM-A may mobilize to the luminal surface, thus creating an adhesive haptotactic gradient that guides luminal leukocytes to the junctions (Ley et al., 2007). However, we suggest that migration through the separated region of ECs (cell-cell separation) is distinct from the classical paracellular route. For example, cell-cell separation can induce significant morphological changes that are not resembled to the junctional separation or disruption. Thus, migration through separated region of ECs may not require the guidance of junctional molecules including PECAM-1 and JAM-A. Since cell-cell separation can make relatively bigger space or hole than junctional separation, leukocyte adhered on ECs may easily transmigrate through this region even in the absence of the guidance of junctional molecules. We therefore suggest that endothelial cell-cell separation may be beneficial for the rapid transmigration of large numbers of leukocytes in which junctional separation or disruption may have a limited explanation.
It has been reported that shear stress facilitates leukocyte extravasation (Cinamon et al., 2001). Based on that report, we examined the effect of shear stress on EC separation. Contrary to our expectations, shear stress had no significant influence on endothelial cell-cell separation, as this separation was also seen under static conditions. Rather, ICAM-1/LFA-1 interaction was shown to be a more critical factor than shear stress (Rose, 2006). These results suggest that an active role of ICAM-1 on ECs is crucial for endothelial contractility, whereas the contribution of the physiological shear stress in blood vessels is insignificant. However, since in vivo endothelial cells and leukocytes are continuously exposed to fluid shear stresses, the physiological relevance of these in vitro observations remains to be determined in an appropriate in vivo experimental model.
It has been known that increased ICAM-1 expression causes EC leakiness, cytoskeletal reorganization and junctional alterations (Clark et al., 2007). In addition, this cellular event is coupled with the increased adhesion of circulating leukocytes to the EC luminal surface (Clark et al., 2007). In the current study, the finding that cells which express high levels of ICAM-1 (IC1hi-C) reveal an increased EC contraction and junctional alteration (Figure 2A and B) also corroborates the pervious reports by others (Muller, 2001, 2003). Nonetheless, it would be important to consider why previous works failed to evaluate the event of "cell-cell separation" in vitro or in vivo. We suggest that our ability to detect endothelial cell-cell separation in this work is primarily a consequence of utilizing time-lapse live-cell imaging system coupled with high magnification. Under the low magnification and no time-lapse imaging system, it will not be easy to detect the dynamic shape changes of ECs. Thus, our assessment of "cell-cell separation" may be underestimated. Another possibility is that such a high number of PBLs may induce an oxidative-stress response of the endothelium. Of particular interest is the role of reactive oxygen species (ROS). ROS are known to impair cell-cell adhesion in EC and are important regulators of endothelial integrity through their indirect stimulation of tyrosine kinase activity. In addition, vascular ROS play an important role in the development of cardiovascular disease (Hordijk, 2006). Although no report has been directly addressed the effect of ROS in endothelial cell-cell separation, it has been reported that oxidants induces shape changes of epithelial cells and eventually separation of them (Welsh et al., 1985).
An important question to emerge from these studies is how the barrier function of the endothelium is preserved after cell-cell separation during leukocytes diapedesis. Several studies have demonstrated junctional alteration of ECs and inter-endothelial gap formation during diapedesis (McDonald et al., 1999; Johnson-Leger et al., 2000; Clark et al., 2007; Ley et al., 2007). However, we were particularly interested in whether contracted endothelium can be relaxed to recover its barrier function, because no report, to our knowledge, has directly addressed this question yet. In our study, contracted ECs began to relax and recover their original shape just within 10-20 min (Figure 3). These results further suggest that ECs can dynamically participate in controlling leukocyte diapedesis once it is activated by the interaction with leukocytes. While the "contraction-respreading" cycle of ECs is mainly mediated by ICAM-1/LFA-1, the detailed mechanism was not determined in the current study and requires further exploration. Previous reports have shown that ligation of ICAM-1 triggers an increase in intracellular calcium and activation of myosin light chains, MAPK, and Rho GTPase, thereby enhancing cell contraction and promoting the opening of interendothelial contacts (Hixenbaugh et al., 1997; Greenwood et al., 2003; Muller, 2003; Ley et al., 2007; Oh et al., 2007). Further studies are necessary to examine a potential involvement of these ICAM-1-mediated signaling cascades in the "contraction-respreading" cycle of ECs.
In conclusion, we have presented evidence that EC separation mediated by LFA-1/ICAM-1 interaction may facilitate the passage of leukocytes through vascular endothelium and provide a route for rapid and efficient diapedesis of leukocytes. This previously unrecognized active role of ECs mediated by ICAM-1/LFA-1 interaction will provide new insights into the basic mechanisms of leukocyte trafficking and transmigration.
Methods
Cell culture
Human umbilical vascular endothelial cells (HUVECs) were isolated from umbilical cord veins, and established as primary cultures in a complete endothelial growth medium (EGM; Cambrex Bioscience, Baltimore, MD) supplemented with 2% FBS, bovine brain extract, hEGF, hydrocortisone and gentamicin. COS-7 cells (ATCC CRL-1651, Manassas, VA) were grown in DMEM medium supplemented with 10% heat-inactivated FBS. Human PBLs were isolated from normal donors by dextran sedimentation followed by centrifugation through a discontinuous Ficoll gradient (Amersham Biosciences, Little Chalfont, England).
Antibodies and reagents
The antibody to human ICAM-1 (R6.5) was purified from an R6.5 hybridoma (ATCC, HB 9580), and the anti-ZO-1 antibody was purchased from Zymed (Zymed, San Francisco, CA). Anti-PECAM antibody and recombinant TNF-α and stromal cell-derived factor-1α (SDF-1α) were purchased from R&D systems (R&D, Minneapolis, MN). Phycoerythrin or FITC-conjugated anti-mouse IgG and phalloidin-TRITC were purchased from Sigma (St. Louis, MO).
Immunofluorescence staining and confocal imaging
HUVECs were grown on glass coverslips (18-mm diameter; Fisher Scientific, Pittsburgh, PA) or on chamber slides (Nalge Nunc International, Naperville, IL). HUVECs were treated for 24 h with TNF-α (10 ng/ml). The cells were fixed, washed twice with PBS, and blocked with 5% goat serum (DAKO, Glostrup, Denmark) in PBS for 30 min. They were then incubated with primary antibodies in blocking buffer for 3 h at room temperature, rinsed three times with PBS, incubated with secondary antibody in blocking buffer for 1 h at RT, rinsed three times with PBS, and mounted with anti-fade solution (Molecular Probes, Eugene, OR). The primary antibodies used were anti-ICAM-1 (R6.5), anti-ZO-1 and anti- PECAM-1; the secondary antibodies used were FITC or TRITC-conjugated goat anti-mouse and anti-rabbit IgG (Sigma). F-actin was detected using phalloidin-TRITC (Sigma). The slides were examined with an FV1000 confocal laser scanning microscope (Olympus Corporation, Japan) equipped with 40×, 63×, and 100× objectives. Cell height was calculated by the sum of the z-axes in an orthogonal view (height of combined Z-sections) using FLUOVIEW software.
Live cell imaging
For shear experiments, HUVECs were seeded on fibronectin-coated coverslips, and grown to confluence. Coverslips were mounted in a flow chamber device and maintained at 37℃. Cells were exposed to shear stress at 2 dyn/cm2 for 1-2 min through the controlled flow of L-15 media, and then PBLs were resuspended at 0.2-1 × 106/200 µl in L-15/5% FBS, loaded into the chamber under shear stress at 0.2 dyn/cm2 for 5 min, to allow accumulation, and then subjected to a constant shear force of 2 dyn/cm2 for 50 min. Unless otherwise indicated, PBLs were pretreated with SDF-1α (100 ng/ml) just before addition to the HUVECs. The behaviors of HUVECs interacting with PBLs were monitored, as described by Oh et al. (2007).
For static experiments, HUVECs grown on coverslips coated with fibronectin were placed in a live chamber device. SDF-1α-treated PBLs (5 × 105 cells) were added and allowed to settle on the monolayer of HUVECs. Sequential differential interference contrast images were acquired using an Axiovert 200 inverted microscope equipped with a 60× objective (Carl Zeiss, Jena, Germany).
Abbreviations
- ECs:
-
endothelial cells
- HUVECs:
-
human umbilical vascular endothelial cells
- ICAM-1:
-
intercellular adhesion molecules-1
- LFA-1:
-
leukocyte function-associated antigen-1
- PBLs:
-
peripheral blood leukocytes
- PECAM-1:
-
platelet/endothelial cell adhesion molecule 1
- SDF-1α:
-
stromal cell-derived factor-1α
- TEM:
-
leukocyte transendothelial migration
- ZO-1:
-
zona occludens 1
References
Cinamon G, Shinder V, Alon R . Shear forces promote lymphocyte migration across vascular endothelium bearing apical chemokines . Nat Immunol 2001 ; 2 : 515 - 522
Clark PR, Manes TD, Pober JS, Kluger MS . Increased ICAM-1 expression causes endothelial cell leakiness, cytoskeletal reorganization and junctional alterations . J Invest Dermatol 2007 ; 127 : 762 - 774
Feng D, Nagy JA, Pyne K, Dvorak HF, Dvorak AM . Neutrophils emigrate from venules by a transendothelial cell pathway in response to FMLP . J Exp Med 1998 ; 187 : 903 - 915
Gahmberg CG, Tolvanen M, Kotovuori P . Leukocyte adhesion--structure and function of human leukocyte beta2-integrins and their cellular ligands . Eur J Biochem 1997 ; 245 : 215 - 232
Godaly G, Bergsten G, Hang L, Fischer H, Frendeus B, Lundstedt AC, Samuelsson M, Samuelsson P, Svanborg C . Neutrophil recruitment, chemokine receptors, and resistance to mucosal infection . J Leukoc Biol 2001 ; 69 : 899 - 906
Greenwood J, Howes R, Lightman S . The blood-retinal barrier in experimental autoimmune uveoretinitis. Leukocyte interactions and functional damage . Lab Invest 1994 ; 70 : 39 - 52
Greenwood J, Amos CL, Walters CE, Couraud PO, Lyck R, Engelhardt B, Adamson P . Intracellular domain of brain endothelial intercellular adhesion molecule-1 is essential for T lymphocyte-mediated signaling and migration . J Immunol 2003 ; 171 : 2099 - 2108
Hixenbaugh EA, Goeckeler ZM, Papaiya NN, Wysolmerski RB, Silverstein SC, Huang AJ . Stimulated neutrophils induce myosin light chain phosphorylation and isometric tension in endothelial cells . Am J Physiol 1997 ; 273 : H981 - H988
Hogg N, Laschinger M, Giles K, McDowall A . T-cell integrins: more than just sticking points . J Cell Sci 2003 ; 116 : 4695 - 4705
Hordijk PL . Endothelial signalling events during leukocyte transmigration . Febs J 2006 ; 273 : 4408 - 4415
Johnson-Leger C, Aurrand-Lions M, Imhof BA . The parting of the endothelium: miracle, or simply a junctional affair ? J Cell Sci 2000 ; 113 : 921 - 933
Ley K, Laudanna C, Cybulsky MI, Nourshargh S . Getting to the site of inflammation: the leukocyte adhesion cascade updated . Nat Rev Immunol 2007 ; 7 : 678 - 689
Majno G, Palade GE . Studies on inflammation. 1. The effect of histamine and serotonin on vascular permeability: an electron microscopic study . J Biophys Biochem Cytol 1961 ; 11 : 571 - 605
Majno G, Shea SM, Leventhal M . Endothelial contraction induced by histamine-type mediators: an electron microscopic study . J Cell Biol 1969 ; 42 : 647 - 672
McDonald DM, Thurston G, Baluk P . Endothelial gaps as sites for plasma leakage in inflammation . Microcirculation 1999 ; 6 : 7 - 22
Muller WA . Migration of leukocytes across endothelial junctions: some concepts and controversies . Microcirculation 2001 ; 8 : 181 - 193
Muller WA . Leukocyte-endothelial-cell interactions in leukocyte transmigration and the inflammatory response . Trends Immunol 2003 ; 24 : 327 - 334
Oh HM, Lee S, Na BR, Wee H, Kim SH, Choi SC, Lee KM, Jun CD . RKIKK motif in the intracellular domain is critical for spatial and dynamic organization of ICAM-1: functional implication for the leukocyte adhesion and transmigration . Mol Biol Cell 2007 ; 18 : 2322 - 2335
Pfau S, Leitenberg D, Rinder H, Smith BR, Pardi R, Bender JR . Lymphocyte adhesion-dependent calcium signaling in human endothelial cells . J Cell Biol 1995 ; 128 : 969 - 978
Rose . The role of the a4 integrin-paxillin interaction in regulating leukocyte trafficking . Exp Mol Med 2006 ; 38 : 191 - 195
Springer TA . Traffic signals for lymphocyte recirculation and leukocyte emigration: the multistep paradigm . Cell 1994 ; 76 : 301 - 314
Welsh MJ, Shasby DM, Husted RM . Oxidants increase paracellular permeability in a cultured epithelial cell line . J Clin Invest 1985 ; 76 : 1155 - 1168
Wysolmerski RB, Lagunoff D . Involvement of myosin light-chain kinase in endothelial cell retraction . Proc Natl Acad Sci U S A 1990 ; 87 : 16 - 20
Yang HS, Kim H, Choi YM, Hwang KJ, Kwo HC, Kim SK, Cho DJ . Expresion of integrins, cyclooxygenases and matrix metalloproteases in three-dimensional human endometrial cell culture system . Exp Mol Med 2002 ; 34 : 75 - 82
Acknowledgements
This work was supported by grants from the Basic Research Program (R01-2008-000-20989-0), the SRC program (R11-2007-007-01002-0), the Molecular and Cellular BioDiscovery Research Program (No. 2006-02516) of MOST/KOSEF, and the Research Program (2008-C00265) of Korea Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Wee, H., Oh, HM., Jo, JH. et al. ICAM-1/LFA-1 interaction contributes to the induction of endothelial cell-cell separation: implication for enhanced leukocyte diapedesis. Exp Mol Med 41, 341–348 (2009). https://doi.org/10.3858/emm.2009.41.5.038
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.3858/emm.2009.41.5.038
Keywords
This article is cited by
-
ICAM-1 on the luminal surface of endothelial cells is induced to a greater extent in mouse retina than in other tissues in diabetes
Diabetologia (2022)
-
Liver sinusoidal endothelial cell ICAM-1 mediated tumor/endothelial crosstalk drives the development of liver metastasis by initiating inflammatory and angiogenic responses
Scientific Reports (2019)
-
Decreased expression of the β2 integrin on tumor cells is associated with a reduction in liver metastasis of colorectal cancer in mice
BMC Cancer (2017)
-
Interaction of endothelial cells with macrophages—linking molecular and metabolic signaling
Pflügers Archiv - European Journal of Physiology (2017)
-
VEGF-A Promotes Both Pro-angiogenic and Neurotrophic Capacities for Nerve Recovery After Compressive Neuropathy in Rats
Molecular Neurobiology (2015)