Abstract
MED13L haploinsufficiency syndrome has been described in two patients and is characterized by moderate intellectual disability (ID), conotruncal heart defects, facial abnormalities and hypotonia. Missense mutations in MED13L are linked to transposition of the great arteries and non-syndromal intellectual disability. Here we describe two novel patients with de novo MED13L aberrations. The first patient has a de novo mutation in the splice acceptor site of exon 5 of MED13L. cDNA analysis showed this mutation results in an in-frame deletion, removing 15 amino acids in middle of the conserved MED13L N-terminal domain. The second patient carries a de novo deletion of exons 6–20 of MED13L. Both patients show features of the MED13L haploinsufficiency syndrome, except for the heart defects, thus further confirming the existence of the MED13L haploinsufficiency syndrome.
Similar content being viewed by others
Introduction
MED13L (Mediator Complex Subunit 13 like) is one of the many subunits of the Mediator transcription co-activator complex. The complex has been shown to associate with general transcription factors and RNA polymerase II to regulate transcription. The mediator complex is the essential co-activator acting as a bridge between transcription factors bound at upstream DNA regulatory elements and the transcription machinery.1
MED13L was found to map to the breakpoints of a patient with intellectual disability (ID) and transposition of the great arteries. Subsequent sequencing of the gene in a larger cohort of patients with transposition of the great arteries identified three additional missense mutations in MED13L.2 A large resequencing study of homozygous regions in consanguineous patients identified a homozygous missense variant in MED13L as a cause of nonsyndromic ID.3
Asadollahi et al4 presented two patients with MED13L haploinsufficiency. These patients suffered from a similar phenotype of hypotonia, moderate ID, conotruncal heart defects and specific dysmorphic facial features, including macroglossia. Their findings showed that MED13L haploinsufficiency in contrast to the previously observed missense mutations cause a distinct syndromic phenotype.
Here, we describe two new patients with de novo MED13L aberrations who are phenotypically similar to the patients described by Asadollahi et al4 but lack the cardiac phenotype.
Patients and methods
Ethical approval
Informed consent for whole-exome sequencing and subsequent Sanger sequencing as a part of the diagnostic process (approved by the Medical Ethical Committee of the University Medical Center Utrecht) was obtained for case 1 and her parents. Informed consent for array CGH was obtained for case 2 and her parents. Consent to publish clinical photographs was obtained for both cases included in this study.
Patient 1
The first patient is the second child of healthy non-consanguineous Caucasian parents. She was born after a twin pregnancy of 37 weeks with a weight of 3020 g. After birth, a right-sided clubfoot was noted for which she was treated at the age of 11 weeks. Her developmental milestones were delayed: she walked independently at the age of 2½ years and spoke her first sentences at age 3½ years. Because of her developmental delay, she was seen at the age of 14 months by the neurologist who observed hypertonia of all extremities. Her older sister and her twin brother were healthy. Apart from a paternal great uncle who has an intellectual deficit of unknown cause, the family history is unremarkable. On clinical examination at the age of 16 months, height was 75 cm (−1 SD), weight: 8.5 kg (−1 SD) and headsize: 43.5 cm (−1.5 SD). She had a slightly asymmetric face with short, upslanted palpebral fissures, a bulbous nasal tip and protrusion of her tongue (Figure 1; Table 1). She had bilateral accessory nipples, abnormal palmar creases with an extra phalangeal crease of the index fingers. Auscultation of heart and lungs was normal. The right foot showed results of the correction of the clubfoot, and both feet showed a sandal gap. On neurological investigation, she had normal reflexes and no hypertonia of the extremities was observed. No murmur could be heard at cardiac auscultation, an ECG was unremarkable and echocardiography showed a structurally and functionally normal heart. Additional investigations (including MRI of the brain, karyotype, array CGH analysis, metabolic and ophthalmological investigations) were normal.
Facial features of patient 1 and 2 with MED13L aberrations: (a) patient 1 at 6 months and (b) 17 months of age. Note macroglossia, facial asymmetry, upslanting palpebral fissures, flat nasal bridge and dark circles under eyes. (c and d) Patient 2 at age 4½ years: slightly different phenotype: note broad nasal bridge, open mouth appearance.
Patient 2
The second patient was born after an uneventful pregnancy of 42 weeks with a weight of 3300 g. Prenatal karyotyping indicated by increased nuchal translucency showed a normal male karyotype. The neonatal period was complicated by feeding problems, eczema and gastroesofageal reflux, which all improved after induction of bottle feeding. Grommets were inserted three times because of recurrent ear infections. Hearing and vision were normal. He had a motor- and speech developmental delay (walking independently at the age of 24 months, and spoke only 10 words at the age of 4 years). There were no behavioral problems. Parents were non-consanguineous and family history is non-contributory. On clinical examination (at the age of 4 years and 2 months) height was: 97 cm (−2.25 SD), weight: 14.55 kg (0 SD) and OFC: 50 cm (−0.5 SD). Facial dysmorphisms include small eyelids and mild retrognathia (Figure 1; Table 1). Cardiac screening was unremarkable; no murmur was present at auscultation, ECG was normal and echocardiography showed a structurally and functionally normal heart with a small persistent foramen ovale (PFO). Metabolic screening and DNA analysis for Fragile X syndrome showed no abnormalities.
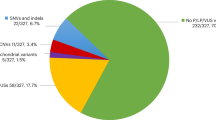
Whole-exome sequencing and array CGH analysis
Trio-based whole-exome sequencing was performed on patient 1 and parents as described previously5 with the alterations that sequencing was performed on the Solid 5500 platform and enrichment was performed using the Agilent Sureselect kit (v4; Agilent, Santa Clara, CA, USA). The obtained average coverage was 69, 77 and 66 × for the patient, father and mother, respectively. Filtering variants with a predicted effect at the protein level using a de novo hypothesis yielded 11 candidate mutations, of which one could be validated by Sanger sequencing (MED13L: NC_000012.11:g.116460407C>A). Filtering with a recessive hypothesis yielded no sound candidate variants. No further rare variants in the MED13L coding regions were identified.
Array CGH was performed on an Agilent 180 K oligo-array (amadid 023363) on patient 2 plus the parents.
Splicing analysis
cDNA was generated using High Capacity cDNA Reverse Transcription Kit (Life Technologies, Carlsbad, CA, USA) on RNA isolated from lymphocytes using Trizol reagent (Life Technologies). Subsequently, PCRs were performed using cDNA specific primers located in the different exons of MED13L (sequence available upon request), followed by excision of the bands from an agarose gel and purification of DNA (QIAquick, Qiagen, Hilden, Germany) followed by Sanger sequencing.
Databases
Mutations and phenotypic details from both patients were submitted to Decipher.6
Results
We performed trio-based whole-exome sequencing on patient 1 and her parents. We identified a single de novo mutation in a consensus splice acceptor site of exon 5 of MED13L (NM_015335.4:c.480-1G>T; exons numbered as in NC_000012.11; Figure 2a). Analysis of cDNA derived from lymphocyte RNA from this patient identified a single alternatively spliced MED13L transcript not present in controls (Figure 2b). Subsequent sequencing of the transcript identified a cryptic splice acceptor site, 45 nucleotides into exon five, which was used in the patient but not in controls. This alternative splicing results in an in-frame deletion of 45 base pairs in the cDNA and deletion of 15 amino acids in the middle of the MED13L N-terminal domain (NM_015335.4:r.480_524del and NP_056150.1:pSer160_Glu174del; Figure 2c), which is a highly conserved domain of unknown function.3 The deletion of multiple amino acids in a highly conserved domain is likely to affect MED13L protein function.
MED13L abberations. (a) Genomic structure of human MED13L with indicated de novo splice site mutation in patient 1 and the minimal de novo deletion of patient 2. (b) Agarose gel results of a PCR on cDNA with primers located on exons 4 and 7. Pt1 denotes cDNA from patient 1 and Ctrl cDNA from a control cDNA sample. The cDNA PCR of patient 1 shows an additional lower band (indicated by arrow). The predicted size of the wildtype band is 467 bp. Sanger sequencing of the band proved an in-frame partial deletion of exon 5. (c) Protein structure of human MED13L, with the conserved protein domains indicated. The splice site mutation in patient 1 results in a deletion of 15 amino acids (160–174) in the conserved MED13L N-terminal domain. The minimal deleted region of patient 2 encompasses exons 6–20 in the middle of the MED13L protein.
Array CGH analysis revealed a deletion of 41 kb containing and disrupting the distal part of the MED13L gene (NC_000012.11:g.(?_116419988)_(116460600_?)del). Additional array studies in both parents revealed that the deletion had arisen de novo. This deletion removes exons 6–20, of the 31 exons of the MED13L gene, likely resulting in loss of protein function (Figure 2c).
Discussion
Recently, the MED13L haploinsufficiency syndrome has been characterized by moderate ID, conotruncal heart defects, facial abnormalities and hypotonia.4 Missense mutations in MED13L were already reported in a cohort of patients with congenital heart defects.2 As parents of those cases were not studied and no phenotype details were available, the relevance of these three missense variants remains unclear. The cases reported here show a similar phenotype as the previously reported syndromal cases4 (Table 1). They both have a delay in motor and speech development and both show a hypotonic open-mouth appearance on clinical examination. Patient 1 also has an asymmetric face with macroglossia and bulbous nasal tip as was decribed in the previous report. Both our cases, however, lack the previously reported cardiac phenotype. This shows reduced penetrance of the cardiac anomalies as part of this syndrome.
In summary, we report two new cases with ID and facial dysmorphic features caused by MED13L haploinsufficiency. Both cases do (apart from the frequently identified small PFO in patient two) not show cardiac anomalies, thereby underlining the reduced penetrance of the cardiac phenotype in of MED13L haploinsufficiency syndrome. Our study thus confirms the existence of a MED13L haploinsufficiency syndrome characterized by ID and specific dysmorphic facial features with macroglossa and shows a reduced penetrance of the cardiac anomalies.
References
Sato S, Tomomori-Sato C, Parmely TJ et al: A set of consensus mammalian mediator subunits identified by multidimensional protein identification technology. Mol Cell 2004; 14: 685–691.
Muncke N, Jung C, Rüdiger H et al: Missense mutations and gene interruption in PROSIT240, a novel TRAP240-like gene, in patients with congenital heart defect (transposition of the great arteries). Circulation 2003; 108: 2843–2850.
Najmabadi H, Hu H, Garshasbi M et al: Deep sequencing reveals 50 novel genes for recessive cognitive disorders. Nature 2011; 478: 57–63.
Asadollahi R, Oneda B, Sheth F et al: Dosage changes of MED13L further delineate its role in congenital heart defects and intellectual disability. Eur J Hum Genet 2013; 21: 1100–1104.
Harakalova M, van Harssel JJ, Terhal PA et al: Dominant missense mutations in ABCC9 cause Cantú syndrome. Nat Genet. 2012; 44: 793–796.
Firth HV, Richards SM, Bevan AP et al: DECIPHER: Database of Chromosomal Imbalance and Phenotype in Humans using Ensembl Resources. Am J Hum Genet 2009; 84: 524–533.
Acknowledgements
We thank Ies Nijman and Edwin Cuppen for support in sequencing and bioinformatics.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
van Haelst, M., Monroe, G., Duran, K. et al. Further confirmation of the MED13L haploinsufficiency syndrome. Eur J Hum Genet 23, 135–138 (2015). https://doi.org/10.1038/ejhg.2014.69
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2014.69
This article is cited by
-
Detection of aberrant gene expression events in RNA sequencing data
Nature Protocols (2021)
-
Use of whole genome analysis to identify shared genomic variants across breeds in canine mitral valve disease
Human Genetics (2021)
-
Report of a de novo c.2605C > T (p.Pro869Ser) change in the MED13L gene and review of the literature for MED13L-related intellectual disability
Italian Journal of Pediatrics (2020)
-
Analysis of Polymorphisms in the Mediator Complex Subunit 13-like (Med13L) Gene in the Context of Immune Function and Development of Experimental Arthritis
Archivum Immunologiae et Therapiae Experimentalis (2018)
-
Variants in members of the cadherin–catenin complex, CDH1 and CTNND1, cause blepharocheilodontic syndrome
European Journal of Human Genetics (2018)