Abstract
In a 51-year-old patient of consanguineous parents with a severe neuromuscular phenotype of early-onset ataxia, myoclonia, dysarthria, muscle weakness and exercise intolerance, exome sequencing revealed a novel homozygous variant (c.-264_31delinsCTCACAAATGCTCA) in the mitochondrial FAD-transporter gene SLC25A32. Flavin adenine dinucleotide (FAD) is an essential co-factor for many mitochondrial enzymes and impaired mitochondrial FAD-transport was supported by a reduced oxidative phosphorylation complex II activity in the patient’s muscle, decreased ATP production in fibroblasts, and a deficiency of mitochondrial FAD-dependent enzymes. Clinically, the patient showed improvement upon riboflavin treatment, which is a precursor of FAD. Our results confirm the recently reported case of SLC25A32 as a cause of riboflavin-responsive disease. Our patient showed a more severe clinical phenotype compared with the reported patient, corresponding with the (most likely) complete absence of the SLC25A32-encoding MFT (Mitochondrial Folate Transporter) protein.
Similar content being viewed by others
Introduction
Mitochondrial disorders are among the most common inherited neuromuscular disorders and are genetically and clinically highly heterogeneous. The limited genotype–phenotype correlations and extreme genetic heterogeneity make selection of a single candidate gene impossible for the majority of patients. Whole-exome sequencing is the best strategy to identify the nuclear genetic defect for these disorders, enabling identification of known disease genes or new candidate genes. Here we identified with exome sequencing a novel homozygous SLC25A32 null variant, causing complete absence of the protein or production of a dysfunctional protein, and resulting in a patient with a severe neuromuscular phenotype. This is the second patient reported with variants in this gene, the first being a patient with exercise intolerance and biochemical features of multiple acyl-coenzyme A dehydrogenase deficiency.1
Subjects and methods
Patient
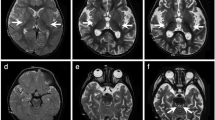
The patient of consanguineous Dutch parents (first cousins) presented at the age of 3 years with muscle weakness after he had suffered from influenza. During childhood, he showed an impaired motor development and exercise intolerance. Subsequently, around the age of 20 years, he developed progressive dysarthria. In the last 10 years, this is accompanied with swallowing difficulties. In addition, he occasionally has myoclonic jerks. He is in a wheelchair (although not continuously) now at age 52. He has 2 brothers and 6 sisters, none of them clinically affected (Supplementary Figure 1a). His blood tests showed an increased lactic acid of 5.7 mmol/l. Stainings of the patient’s muscle tissue revealed the presence of many ragged-red fibres, as well as multiple cytochrome oxidase-negative muscle fibres. Biochemical measurement of complex I, complex II+III, complex IV and citrate synthetase activities was performed in muscle tissue as described before.2 Activities of the patient’s oxidative phosphorylation (OXPHOS) complexes I, II+III and IV in muscle biopsy revealed a complex II+III activity of approximately 44% of control muscle, indicating an OXPHOS complex II deficiency. Furthermore, measurements of isolated complex II activity in muscle showed a complex II activity of 36% of control muscle. In addition, oxygen consumption rate parameters in patient-derived fibroblasts showed decreased basal respiration levels and ATP production (Supplementary Figure 2).
Whole-exome sequencing
Exome enrichment was performed by the Agilent SureSelectXT exome enrichment kit version 5 (Agilent Technologies, Santa Clara, CA, USA). Sequencing was performed by an Illumina NextSeq500 platform, using a 2 × 150 bp paired-end setting (Illumina, San Diego, CA, USA). Basecalling and demultiplexing was done using bcl2fastq 2.16.0; reads were aligned onto the human reference genome (hg19) by BWA 0.5.9; duplicates were removed using PICARD software suite 1.77 (Broad Institute, Cambridge, MA, USA); variant calling was performed using GATK 2.1-8 (Broad Institute). Annotations were added using an in-house developed annotation pipeline, which uses as resources amongst others Gencode V19, dbSNP144, ExAC v0.2, and CADD v1.3. Results were also compared to an in-house database that contains the occurrences amongst 7788 exomes. Targeted exome analyses of a panel of ~450 nuclear genes was performed, containing known mitochondrial disease genes and functionally or clinically related genes. The data were filtered for homozygous and heterozygous non-synonymous variants, insertions and deletions (both in-frame and frameshift), nonsense variants and splice-variants, with allele frequencies <0.01 in the ExAC database3 and in our in-house database. The impact of missense variants on protein function was estimated using the algorithms integrated in the Alamut software version 2.7 (Rouen, France). The pathogenic variant in SLC25A32 and the patient’s phenotype were submitted to the gene variant database www.LOVD.nl/SLC25A32 (patient ID00092292).
Results
Whole-exome sequencing was performed to identify the underlying genetic defect in the patient. Since the patient was suspected of having a mitochondrial disorder, targeted exome analyses of known mitochondrial disease genes, as well as functionally or clinically related genes, was performed. After filtering variants on allele frequency and predicted impact on protein function, only SLC25A32 contained two mutated alleles. The patient was homozygous for the SLC25A32 c.-264_31delinsCTCACAAATGCTCA variant (NM_030780.4), a novel variant that is not present in any of the SNP-databases and not reported before in patients. The presence of the variant was confirmed by Sanger sequencing in the index patient, whereas the variant was not detected in an unaffected brother (Supplementary Figure 1a). Other siblings, as well as the patient’s parents, were not available for testing.
The c.-264_31delinsCTCACAAATGCTCA variant deletes the methionine (AUG) translation start codon (Supplementary Figure 1b), resulting in complete absence of the MFT protein or, alternatively, production of a dysfunctional protein due to the use of a downstream translation start codon. The second AUG-codon in the SLC25A32 gene is located in exon 4, however, this is not in the context of a Kozak consensus sequence required for translation initiation.4 It is therefore most likely that the homozygous variant in our patient causes complete loss of the MFT protein.
MFT is a mitochondrial transporter of flavin adenine dinucleotide (FAD), a co-factor required for many mitochondrial enzymes. A causal role for the SLC25A32 variant in the patient’s clinical and biochemical phenotype was therefore confirmed by the reduced activity of OXPHOS complex II, containing FAD-dependent succinate dehydrogenase (SDH), in the patient’s muscle. Further support for the link between the SLC25A32 gene and the patient’s phenotype was obtained from metabolic investigations (Table 1). Analysis of urinary organic acids revealed strongly increased excretion of isovalerylglycine, isobutyrylglycine and ethylmalonic acid, and acylcarnitine profiling in plasma showed increased levels of (iso)butyryl-, isovaleryl-, hexanoyl-, octanoyl-, decenoyl-, decanoyl- and glutaryl- carnitine esters. These metabolic results indicate decreased activities of multiple acyl-coenzyme A dehydrogenases in the patient, corresponding with a dysfunctional FAD-transport.
After identification of the damaging variant in the SLC25A32 gene, encoding the mitochondrial FAD-transporter (MFT), as the causal genetic defect in the patient, oral supplementation with riboflavin at a dose of 10 mg three times a day was started. This showed improvement in the patient’s clinical condition: Before starting the riboflavin treatment, he was able to walk a maximum distance of 100 m. One and a half month after starting riboflavin supplementation, the patient could walk at least 500 m. His endurance was increased, without a change in muscle strength.
Discussion
Using whole-exome sequencing, we identified a novel homozygous variant in the SLC25A32 FAD-transporter gene causing a severe neuromuscular phenotype in a consanguineous Dutch family. The SLC25A32 c.-264_31delinsCTCACAAATGCTCA variant completely abolishes the translation start codon and it is therefore highly likely that the protein is either completely absent or dysfunctional, when an alternative start codon would be used. On the basis of this, we concluded that no functional MFT protein could be formed, and therefore we did not perform follow-up experiments. Because the patient’s parents were not available for testing, the ‘apparently’ homozygous SLC25A32 variant can theoretically be hemizygous, due to a large deletion of one allele, which can not be detected by both sequencing methods used (exome sequencing and Sanger sequencing). Nevertheless, the consanguinity of the parents (first cousins) and the large homozygous region (LOH region) in which the variant is located, as shown in the exome data (data not shown), make homozygosity of the SLC25A32 variant in the patient highly likely.
Only one other, recently reported patient has been described with SLC25A32 variants.1 Remarkably, in comparison with the reported patient with late-onset exercise intolerance, our patient suffers from more severe, heterogeneous symptoms, involving early-onset ataxia, myoclonia, dysarthria, muscle weakness and exercise intolerance. The severe neuromuscular phenotype of our patient is probably explained by the type of variant resulting (very likely) in complete absence of the MFT protein, while the reported SLC25A32-patient with a milder phenotype is compound heterozygous for a nonsense and a missense variant.
MFT is a member of the large family of SLC25 solute carrier.5 Embedded in the inner mitochondrial membrane, MFT transports flavin adenine dinucleotide (FAD) from the cytosol into the mitochondria.6 The presence of mitochondrial FAD is necessary for many mitochondrial enzymes, including succinate dehydrogenase (SDH) and multiple acyl-coenzyme A dehydrogenases. Therefore, reduced mitochondrial FAD levels results in, amongst others, decreased mitochondrial β-oxidation and oxidative phosphorylation. Supplementation with the FAD precursor riboflavin, or vitamin B2, raises the intra-mitochondrial FAD concentration, which might compensate for the decreased FAD binding of enzymes.7 This is reflected by the clinical improvement of our patient upon riboflavin treatment.
In conclusion, we report the second patient with damaging variants in the SLC25A32 gene as a novel cause of riboflavin-responsive neuromuscular disease. Our data show that SLC25A32 variants can manifest clinically quite divers. SLC25A32 should be added to the list of candidate genes for patients with neuromuscular symptoms suspected of having a mitochondrial disorder, especially in case of a biochemical phenotype of FAD deficiency.
References
Schiff M, Veauville-Merllié A, Su CH et al: SLC25A32 mutations and riboflavin-responsive exercise intolerance. N Engl J Med 2016; 374: 795–797.
Sgobbo P, Pacelli C, Grattagliano I, Villani G, Cocco T : Carvedilol inhibits mitochondrial complex I and induces resistance to H2O2 -mediated oxidative insult in H9C2 myocardial cells. Biochim Biophys Acta 2007; 1767: 222–232.
Lek M, Karczewski KJ, Minikel EV et al: Analysis of protein-coding genetic variation in 60706 humans. Nature 2016; 536: 285–291.
Kozak M : Point mutations define a sequence flanking the AUG initiator codon that modulates translation by eukaryotic ribosomes. Cell 1986; 44: 283–292.
Palmieri F : The mitochondrial transporter family SLC25: identification, properties and physiopathology. Mol Aspects Med 2013; 34: 465–484.
Spaan AN, Ijlst L, van Roermund CW et al: Identification of the human mitochondrial FAD transporter and its potential role in multiple acyl-CoA dehydrogenase deficiency. Mol Genet Metab 2005; 86: 441–447.
Henriques BJ, Lucas TG, Gomes CM et al: Therapeutic approaches using riboflavin in mitochondrial energy metabolism disorders. Curr Drug Targets 2016; 17: 1527–1534.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on European Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Hellebrekers, D., Sallevelt, S., Theunissen, T. et al. Novel SLC25A32 mutation in a patient with a severe neuromuscular phenotype. Eur J Hum Genet 25, 886–888 (2017). https://doi.org/10.1038/ejhg.2017.62
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2017.62
This article is cited by
-
New insights into the nutritional genomics of adult-onset riboflavin-responsive diseases
Nutrition & Metabolism (2023)
-
Combinatorial GxGxE CRISPR screen identifies SLC25A39 in mitochondrial glutathione transport linking iron homeostasis to OXPHOS
Nature Communications (2022)
-
Hypoketotic hypoglycemia without neuromuscular complications in patients with SLC25A32 deficiency
European Journal of Human Genetics (2022)
-
Mitochondrial FAD shortage in SLC25A32 deficiency affects folate-mediated one-carbon metabolism
Cellular and Molecular Life Sciences (2022)