Abstract
The purpose of this study was to investigate the expression of IL-16 in the rheumatoid synovium and the role of inflammatory cytokines and Toll-like receptor (TLR) ligands in IL-16 production by fibroblastlike synoviocytes (FLS) of rheumatoid arthritis (RA) patients. Immunohistochemical staining was performed with a monoclonal antibody to IL-16 in synovial tissues from patients with RA and likewise in patients with osteoarthritis (OA). FLS were isolated from RA synovial tissues and stimulated with IL-15, IL-1β, IFN-γ, and IL-17. The IL-16 mRNA level was assessed by semiquantitative RT-PCR and real time (RT) PCR and a comparison was made between IL-16 mRNA levels produced by RA-FLS and OA-FLS. Production of IL-16 was identified by a western blot assay, and IL-16 production after stimulation by specific ligands of TLR2 and TLR4 was assessed by RT-PCR. While immunohistochemical staining demonstrated strong expression of IL-16 mRNA in synovial tissues from patients with RA, similar findings were not present in the OA group. Moreover, mRNA expression of IL-16 by RA-FLS increased after treatment with IL-17 but not with IL-15, IL-1β, and IFN-γ. Specifically, IL-17 increased IL-16 mRNA level by RA-FLS and peripheral blood mononuclear cells in a dose-dependent manner. However, IL-17 did not stimulate IL-16 production in OA-FLS. Peptidoglycan, a selective TLR2 ligand, also increased production of IL-16 by RA-FLS dosedependently, whereas LPS, a selective TLR4 ligand, had no such stimulatory effect. The results from our data demonstrate that IL-17 and TLR2 ligands stimulate the production of IL-16 by RA-FLS.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a chronic systemic inflammatory disorder that is characterized by synovial hyperplasia, neoangiogenesis, and progressive destruction of cartilage and bone (Weyand and Goronzy, 1997; Koch, 1998). T cells comprise a large proportion of the inflammatory cells infiltrating the RA synovium responsible for such changes, and thus is the reason RA is considered a Th-1-associated disease. T cell activation and migration into the synovium is important for the initiation and perpetuation of the disease (Weyand and Goronzy, 1997).
IL-16 is a 17 kDa chemoattractant identified initially by its actions on T cells (Center et al., 1997). Recent studies show that IL-16 contributes to the regulatory process of CD4+ immune cell recruitment and activation at sites of inflammation through the binding of the D4 region of CD4 on lymphocytes (Wu et al., 1999). IL-16 is synthesized by a variety of immune (T cells, eosinophils, and dendritic cells) and nonimmune cells (fibroblasts, epithelial cells, and neuronal cells) (Cruikshank et al., 2000). The principal site of IL-16 production in the joint is the CD68- fibroblast-like cells of the synovial lining (Franz et al., 1998).
Franz et al. (1998) showed that IL-16 is produced and IL-16 mRNA is expressed in human synovial fibroblasts from patients with RA, but not in cells from patients with osteoarthritis (OA). In synovial fluid, IL-16 concentration correlates positively with chemotactic activity, and the highest concentrations have been observed in patients with early RA (Franz et al., 1998). Synovial fibroblasts from patients with RA produce high levels of IL-16 in response to RA-IgG, and this is one possible mechanism through which T cells infiltrate articular tissues in RA (Pritchard et al., 2004). The expression of IL-16 increases in cultured fibroblast-like synoviocytes (FLS) stimulated by IL-1β (Sciaky et al., 2000).
In inflammatory arthritis, IL-17 plays key roles in the propagation of joint inflammation, cartilage destruction, and bone erosion (Lubberts et al., 2005). IL-17RA knockout mice exhibit reduced serum chemokine concentration and concomitantly reduced neutrophil migration to bone. IL-17 activates NF-κB and stimulates the production of several inflammatory mediators, including IL-6, IL-8, granulocyte-macrophage colony stimulating factor (GMCSF), and prostaglandin E2 (PGE2) in synoviocytes (Lubberts et al., 2005; Miossec, 2004; Stamp et al., 2004; Hwang et al., 2004). IL-17 is released mainly by memory T cells and is associated particularly with the severity of synovial inflammation of patients with RA (Cho et al., 2004; Hwang et al., 2004).
Toll-like receptors (TLRs), phylogenetically conserved receptors that recognize pathogen-associated molecular patterns, are important because of their special function in linking innate immunity to adaptive immunity (Akira et al., 2001; Takeda and Akira, 2005). TLR2 and TLR4 are expressed in inflamed RA synovium, and the expression of these receptors is associated with the presence of inflammatory cytokines (Seibl et al., 2003; Radstake et al., 2004). We recently reported that activation of TLR2 by its specific ligand mediates the upregulation of CXCL8, vascular endothelial growth factor, and IL-8 (Cho et al., 2007). We also observed that the combined engagement of TLR2 and TLR4 upregulates IL-15 in RA-FLS (Jung et al., 2007), which may contribute to the maintenance and perpetuation of synovitis in patients with RA.
We now report, for the first time, that IL-17 markedly increases the production of IL-16 and that stimulation of TLR2 by its specific ligands synergistically enhances the production of IL-16 in FLS from patients with RA.
Materials and Methods
Reagents
Antibodies to IL-1β, IL-15, IL-16, IL-17, and IFN-γ were obtained from R&D Systems (Minneapolis, MN). Peptidoglycan (PGN) and LPS were obtained from Sigma-Aldrich (St Louis, MO).
Isolation of synovial fibroblasts
FLS were isolated by enzymatic digestion of synovial tissues obtained from patients with RA undergoing total joint replacement surgery.
Isolation of peripheral blood mononuclear cells
Peripheral blood mononuclear cells (PBMC) were prepared from heparinized blood by Ficoll-Hypaque (SG1077) density gradient centrifugation
Hematoxylin and eosin staining
The tissue slides were prepared as described below, deparaffinized with three changes of xylene of 5 min each, rehydrated in a graded series of ethanol (100-70%), and washed in tap water. The sections were stained with hematoxylin for 5 min and washed in running tap water for 5 min. Tissue slides were counterstained with eosin for 15 s to 2 min, depending on the age of the eosin and the depth of the counterstaining desired. The slides were dehydrated in 95% and 100% alcohol with two changes of 2 min each or until the excess eosin was removed. Slides were treated with xylene (two changes of 2 min each) and mounted in permount or balsam.
Immunohistochemistry of synovial tissues
Immunohistochemical staining for IL-16 was performed with sections of synovium. Briefly, synovium was obtained from patients with RA or OA, fixed with 4% paraformaldehyde solution overnight at 4℃, dehydrated with alcohol, washed, embedded in paraffin, and sectioned into slices 7 µm thick. Sections were depleted of endogenous peroxidase activity by adding methanolic H2O2 and blocked with normal serum for 30 min. The sections were incubated overnight at 4℃ with polyclonal anti-human IL-16 antibody (R&D Systems); incubated with the secondary antibody, biotinylated anti-rabbit IgG, for 20 min; incubated with streptavidin-peroxidase complex (Vector, Peterborough, UK) for 1 h; and incubated with 3,3'-diaminobenzidine (Dako, Glostrup, Denmark) for 5 min. The sections were counterstained with hematoxylin. Samples were photographed with an Olympus photomicroscope (Tokyo, Japan).
Expression of IL-16 mRNA determined by RT-PCR and real-time PCR
mRNA was extracted using RNAzol B (Biotex Laboratories, Houston, TX) according to the manufacturer's instructions. Reverse transcription of 2 µg aliquots of total mRNA was carried out at 42℃ using the Superscript reverse transcription system (TaKaRa, Shiga, Japan). PCR amplification of cDNA aliquots was performed by adding 2.5 µM dNTPs, 2.5 U Taq DNA polymerase (TaKaRa), and 0.25 µM of sense and antisense primers. The following sense and antisense primers for each molecule were used (5'→3'): IL-16, 5'-ATGCCTGACCTCAACTCCACT (sense) and 5'-GCCACCCAGCTGCAAGATTTC (antisense); and GAPDH, 5'-CGATGCTGGGCGTGAGTAC (sense) and 5'-CGTTCAGCTCAGGGATGACC (antisense). Reactions were processed in a DNA thermal cycler (PerkinElmer Cetus, Wellesley, MA) through 35 cycles at 94℃ for 30 s, at 58℃ for 30 s, and at 72℃ for 30 s for IL-16; and 25 cycles at 94℃ for 30 s, at 56℃ for 30 s, and at 72℃ for 30 s for GAPDH.
The expression of IL-16 mRNAs was determined by real-time PCR with SYBR Green I. For quantitative analysis of IL-16 mRNAs, a LightCycler (Roche Diagnostics Mannheim, Germany) was used. The relative expression levels in the samples were calculated from the IL-16 levels normalized to the endogenously expressed housekeeping gene (GAPDH). Melting curve analysis was performed immediately after the amplification protocol under the following conditions: 0 s (hold time) at 95℃, 15 s at 65℃, and 0 s (hold time) at 95℃. The rate of temperature change was 20℃/s, except in the final step, in which it was 0.1℃/s. The crossing point (Cp) was defined as the maximum of the second derivative from the fluorescence curve.
Western blot analysis
FLS were incubated with 1-10 ng/ml of IL-17 for 48 h, and whole-cell lysates were prepared from about 2 × 105 cells by homogenization in the lysis buffer and centrifuged at 14,000 rpm for 15 min. The protein concentration in the supernatant was determined using the Bradford method (Bio-Rad, Hercules, CA). Protein samples were separated on 10% SDS-PAGE, and transferred to a nitrocellulose membrane (Amersham Pharmacia Biotech, Uppsala, Sweden). For western hybridization, the membrane was preincubated with 0.5% skim milk in TTBS buffer (0.1% Tween 20 in Tris-buffered saline) at room temperature for 2 h. The primary antibody to IL-16 (R&D Systems) or β-actin, diluted 1 : 1,000 in 5% BSA-0.1% Tween-20-TBS, was added and incubated for overnight at 4℃. The membrane was washed four times with TTBS, and HRP-conjugated secondary antibody was added and incubated for 1 h at room temperature. After TTBS washing, hybridized bands were detected using the ECL detection kit and Hyperfilm-ECL reagents (Amersham Pharmacia).
Statistical analysis
Data are expressed as the mean ± SD. The data were compared between pairs of groups using Student's t test for independent samples and Student's paired t test for matched pairs. Correlation coefficients were determined using Spearman's rank correlation test.
Results
Expression of IL-16 in RA synovium
IL-16 expression in joint tissue sections of RA patients was assessed by staining with anti-IL-16 monoclonal antibody or with irrelevant primary isotype-specific antibodies as a negative control. OA synovium was examined as a related control. Immunohistochemical staining revealed pronounced expression of IL-16 in the synovial lining, the sublining, and the perivascular region of the RA synovium, and at sites of lymphocyte infiltration. In contrast, minimal IL-16 staining was observed in OA synovium (Figure 1).
Increased expression of IL-16 by IL-17 stimulation and additive upregulation by TLR2 stimulation
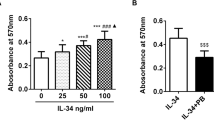
FLS obtained from four patients with RA and four patients with OA were evaluated for mRNA expression by semiquantitative RT-PCR (Figure 2A) and real-time PCR (Figure 2B). Basal gene expression of IL-16 was stronger in RA-FLS than in OA-FLS (Figure 2A). In one representative sample of RAFLS, IL-16 mRNA expression was strongly induced after incubation with IL-17 (20 ng/ml). However, IL-15 (10 ng/ml), IL-1β (10 ng/ml), or IFN-γ (10 ng/ml) did not affect the expression of IL-16 mRNA (Figure 2A). The mRNA expression of IL-16 relative to GAPDH was higher when FLS were cultured with IL-17 than when cultured with IL-15, IL-1β, or IFN-γ (Figure 2B). The mRNA expression of IL-16 by RA-FLS (n = 4) was strongly upregulated by IL-17 in a dose-dependent manner. The expression of IL-16 mRNA was evaluated by RT-PCR (Figure 3A and B) and realtime PCR (Figure 3C and D). Compared with untreated cells, relative mRNA expression of IL-16/GAPDH was: for 1 ng/ml of IL-17, 2.1 ± 0.5; for 10 ng/ml of IL-17, 6.0 ± 1.1; and for 20 ng/ml of IL-17, 13 ± 2.1. *P < 0.05, **P < 0.01 (Figure 3A).
IL-16 mRNA expression is upregulated by IL-17 stimulation in RA-FLS, but not in OA-FLS. (A) IL-16 mRNA expression induced by IL-17 in RA-FLS. FLS were cultured with cytokines (IL-15, IL-1β IFN-γ or IL-17) for 12 h. The expression of IL-16 mRNA was evaluated by RT-PCR. The optical density was normalized to the band for GAPDH. (B) The expression of IL-16 mRNA was evaluated by real-time PCR. **P < 0.01 compared with Nil (untreated control cells).
IL-16 mRNA expression in RA-FLS and RA-PBMC is upregulated by IL-17 in a dose-dependent manner. (A, B) IL-16 mRNA expression was induced by IL-17 in RA-PBMC. FLS were cultured with IL-17 (1-20 ng/ml) for 12 h. RA-PBMC were cultured with IL-17 (1-20 ng/ml), IFN-γ (10 ng/ml), or IL-1β (10 ng/ml) for 12 h. The expression of IL-16 mRNA was evaluated by RT-PCR. The optical density was normalized to the band for GAPDH. (C, D) The expression of IL-16 mRNA was evaluated by real-time PCR. *P < 0.05, **P < 0.01 compared with Nil (untreated control cells).
The relative mRNA expression of IL-16 by PBMC from five patients with RA (n = 5) was also upregulated by IL-17 in a dose-dependent manner. Compared with untreated cells, relative mRNA expression of IL-16/GAPDH was: for 1 ng/ml of IL-17, 1.5 ± 0.3; for 10 ng/ml of IL-17, 2.7 ± 0.5; for 20 ng/ml of IL-17, 6 ± 1.1. *P < 0.05, **P < 0.01 (Figure 3B). IFN-γ did not increase the expression of IL-16 in RA-FLS (data not shown) or RA-PBMC, but IL-1β increased the expression of IL-16 in RA-PBMC (2.5 ± 0.5 compared with untreated cells) (*P < 0.05). The representative samples of RA-FLS and RA-PBMC show a dose-dependent increase in IL-16 mRNA expression after incubation with IL-17 (Figure 3). The dose-dependent increase in the expression of IL-16 stimulated by IL-17 was assessed with western blot analysis (Figure 4).
IL-16 protein expression increased significantly with treatment by IL-17. RA-FLS were cultured with or without IL-17 (1-10 ng/ml) for 48 h. IL-16 protein expression was measured in cell lysates by western blot analysis using goat polyclonal anti-IL-16 antibody. Results are expressed as the ratio of the densitometric intensity of the IL-16 product to that of the β-actin product. The data represent one of three independent experiments.
The production of IL-16 by RA-FLS (n = 6) was strongly upregulated by PGN in a dose-dependent manner (1 µg/ml PGN, 3 ± 0.5; 10 µg/ml PGN, 7.9 ± 1.1 µg/ml compared with untreated FLS) (*P < 0.05, **P < 0.01, each dose compared with untreated FLS) (Figure 5). The augmented production of IL-15 in response to TLR2 stimulation was regulated at the mRNA level. IL-16 gene expression did not change in response to LPS. The stimulatory effect of IL-17 on IL-16 production was augmented by PGN in a dose-dependent manner (FLS treated with 10 ng/ml IL-17 only, 6 ± 1.21 µg/ml; PGN + 10 ng/ml IL-17, 13 ± 2.5; 10 µg/ml PGN + 10 ng/ml IL-17, 17 ± 2.7 compared with untreated cells) (#P < 0.05, ##P < 0.01) (Figure 5).
Increased IL-16 mRNA expression by IL-17 stimulation and additive upregulation by TLR2 stimulation. Expression of IL-16 was induced by IL-17, PGN (a TLR2 ligand), LPS (a TLR4 ligand), IL-17 + PGN or IL-17 + LPS. FLS were cultured with IL-17 (10 ng/ml), PGN (1-10 ng/ml), LPS (10-100 ng/ml), IL-17 + PGN, or IL-17 + LPS for 12 h. PGN (0.1-10 ng/ml), LPS (10-1000 ng/ml), or PGN (1 µg/ml) plus LPS (10-1000 ng/ml) for 12 h. The expression of IL-16 mRNA was evaluated by real-time PCR. *P < 0.05, **P < 0.01 compared with Nil (untreated control cells). ##P < 0.01 compared with IL-17 stimulation.
Discussion
We observed the spontaneous expression of IL-16 in synovial tissues from RA patients, but not in tissues from OA patients. This result agrees with previous reports (Franz et al., 1998; Sciaky et al., 2000 Weis-Klemm et al., 2004). However, the stimuli that contribute to induce IL-16 in RA-FLS have been reported rarely. In our experiment, IL-17 and the specific ligand of TLR2 showed to be the major stimuli that induced IL-16 expression and production in RA-FLS.
IL-17 is a 17 kDa protein that is secreted predominantly by human memory T cells or mouse αβTCR+CD4-CD8- thymocytes (Yao et al., 1995; Kennedy et al., 1996). IL-17 is produced spontaneously in the RA synovium, and a high concentration of IL-17 is detected in the synovial fluid of patients with RA (Chabaud et al., 1999; Kotake et al., 1999). In synergy with other proinflammatory cytokines such as IL-1β, TNF-α, and IFN-γ, IL-17 provokes local inflammation and amplification of inflammatory responses (Ruddy et al., 2004; Albanesi et al., 1999; Witowski et al., 2000). IL-17 also mediates chemotaxis of neutrophils and monocytes by inducing chemoattractant molecules such as IL-8, monocyte chemoattractant protein-1 (MCP-1), and growth-related protein-α (Witowski et al., 2000; Afzali et al., 2007). We observed that IL-17 but not other proinflammatory cytokines stimulated the production of IL-16. Weis-Klemm et al. (2004) reported that IL-1β or TNF-α do not upregulate IL-16 mRNA in FLS in RA patients. In contrast, an experiment using human orbital fibroblasts showed that IL-1β increases IL-16 synthesis (Sciaky et al., 2000). We observed a partial stimulatory effect of IL-1β on IL-16 in RA-PBMC, but not in RA-FLS. We postulate that the effects of cytokines on IL-16 production differ between cell types. Our results suggest that the upregulation of IL-16 is another important function of IL-17 in RA-FLS along with its various proinflammatory roles. In addition, the stimulatory effect of IL-17 on IL-16 was observed specifically in RA-FLS, but not in OA-FLS.
TLRs are key receptors responsible for the recognition of bacterial components such as LPS, cytosine phosphate guanine (CpG) DNA, andendogenous ligands. TLR2 has been identified as a receptor for gram-positive bacterial cell wall proteins, such as PGN and bacterial lipopeptide (Underhill et al., 1999; Brightbill et al., 1999). TLR4 interacts with LPS (Zhang et al., 1999) and with endogenous ligands such as heat-shock proteins (Ohashi et al., 2000), fragments of hyaluronic acid (Termeer et al., 2002), and fibronectin (Okamura et al., 2001). As mentioned above, TLR expression increases in the rheumatoid synovium where it participates in the perpetuation of synovial inflammation. Our previous work demonstrated that activation of TLRs by their specific ligands could induce the production of chemokines or proinflammatory cytokines in RA-FLS (Cho et al., 2007; Jung et al., 2007). Those findings prompted us to test the potential role of TLR activation in the provocation of IL-16. We identified a stimulatory effect of the TLR2 ligand on IL-16 production in RA-FLS. In contrast, activation of TLR4 did not influence IL-16 expression. We also observed additive effect of PGN and IL-17 on IL-16 production.
IL-16 is detected in a number of inflammatory processes and acts as a potent chemoattractant for all peripheral immune cells expressing CD4, including CD4+ monocytes (Cruikshank et al., 1987), eosinophils (Rand et al., 1991), and dendritic cells (Kaser et al., 1999). There are conflicting data about the roles of IL-16 in inflammatory conditions. Animal studies have reported that IL-16 is an immunomodulatory mediator and that administration of IL-16 in a murine model of RA decreases the production of IFN-γ, IL-1β and TNF-α (Cruikshank et al., 1996; Klimiuk et al., 1999). Blaschke et al. (2001) reported no significant association between serum and synovial fluid IL-16 concentration and synovial tissue expression of IL-16 and clinical disease activity in patients with RA. In contrast, IL-16 contributes to airway inflammation in bronchial asthma (Cruikshank et al., 1995) and to granulomatous inflammation (Wu et al., 1999). IL-16 stimulates the expression and production of proinflammatory cytokines such as TNF-α, IL-1β and IL-6 in human PBMC (Mathy et al., 2000). In RA, the induced IL-16 may play a role in the perpetuation of synovitis by recruiting inflammatory cells, includeing T cells, into synovial tissues, although the exact role of IL-16 in RA pathogenesis needs to be investigated further.
The results in this paper demonstrate that IL-17 and activation of TLR2 increase the production of IL-16 in RA-FLS. Although the intracellular signaling cascades through which IL-17 or TLR2 ligand provoke the production of IL-16 in RA-FLS have not been defined, this finding may provide future molecular targets to treat patients with RA.
Abbreviations
- FLS:
-
fibroblast-like synoviocytes
- GMCSF:
-
granulocyte-macrophage colony stimulating factor
- OA:
-
osteoarthritis
- PBMC:
-
Peripheral blood mononuclear cells
- PGE2:
-
Prostaglandin E2
- RA:
-
rheumatoid arthritis
- TLRs:
-
Toll-like receptor
References
Afzali B, Lombardi G, Lechler RI, Lord GM . The role of T helper 17 (Th17) and regulatory T cells (Treg) in human organ transplantation and autoimmune disease . Clin Exp Immunol 2007 ; 148 : 32 - 46
Akira S, Takeda K, Kaisho T . Toll-like receptors: critical proteins linking innate and acquired immunity . Nat Immunol 2001 ; 2 : 675 - 680
Albanesi C, Cavani A, Girolomoni G . IL-17 is produced by nickel-specific T lymphocytes and regulates ICAM-1 expression and chemokine production in human keratinocytes: synergistic or antagonist effects with IFN-gamma and TNF-alpha . J Immunol 1999 ; 162 : 494 - 502
Blaschke S, Schulze H, Schwartz G, Blaschke V, Müller GA, Reuss-Borst M . Interleukin 16 expression in relation to disease activity in rheumatoid arthritis . J Rheumatol 2001 ; 28 : 12 - 21
Brightbill HD, Libraty DH, Krutzik SR, Yang RB, Belisle JT, Bleharski JR, Maitland M, Norgard MV, Plevy SE, Smale ST, Brennan PJ, Bloom BR, Godowski PJ, Modlin RL . Host defense mechanisms triggered by microbial lipoproteins through toll-like receptors . Science 1999 ; 285 : 732 - 736
Center DM, Kornfeld H, Cruikshank WW . Interleukin-16 . Int J Biochem Cell Biol 1997 ; 29 : 1231 - 1234
Chabaud M, Durand JM, Buchs N, Fossiez F, Page G, Frappart L, Miossec P . Human interleukin-17: a T cell-derived proinflammatory cytokine produced by the rheumatoid synovium . Arthritis Rheum 1999 ; 42 : 963 - 970
Cho ML, Yoon CH, Hwang SY, Park MK, Min SY, Lee SH, Park SH, Kim HY . Effector function of type II collagen-stimulated T cells from rheumatoid arthritis patients: cross-talk between T cells and synovial fibroblasts . Arthritis Rheum 2004 ; 50 : 776 - 784
Cho ML, Ju JH, Kim HR, Oh HJ, Kang CM, Jhun JY, Lee SY, Park MK, Min JK, Park SH, Lee SH, Kim HY . Toll-like receptor 2 ligand mediates the upregulation of angiogenic factor, vascular endothelial growth factor and interleukin-8/CXCL8 in human rheumatoid synovial fibroblasts . Immunol Lett 2007 ; 108 : 121 - 128
Cruikshank WW, Berman JS, Theodore AC, Bernardo J, Center DM . Lymphokine activation of T4 lymphocytes and monocytes . J Immunol 1987 ; 138 : 3817 - 3823
Cruikshank WW, Long A, Tarpy RE, Kornfeld H, Carroll MP, Teran L, Holgate ST, Center DM . Early identification of IL-16 (lymphocyte chemoattractant factor) and macrophage inflammatory protein 1α (MIP1α) in bronchoalveolar lavage fluid of antigen challenged asthmatics . Am J Respir Cell Mol Biol 1995 ; 13 : 738 - 747
Cruikshank WW, Lim K, Theodore AC, Cook J, Fine G, Weller PF, Center DM . IL-16 inhibition of CD3-dependent lymphocyte activation and proliferation . J Immunol 1996 ; 157 : 5240 - 5248
Cruikshank WW, Kornfeld H, Center DM . Interlekin-16 . J Leukoc Biol 2000 ; 67 : 757 - 766
Franz JK, Kolb SA, Hummel KM, Lahrtz F, Neidhart M, Aicher WK, Pap T, Gay RE, Fontana A, Gay S . Interleukin-16, produced by synovial fibroblasts, mediates chemoattraction for CD4+ T lymphocytes in rheumatoid arthritis . Eur J Immunol 1998 ; 28 : 2661 - 2671
Hwang SY, Kim JY, Kim KW, Park MK, Moon YM, Kim WU . IL-17 induces production of IL-6 and IL-8 in rheumatoid arthritis synovial fibroblasts via NF-kappaB-and PI3-kinase/Akt-dependent pathways . Arthritis Res Ther 2004 ; 6 : R120 - R128
Jung YO, Cho ML, Kang CM, Jhun JY, Park JS, Oh HJ, Min JK, Park SH, Kim HY . Toll-like receptor 2 and 4 combination engagement upregulate IL-15 synergistically in human rheumatoid synovial fibroblasts . Immunol Lett 2007 ; 109 : 21 - 27
Kaser A, Dunzendorfer S, Offner FA, Ryan T, Schwabegger A, Cruikshank WW, Wiedermann CJ, Tilg H . A role for IL-16 in the cross-talk between dendritic cells and T cells . J Immunol 1999 ; 163 : 3232 - 3238
Kennedy J, Rossi DL, Zurawski SM, Vega F, Kastelein RA, Wagner JL, Hannum CH, Zlotnik A . Mouse IL-17: a cytokine preferentially expressed by αβTCR+CD4-CD8-T cells . J Interferon Cytokine Res 1996 ; 16 : 611 - 617
Klimiuk PA, Goronzy JJ, Weyand CM . IL-16 as an anti-inflammatory cytokine in rheumatoid synovitis . J Immunol 1999 ; 162 : 4293 - 4299
Koch AE . Angiogenesis: implications for rheumatoid arthritis . Arthritis Rheum 1998 ; 41 : 951 - 962
Kotake S, Udagawa M, Takahashi N, Matsuzaki K, Itoh K, Ishiyama S . IL-17 in synovial fluids from patients with rheumatoid arthritis is a potent stimulator of osteoclastogenesis . J Clin Invest 1999 ; 103 : 1345 - 1352
Lubberts E, Koenders M, van den Berg WB . The role of T cells interleukin-17 in conducting destructive arthritis: lessons from animal models . Arthritis Res Ther 2005 ; 7 : 29 - 37
Mathy NL, Scheuer W, Lanzendorfer M, Honold K, Ambrosius D, Norley S, Kurth R . Interleukin-16 stimulates the expression and production of pro-inflammatory cytokines by human monocytes . Immunology 2000 ; 100 : 63 - 69
Miossec P . An update on the cytokine network in rheumatoid arthritis . Curr Opin Rheumatol 2004 ; 16 : 218 - 222
Ohashi K, Burkart V, Flohe S, Kolb H . Cutting edge: heat shock protein 60 is a putative endogenous ligand of the Toll-like receptor-4 complex . J Immunol 2000 ; 164 : 558 - 561
Okamura Y, Watari M, Jerud ES, Young DW, Ishizaka ST, Rose J, Chow JC, Strauss JF . The extra domain A of fibronectin activates Toll-like receptor 4 . J Biol Chem 2001 ; 276 : 10229 - 10233
Pritchard J, Tsui S, Horst N, William W, Cruikshank, Smith TJ . Synovial fibroblasts from patients with rheumatoid arthritis, like fibroblasts from Graves' disease, express high levels of IL-16 when treated with Igs against insulin-like growth factor-1 receptor . J Immunol 2004 ; 173 : 3564 - 3569
Radstake TR, Roelofs MF, Jenniskens YM, Oppers-Walgreen B, van Riel PL, Barrera P, Joosten LA, van den Berg WB . Expression of toll-like receptors 2 and 4 in rheumatoid synovial tissue and regulation by proinflammatorycytokine interleukin-12 and interleukin-18 via interferon-γ . Arthritis Rheum 2004 ; 50 : 3856 - 3865
Rand T, Cruikshank WW, Center DM, Weller PF . CD4-mediated stimulation of human eosinophil: lymphocyte chemoattractant factor and other CD4-binding ligands elicit eosinophil migration . J Exp Med 1991 ; 173 : 1521 - 1528
Ruddy MJ, Wong GC, Liu XK, Yamamoto H, Kasayama S, Kirkwood KL, Gaffen SL . Functional cooperation between interleukin-17 and tumor necrosis factor-α is mediated by CAAT/enhancer-binding protein family members . J Biol Chem 2004 ; 279 : 2559 - 2567
Sciaky D, Brazer W, Center DM, William W, Cruikshank, Smith TJ . Cultured human fibroblasts express constitutive IL-16 mRNA: cytokine induction of active IL-16 protein synthesis through a caspase-3-dependent mechanism . J Immunol 2000 ; 164 : 3806 - 3814
Seibl R, Birchler T, Loeliger S, Hossle JP, Gay RE, Saurenmann T, Michel BA, Seger RA, Gay S, Lauener RP . Expression and regulation of toll-like receptor 2 in rheumatoid arthritis synovium . Am J Pathol 2003 ; 162 : 1221 - 1227
Stamp LK, Cleland LF, James MJ . Upregulation of synoviocyte COX-2 through interactions with T lymphocytes: role of IL-17 and tumor necrosis factor-α . J Rheumatol 2004 ; 31 : 1255 - 1264
Takeda K, Akira S . Toll-like receptors in innate immunity . Int Immunol 2005 ; 17 : 1 - 14
Termeer C, Benedix F, Sleeman J, Fieber C, Voith U, Alurens T . Oligosaccharides of hyaluronan activate dendritic cells via Toll-like receptor 4 . J Exp Med 2002 ; 195 : 99 - 111
Underhill DM, Ozinsky A, Smith KD, Aderem A . Toll-like receptor-2 mediates mycobacteria-induced proinflammatory signaling in macrophages . Proc Natl Acad Sci USA 1999 ; 96 : 14459 - 14463
Weis-Klemm M, Alexander D, Pap T, Schutzle H, Reyer D, Franz JK, Aicher WK . Synovial fibroblasts from rheumatoid arthritis patients differ in their regulation of IL-16 gene activity in comparison to osteoarthritis fibroblasts . Cell Physiol Biochem 2004 ; 14 : 293 - 300
Weyand CM, Goronzy JJ . Pathogenesis of rheumatoid arthritis . Med Clin North Am 1997 ; 81 : 29 - 55
Witowski J, Pawlaczyk K, Breborowicz A, Scheuren A, Kuzlan-Pawlaczyk M, Wisniewska J, Polubinska A, Friess H, Gahl GM, Frei U, Jorres A . IL-17 stimulates intraperitoneal neutrophil infiltration through the release of GRO alpha chemokine from mesothelial cells . J Immunol 2000 ; 165 : 5814 - 5821
Wu DM, Zhang Y, Parada MA, Kornfeld H, Nicoll J, Center DM . Processing and release of interleukin-16 from CD4+ but not CD8+ T cells is activation dependent . J Immunol 1999 ; 162 : 1287 - 1293
Yao Z, Painter SL, Fanslow WC, Ulrich D, Macduff BM, Spriggs MK, Armitage RJ . Human IL-17: a novel cytokine described from T cells . J Immunol 1995 ; 155 : 5483 - 5486
Zhang FX, Kirschning CJ, Mancinelli R, Xu XP, Jin Y, Faure E, Mantovani A, Rothe M, Muzio M, Arditi M . Bacterial lipopolysaccharide activates nuclear factor-κB through interleukin-1 signalling mediators in cultured human dermal endothelial cells and mononuclear phagocytes . J Biol Chem 1999 ; 274 : 7611 - 7614
Acknowledgements
This work was supported by grant No. R11-2002-098-05003-0 from the Korea Science and Engineering Foundation through the Rheumatism Research Center at Catholic University of Korea and the Korea Research Foundation Grant funded by the Korean Government (MOEHRD, Basic Research Promotion Fund) (KRF-2006-331-E00107).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Cho, ML., Jung, Y., Kim, KW. et al. IL-17 induces the production of IL-16 in rheumatoid arthritis. Exp Mol Med 40, 237–245 (2008). https://doi.org/10.3858/emm.2008.40.2.237
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.3858/emm.2008.40.2.237
Keywords
This article is cited by
-
A comprehensive profile of chemokines in the peripheral blood and vascular tissue of patients with Takayasu arteritis
Arthritis Research & Therapy (2022)
-
Association of a miRNA-binding site polymorphism in IL-16 gene with disease risk and clinical characteristics of rheumatoid arthritis and systemic lupus erythematosus
Clinical Rheumatology (2022)
-
Serum interleukin-16 significantly correlates with the Vasculitis Damage Index in antineutrophil cytoplasmic antibody-associated vasculitis
Arthritis Research & Therapy (2020)
-
PTEN ameliorates autoimmune arthritis through down-regulating STAT3 activation with reciprocal balance of Th17 and Tregs
Scientific Reports (2016)
-
HtrA2 suppresses autoimmune arthritis and regulates activation of STAT3
Scientific Reports (2016)