Abstract
Identifying germline BRCA pathogenic mutations in patients with ovarian or breast cancer is a crucial component in the medical management of affected patients. Furthermore, the relatives of affected patients can be offered genetic testing. Relatives who test positive for a germline BRCA pathogenic mutation can take appropriate action to prevent cancer or have cancer diagnosed as early as possible for better treatment options. The recent discovery that BRCA pathogenic mutation status can inform treatment decisions in patients with ovarian cancer has led to an increased demand for BRCA testing, with testing taking place earlier in the patient care pathway. New approaches to genetic counselling may be required to meet this greater demand for BRCA testing. This review discusses the need for best practices for genetic counselling and BRCA testing; it examines the challenges facing current practice and looks at adapted models of genetic counselling.
Similar content being viewed by others
Introduction
It is well established that individuals carrying a germline BRCA1 or BRCA2 pathogenic mutation have an elevated lifetime risk of developing ovarian cancer (40% and 18% by age of 70 years for BRCA1 and BRCA2, respectively) or breast cancer (57% and 49% by age of 70 years for BRCA1 and BRCA2, respectively).1 Prospective cancer-risk data from the EMBRACE study in the UK show similar numbers; average cumulative risk of ovarian cancer by age of 70 years in BRCA1 and BRCA2 pathogenic mutation carriers is 59% and 17%, respectively; and 60% and 55%, respectively, for breast cancer.2 Although guidelines differ between countries and regions, genetic testing is used predominantly to determine the BRCA pathogenic mutation status and assess the cancer risk in patients with a high probability of an inherited predisposition, which is currently based in particular on a family history for breast and ovarian cancer or, for instance, Jewish ancestry.3, 4, 5, 6 Pathogenic mutation carriers are offered regular surveillance and/or prophylactic mastectomies or prophylactic salpingo-oophorectomies, which have been shown to reduce the risk of developing cancer.7, 8
In view of the elevated lifetime risk of developing ovarian or breast cancer associated with germline BRCA pathogenic mutations, it is important that relatives of those patients who developed ovarian or breast cancer because of a germline BRCA pathogenic mutation are offered germline BRCA testing. Those relatives who are confirmed as carrying a germline BRCA pathogenic mutation can then take appropriate action in order to prevent cancer or have cancer diagnosed as early as possible for better treatment options.
Recent studies have reported that patients with ovarian cancer who carry a BRCA pathogenic mutation have longer survival rates, a favourable response to platinum-based chemotherapy and may demonstrate sensitivity to novel treatments such as inhibitors of poly(ADP)-ribose polymerase (PARP), which target the DNA repair pathway that is defective in the tumour cells of carriers.9, 10, 11, 12 By focussing on family history while selecting patients eligible for BRCA testing, 15–44% of women with ovarian cancer, who are BRCA pathogenic mutation carriers but appear to have no family risk factors, are missed.9, 13, 14, 15, 16 With the prospect of targeted treatment options on the horizon and the high prevalence of BRCA pathogenic mutations among patients with ovarian cancer, there is a case for expanding genetic testing to all women with ovarian cancer regardless of family history and to screen not only for germline BRCA pathogenic mutations in this setting but also for somatic BRCA pathogenic mutations.9, 17
BRCA testing guidelines vary considerably between countries, but there is an evolving trend to look beyond family cancer history. For instance, the National Comprehensive Cancer Network, the American Congress of Obstetricians and Gynecologists and the revised Dutch guidelines recommend BRCA genetic testing for patients with ovarian cancer, irrespective of family history, and the Scottish Intercollegiate Guidelines Network guideline 135 recommends offering BRCA genetic testing to all women with non-mucinous ovarian cancer or fallopian tube cancer, irrespective of family history; however, other guidelines, including the European Society for Medical Oncology clinical practice guidelines and some country-specific guidelines, rely on family history of breast cancer and/or ovarian cancer.4, 5, 6, 18, 19
Undeniably, this increase in demand for BRCA testing will have an impact on the current genetic testing process. Current practice in many countries requires face-to-face counselling with a qualified genetic counsellor or a clinical geneticist both before and afer BRCA testing.3, 5 One could argue that there will be a need for more genetic professionals in order to cope with increasing demands, but new approaches for delivering genetic counselling can also be explored.
This review gives an overview of alternative procedures for genetic counselling and testing of patients at risk of hereditary breast and ovarian cancer, with a focus on patients with ovarian cancer. On the basis of these examples and the experienced advantages and disadvantages, a novel best practice model for patients with ovarian cancer is proposed, to ensure that patients and relatives receive consistency of care and that sequence variants are interpreted and managed appropriately.20
The effect of new treatment options on the existing BRCA testing process
Utilising BRCA testing to inform treatment selection is likely to add greater complexity to the existing testing process (Figure 1). Early and rapid BRCA testing has already been introduced in the workflow of many centres for newly diagnosed women with breast cancer who have characteristics of an inherited predisposition, in order to inform surgical decisions (eg, bilateral mastectomy).21 Because of the implications of test results on patients and their families (ie, raised cancer risk), current practice in many countries requires face-to-face counselling with a qualified genetics counsellor both before and following BRCA testing.22 As genetic testing may take place early in routine patient care in order to guide management decisions, the content and timing of genetic counselling is likely to change in the future.23
As models of genetic counselling evolve, a multidisciplinary team of professionals, including clinical geneticists, gynaecologists, surgeons, radiotherapists and medical oncologists will be increasingly involved in the process.23 Any future model of BRCA testing and genetic counselling will need to address a range of issues that arise in genetic counselling. For example, broader cancer gene testing may lead to a higher probability of identifying a ‘variant of unknown significance’ rather than a known pathogenic mutation, which requires careful interpretation and sensitive explanation by a clinical geneticist.24, 25 In addition, clinicians need to be aware of the different clinical consequences of a somatic versus a germline pathogenic BRCA mutation. Furthermore, if a negative BRCA result is received, other less frequent genetic causes of cancer predisposition need to be considered.
The effect of genetic testing reaches beyond the patient with cancer and affects the entire family. Not only are there consequences for relatives once a pathogenic BRCA mutation is found but also when no such mutation is found, as the relative may still have a high familial risk for cancer and the need for cancer prevention. Currently, the majority of oncologists are not accustomed in calculating and communicating cancer risks for relatives.26 The information provided to patients and their relatives needs to be consistent among all members of the multidisciplinary team and a clinical geneticist must be part of this team. Importantly, professionals involved in BRCA testing need to be aware of the psychological consequences of BRCA genetic testing, which may result in distress during the testing process and/or after carrier status is identified.27, 28, 29
Models of germline BRCA testing
Research is currently being undertaken on novel approaches to BRCA testing and genetic counselling.24, 30, 31, 32 These alternative processes may act as a guide to optimal practice as the demand for access to genetic counsellors and clinical geneticists increases. The following section outlines four approaches to genetic counselling and discusses the associated issues and benefits of each in the context of current practice.
Current practice: the Huntington protocol
Because of the potentially far-reaching implications of BRCA susceptibility testing, a lighter version of the ‘Huntington protocol’ was adopted for the counselling of unaffected individuals who wanted to determine whether they had inherited a familial pathogenic mutation in BRCA.22 Predictive testing is generally offered solely to adults at risk, who have had the appropriate counselling, are fully informed and wish to proceed.22 The guidelines recommend that individuals who undergo predictive testing are seen for two to four counselling sessions, spread over a 3-month period, before disclosure of the test results.22 If a pathogenic mutation is found, counselling must be offered to the family and others involved.
The pre-test counselling sessions allow for advance consideration of medical options and the impact that test results may have on the individual as well as on family members, while post-test counselling provides a valuable opportunity for health-care providers to interpret test results and to decide whether additional genetic testing is needed. For instance, in women with ovarian cancer and a family history for colorectal cancer, analysis of the mismatch repair genes may reveal Lynch syndrome. Another item in the post-counselling is to emphasise the importance of continuing regular preventive activities for the patient and for relatives if indicated.33 For example, if a patient receives a negative BRCA test result, a personalised and intensified breast surveillance protocol in agreement with increased familial cancer risk as calculated from the exact family history is often advised for specific female relatives. Therefore, relatives may benefit from cancer prevention both in cases of a pathogenic mutation in BRCA or in cases of a positive family history hinting at a high familial cancer risk.
Although there are local or national variations of this process, the universal characteristic is the need for at least one pre-test counselling session with a genetic counsellor or a clinical geneticist. The strength of this approach is the face-to-face contact with a health-care professional who is specifically trained in discussing the medical and psychological implications of genetic testing; however, this approach may no longer be possible in the era of treatment-based genetic counselling, which demands faster turnaround times.23
The ‘DNA-direct’ model (The Netherlands)
The ‘DNA-direct’ model is a telephone-based genetic counselling model for patients with breast cancer. It is a novel approach that replaces the initial consultation with a telephone call (to provide information, not counselling) and written and digital information, which is sent home with the patient; face-to-face counselling is offered only after BRCA testing, where the counsellor discloses the DNA results and delivers customised advice to the patient (Figure 2).32
The aim of this process is to eliminate extraneous information, which is not applicable to the individual patient, and to provide patients with the information they desire in a quick and patient-centric manner.32
In a study of 161 eligible patients with breast cancer, patients chose either the DNA-direct approach or a traditional DNA-intake approach. The DNA-intake approach offered pre-test face-to-face genetic counselling. The patients who chose the DNA-direct approach received an information package, which included an information letter, a link to a website and access to a short educational movie about hereditary breast cancer and DNA-testing. An appointment for a personal consultation to disclose the results was set for 8 weeks after DNA-testing commenced.32 The fact that patients were not randomised between the two methods of counselling enabled the researchers to measure the percentage of patients that opted for the DNA-direct approach. This study design however introduced a bias and does not allow a thorough comparison between the two approaches.
Overall, 59% of patients chose the DNA-direct approach, of whom 89% were satisfied and would choose DNA-direct again (including 6/8 carriers of a pathogenic BRCA mutation). The self-reported reasons for choosing the DNA-direct or the DNA-intake approach can be seen in Figure 3.32
Patient characteristics differed significantly between the approaches (Figure 3). Participants who had previously received information about personal consequences of hereditary breast cancer, or used websites for breast cancer information, were more likely to choose DNA-direct.32 Those who had received information about genetics in general or who experienced higher decisional conflict were more likely to choose DNA-intake.
General distress and heredity-specific distress scored lower in the DNA-direct group than the DNA-intake group both at baseline and at follow-up 2 weeks after BRCA result disclosure.32 Quality of life, breast cancer worry, risk perception for hereditary breast cancer and second breast cancer did not differ between DNA-direct versus DNA-intake or over time. BRCA pathogenic mutation detection rate was equal between procedures at 8%. Processing time (triage call to patient BRCA result disclosure) was reduced by 1 month with the DNA-direct (70 days) versus the DNA-intake (103 days; P=0.002) approach.32 The total duration of face-to-face contact time was diminished from 60 to 30 min (unpublished data). It is worth noting that processing times are health-system dependent and may vary elsewhere.32
The authors concluded that before BRCA testing, more patients with breast cancer preferred replacing a face-to-face consultation with a trained genetic counsellor by a home information package including telephone, written and digital information. The majority of patients were strongly to moderately satisfied with the procedure without increased distress compared with the face-to-face intake approach.32 Benefits attributed to the DNA-direct approach included the ability to review information at home without having to attend additional hospital/clinic appointments and perceived faster turnaround times; however, this approach may not be suited to all patients. The authors suggest that it may be most appropriate for patients who match the overall profile of DNA-direct participants – more highly educated and better informed patients, who are more certain of genetic testing and show less distress.32
Telephone-based counselling model (USA)
The telephone-based counselling model was made for healthy relatives or patients after successful breast or ovarian cancer treatment. Genetic counselling offered via telephone has the potential to broaden the reach and accessibility of BRCA1/BRCA2 testing – especially in rural areas or where there is limited access to genetic counselling resources – and to reduce costs (Figure 4).31
A study by Schwartz et al.31 compared telephone delivery of BRCA genetic counselling with in-person delivery. Women aged 21–85 years, who did not have newly diagnosed or metastatic cancer and who lived within a study site catchment area, were randomly assigned to usual care or telephone counselling. Usual care participants received in-person pre- and post-test counselling while telephone counselling participants completed all counselling by telephone. Telephone counselling was non-inferior to usual care on all primary outcomes (Figure 5).
One area where telephone counselling was not equivalent to usual care was on BRCA test uptake: 84% of patients randomised to telephone counselling went on to have a BRCA test compared with 90% following usual care. Patients receiving usual care could supply a DNA sample directly after their counselling session, whereas telephone-counselled patients had to travel to a clinic to provide a sample. Moreover, the time between the telephone counselling session and attending the clinic may have provided time for deliberation and reconsideration, leading patients to forgo testing.
The outcome of this study might have been influenced by the fact that ‘direct-to-consumer’ genetic testing is offered by numerous companies in the USA and therefore is more common practice than in other countries. Especially in Europe, this is not common practice. In our opinion, it is important to note that telephone counselling may not be appropriate for newly diagnosed patients with cancer or patients with metastatic cancer, for whom the reassurance of face-to-face guidance is important.
Royal Marsden testing model (UK)
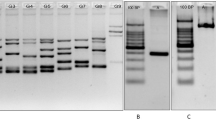
At the Royal Marsden Hospital in London a new mainstreaming model for BRCA testing in patients with ovarian cancer has been implemented.34 This pathway requires non-geneticists to undertake online training and follow clear protocols that delineate the patient pathway and the approval process (Figure 6).
The Royal Marsden BRCA testing model.31
This approach aims to bring gene testing to the patient through their existing oncology appointments. Trained members of the oncology team manage the pre-test consultation; however, patients are referred to the Cancer Genetics Unit if more detailed discussions are required. Any patient found to carry a pathogenic mutation is seen by a geneticist in the Cancer Genetics Unit; those with normal results are referred to the Cancer Genetics Unit only if requested by the patient.
In a pilot from July to December 2013, 119 women with either non-mucinous ovarian cancer diagnosed at <65 years or ovarian or breast cancer at any age were tested.34 No patients requested additional Cancer Genetics Unit input before the test. Among the 119 women tested, 20 patients (17%) carried a pathogenic mutation (BRCA1 n=8, BRCA2 n=12). Of those with a pathogenic mutation, 60% were assessed as having no family history of breast and/or ovarian cancer. Nine of the carriers of a pathogenic mutation had an immediate change in management due to BRCA status. It should be noted that data on family history from this study were not validated or checked and no data are available on uptake of BRCA cascade testing in relatives.
Somatic (tumour) pathogenic mutations in BRCA: is there a case for testing prior to germline testing?
Although research has demonstrated that germline pathogenic mutations in BRCA1/BRCA2 in ovarian cancer can deregulate homologous recombination (HR), and thereby increase a patient’s sensitivity to platinum-based chemotherapy and possibly to treatment with PARP inhibitors, few studies have investigated the potential impact of somatic sequence variants on BRCA function.9, 10, 11, 12
A recently published study has demonstrated that germline and somatic pathogenic mutations in HR genes (BRCA1, BRCA2, ATM, BARD1, BRIP1, CHEK1, CHEK2, FAM175A, MRE11A, NBN, PALB2, RAD51C and RAD51D) occur in ~31% of patients with serous or non-serous ovarian cancer.12 Of these, 75% of germline HR mutations and 71% of somatic HR mutations were in BRCA.12 Patients with a germline or somatic HR pathogenic mutation were more sensitive to primary platinum chemotherapy and experienced improved overall survival (66 months, germline HR mutation; 59 months, somatic HR mutation; and 41 months, no HR mutation) compared with patients with no HR pathogenic mutations.12
The role of somatic pathogenic BRCA mutations in platinum-based chemotherapy sensitivity, and their potential role in PARP inhibitor sensitivity, suggests that the number of women with ovarian cancer who might benefit from these treatments is greater than predicted by the frequency of germline pathogenic mutations.10 Consequently, there is a possible case for the inclusion of somatic pathogenic mutation testing in the BRCA testing process.
The ‘Nijmegen tumour analysis plan’ is one such proposed genetic counselling pathway that includes BRCA testing of ovarian tumour samples from newly diagnosed patients with ovarian cancer as a means of pre-screening for germline BRCA testing. The benefit of this plan is twofold. First, this allows more effective recognition of patients who may benefit from PARP inhibitor treatments. Second, and equally important, these patients are also eligible for germline BRCA-analysis to determine hereditary cancer risks in their relatives, who may benefit from cancer-prevention measures. Half of the tumour BRCA pathogenic mutations are accompanied by a germline BRCA pathogenic mutation.35 Therefore, the use of tumour BRCA testing as a pre-screen for germline BRCA testing would reduce the number of patients referred for genetic counselling and increase the pathogenic mutation detection rate of germline BRCA testing from 12 to 50%. We are aware that tumour BRCA testing poses several challenges for laboratories, which are discussed in the accompanying article by Andrew Wallace (New challenges for BRCA testing: a view from the diagnostic laboratory).
Summary of BRCA testing and counselling models
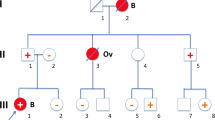
It is possible that future BRCA testing and counselling models will incorporate different elements of those models described above. In Figure 7, a hypothetical BRCA testing model is described for a broader ovarian cancer population that keeps the patient and their relatives well informed of the test consequences throughout the process. In this model, all newly diagnosed patients with epithelial ovarian cancer receive an initial BRCA test of tumour samples guided by a gynaecologist. For those patients testing positive for a BRCA tumour pathogenic mutation with or without a positive family history of cancer, a clinical geneticist would provide counselling before germline BRCA testing. On the basis of patient preferences, this could be via telephone with additional educational resources provided in the form of written and digital information. Following germline BRCA testing, all patients would be provided with face-to-face genetic counselling with a clinical geneticist. Patients who test negative for a BRCA tumour pathogenic mutation but have a positive family history of cancer would also be referred for genetic counselling.
There is still some ambiguity amongst national and society guidelines on the universal approach of BRCA testing for all newly diagnosed patients with ovarian cancer, with several still having a requirement of a pre-test probability threshold to be met before genetic testing is offered.36 Arguments for having a pre-test probability threshold are generally based on the cost implications and potential overload to existing health-care infrastructure and services.36 There will also be some patients who will not choose to have genetic testing performed due to ethical/religious beliefs or comorbidities such as psychological conditions.
The importance of education and the management of patient preferences in the genetic counselling process
Educating women and their families on the consequences of genetic testing so that they can make an informed decision about whether to proceed is a central tenet of the genetic counselling process. In most women, this can be achieved successfully through face-to-face or telephone-based consultations with clinical geneticists, or at home via printed and digital media.24, 30, 31, 32
Patients at risk of a hereditary predisposition are likely to prefer information that is specific to their familial risk of cancer and the treatment or prophylactic options available to them over general information on genetics.37 Providing personalised information as early as possible and reducing the long period of uncertainty during the genetic diagnostic process may prove helpful.32
Studies have consistently reported high levels of inaccurate risk perception in women at high risk, even after counselling.38 Therefore, health-care professionals involved in the genetic counselling process must be adequately trained to ensure that genetic test results are correctly interpreted and the potential consequences of those results are clearly and consistently communicated to the patient.
A single approach to genetic counselling may not be appropriate for all patients. Although the majority of patients are comfortable with receiving pre-test information via telephone, print or digital media, others express a preference for the personal contact of a face-to-face consultation with a clinical geneticist.32, 39 Determining patient preferences early in the genetic counselling process, and ensuring that the process is flexible enough to accommodate a range of preferences, will ensure that both the needs of the patient and of her relatives are adequately met.23
Conclusions
In many countries, genetic counselling before BRCA testing is carried out face-to-face by a qualified genetic counsellor or a clinical geneticist. Germline BRCA testing without prior face-to-face genetic counselling could be considered for selected patients who are adequately informed by their oncologist together with telephone, digital or written information from a clinical geneticist. This could include all patients with ovarian cancer and breast cancer patients with a positive family history of breast or ovarian cancer.
There is a general consensus that after a positive BRCA test result or in cases of highly suggestive family history for hereditary cancer, face-to-face counselling with a clinical geneticist is important in order to discuss the consequences of the results for the patient and other family members, as well as to explain complex test results and other hereditary causes of cancer. Evidence suggests that there is a case for extending genetic testing to all patients with ovarian cancer; the inclusion of genetic testing for somatic pathogenic mutations may also prove valuable. In the era of personalised care and treatment-based genetic counselling these approaches may form the basis of optimising future workflow.
References
Chen S, Parmigiani G : Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol 2007; 25: 1329–1333.
Mavaddat N, Peock S, Frost D et al: Cancer risks for BRCA1 and BRCA2 mutation carriers: results from prospective analysis of EMBRACE. J Natl Cancer Inst 2013; 105: 812–822.
National Institute of Health and Care Excellence (NICE): Clinical guideline 164: familial breast cancer. Last update 2013. Available at www.nice.org.uk/guidance/cg164 (accessed on 27 April 2015).
Scottish Intercollegiate Guidelines Network (SIGN): SIGN Guideline No 135 Management of Epithelial Ovarian Cancer. Edinburgh: SIGN, 2013.
Gadzicki D, Evans DG, Harris H et al: Genetic testing for familial/hereditary breast cancer-comparison of guidelines and recommendations from the UK, France, the Netherlands and Germany. J Community Genet 2011; 2: 53–69.
Lambert M : Guidelines for managing hereditary breast and ovarian cancer syndrome. Am Fam Physician 2009; 80: 1505–1507.
Rebbeck TR, Friebel T, Lynch HT et al: Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers: the PROSE Study Group. J Clin Oncol 2004; 22: 1055–1062.
Rebbeck TR, Kauff ND, Domchek SM : Meta-analysis of risk reduction estimates associated with risk-reducing salpingo-oophorectomy in BRCA1 or BRCA2 mutation carriers. J Natl Cancer Inst 2009; 101: 80–87.
Alsop K, Fereday S, Meldrum C et al: BRCA mutation frequency and patterns of treatment response in BRCA mutation-positive women with ovarian cancer: a report from the Australian Ovarian Cancer Study Group. J Clin Oncol 2012; 30: 2654–2663.
Hennessy BT, Timms KM, Carey MS et al: Somatic mutations in BRCA1 and BRCA2 could expand the number of patients that benefit from poly (ADP ribose) polymerase inhibitors in ovarian cancer. J Clin Oncol 2010; 28: 3570–3576.
Lee JM, Hays JL, Annunziata CM et al: Phase I/Ib study of olaparib and carboplatin in BRCA1 or BRCA2 mutation-associated breast or ovarian cancer with biomarker analyses. J Natl Cancer Inst 2014; 106: dju089.
Pennington KP, Walsh T, Harrell MI et al: Germline and somatic mutations in homologous recombination genes predict platinum response and survival in ovarian, fallopian tube, and peritoneal carcinomas. Clin Cancer Res 2014; 20: 764–775.
Rafnar T, Benediktsdottir KR, Eldon BJ et al: BRCA2, but not BRCA1, mutations account for familial ovarian cancer in Iceland: a population-based study. Eur J Cancer 2004; 40: 2788–2793.
Sarantaus L, Vahteristo P, Bloom E et al: BRCA1 and BRCA2 mutations among 233 unselected Finnish ovarian carcinoma patients. Eur J Hum Genet 2001; 9: 424–430.
Stratton JF, Gayther SA, Russell P et al: Contribution of BRCA1 mutations to ovarian cancer. N Engl J Med 1997; 336: 1125–1130.
Yazici H, Glendon G, Yazici H et al: BRCA1 and BRCA2 mutations in Turkish familial and non-familial ovarian cancer patients: a high incidence of mutations in non-familial cases. Hum Mutat 2002; 20: 28–34.
Eccles D, Garcia EG, Balmaña J et al: Selecting Ovarian Cancer Patients for BRCA Mutation Testing: Findings from Guidelines and Literature Review. in Poster at the Conference of the British Society of Genetic Medicine (BSGM); 22–24 September 2014; Liverpool, UK.
Balmaña J, Diez O, Rubio IT, Cardoso F : BRCA in breast cancer: ESMO Clinical Practice Guidelines. Ann Oncol 2011; 22: vi31–vi34.
Daly MB, Pilarski R, Axilbund JE et al: Genetic/familial high-risk assessment: breast and ovarian, version 1.2014. J Natl Compr Canc Netw 2014; 12: 1326–1338.
Slade I, Riddell D, Turnbull C, Hanson H, Rahman N : Development of cancer genetic services in the UK: A national consultation. Genome Med 2015; 7: 18.
Smith KL, Isaacs C : BRCA mutation testing in determining breast cancer therapy. Cancer J 2011; 17: 492–499.
van Oostrom I, Tibben A : A counselling model for BRCA1/2 genetic susceptibility testing. Hered Cancer Clin Pract 2004; 2: 19–23.
Vig HS, Wang C : The evolution of personalized cancer genetic counseling in the era of personalized medicine. Fam Cancer 2012; 11: 539–544.
Arie S : Routine testing for women with ovarian cancer. BMJ 2014; 348: g1200.
Moghadasi S, Hofland N, Wouts JN et al: Variants of uncertain significance in BRCA1 and BRCA2 assessment of in silico analysis and a proposal for communication in genetic counselling. J Med Genet 2013; 50: 74–79.
Dekker N, Hermens RP, de Wilt JH, van Zelst-Stams WA, Hoogerbrugge N : Improving recognition and referral of patients with an increased familial risk of colorectal cancer: results from a randomised controlled trial. Colorectal Dis 2014; 17: 499–510.
Brédart A, Kop JL, Depauw A et al: Short-term psychological impact of the BRCA1/2 test result in women with breast cancer according to their perceived probability of genetic predisposition to cancer. Br J Cancer 2013; 108: 1012–1020.
Hamilton JG, Lobel M, Moyer A : Emotional distress following genetic testing for hereditary breast and ovarian cancer: a meta-analytic review. Health Psychol 2009; 28: 510–518.
Hirschberg AM, Chan-Smutko G, Pirl WF : Psychiatric implications of cancer genetic testing. Cancer 2015; 121: 341–360.
Bjorvatn C, Aas T, Fiane BE et al: BRCA mutation testing in all newly diagnosed patients with breast or ovarian cancer: the DNA BONus study. Abstract P12.016-M at the European Society of Human Genetics (ESHG); 31 May-3 June 2014; Milan, Italy.
Schwartz MD, Valdimarsdottir HB, Peshkin BN et al: Randomized noninferiority trial of telephone versus in-person genetic counseling for hereditary breast and ovarian cancer. J Clin Oncol 2014; 32: 618–626.
Sie AS, van Zelst-Stams WA, Spruijt L et al: More breast cancer patients prefer BRCA-mutation testing without prior face-to-face genetic counseling. Fam Cancer 2014; 13: 143–151.
Robson ME, Storm CD, Weitzel J, Wollins DS, Offit K : American Society of Clinical Oncology policy statement update: genetic and genomic testing for cancer susceptibility. J Clin Oncol 2010; 28: 893–901.
George A, Smith F, Cloke V et al: Implementation of routine BRCA gene testing of ovarian cancer (OC) patients at Royal Marsden Hospital. Ann Oncol 2014; 25: iv305–iv326.
Cancer Genome Atlas Research Network: Integrated genomic analyses of ovarian carcinoma. Nature 2011; 474: 609–615.
NHS England. Clinical Commissioning Policy: Genetic Testing for BRCA1 and BRCA2 Mutations. October 2015; Available at https://www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2015/10/e01pb-brca-ovarian-canceroct15.pdf.
Salemink S, Dekker N, Kets CM, van der Looij E, van Zelst-Stams WA, Hoogerbrugge N : Focusing on patient needs and preferences may improve genetic counseling for colorectal cancer. J Genet Couns 2013; 22: 118–124.
Lobb EA, Butow PN, Meiser B et al: Women's preferences and consultants' communication of risk in consultations about familial breast cancer: impact on patient outcomes. J Med Genet 2003; 40: e56.
Audrain J, Rimer B, Cella D et al: Genetic counseling and testing for breast-ovarian cancer susceptibility: what do women want? J Clin Oncol 1998; 16: 133–138.
Acknowledgements
We kindly thank Dr Marjolijn Ligtenberg for her editorial suggestions and careful review of this manuscript. This supplement was sponsored by AstraZeneca. Medical writing services were provided by Tom Hudson of iMed Comms, Macclesfield, UK and were funded by AstraZeneca.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
NH has received payments for consulting and speaker services from AstraZeneca and has attended advisory boards for AstraZeneca. She has also received grant support from AstraZeneca. MCJJ has declared no conflicts.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Hoogerbrugge, N., Jongmans, M. Finding all BRCA pathogenic mutation carriers: best practice models. Eur J Hum Genet 24 (Suppl 1), S19–S26 (2016). https://doi.org/10.1038/ejhg.2016.95
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2016.95
This article is cited by
-
Real-World Study of Regional Differences in Patient Demographics, Clinical Characteristics, and BRCA1/2 Mutation Testing in Patients with Human Epidermal Growth Factor Receptor 2–Negative Advanced Breast Cancer in the United States, Europe, and Israel
Advances in Therapy (2023)
-
Assessment of small in-frame indels and C-terminal nonsense variants of BRCA1 using a validated functional assay
Scientific Reports (2022)
-
Evaluation of telephone genetic counselling to facilitate germline BRCA1/2 testing in women with high-grade serous ovarian cancer
European Journal of Human Genetics (2019)