Abstract
X-linked intellectual disability (XLID), also known as X-linked mental retardation, is a highly genetically heterogeneous condition for which mutations in >90 different genes have been identified. In this study, we used a custom-made sequencing array based on the Affymetrix 50k platform for mutation screening in 17 known XLID genes in patients from 135 families and found eight single-nucleotide changes that were absent in controls. For four mutations affecting ATRX (p.1761M>T), PQBP1 (p.155R>X) and SLC6A8 (p.390P>L and p.477S>L), we provide evidence for a functional involvement of these changes in the aetiology of intellectual disability.
Similar content being viewed by others
Introduction
Mental retardation/intellectual disability (ID) has a prevalence of ∼2% in the general population.1 Therefore, as well as because of the life-long restrictions for the patients and their families in combination with extremely limited therapeutic options, ID ranges among the top health issues of our time. Significantly more males compared with females are affected, which can be partly accounted for by mutations in genes on the X chromosome. Moderate-to-severe forms of X-linked ID (XLID) affect 0.05%2 of the population in developed countries. The majority of the patients show non-syndromic forms of XLID (NS-XLID), in which ID is the only clinically consistent manifestation.
On the genetic level, NS-XLID is highly heterogeneous and the causative mutations known to date were found in more than 37 genes, each gene accounting for only a few percent of the cases.1, 3 Families with several affected members from different generations are suitable for linkage analysis, and such families have therefore been instrumental in finding many of the presently known mutations that cause NS-XLID. However, to identify the underlying genetic defect in small ID families or in sporadic patients, a different approach is required. Thus, to investigate the genetic basis of ID in 135 small families from the cohort of the European MRX (Euro-MRX) consortium (http://www.euromrx.com), we have designed a resequencing array based on the Affymetrix 50k platform, containing the coding and splice site regions of 17 XLID genes (see below), with a relatively high mutation frequency in NS-XLID patients. Application of this array led to the identification of eight previously unknown changes in these genes.
Subjects and methods
Patients and controls
DNA from 135 unrelated ID patients without a molecular diagnosis were collected through the Euro-MRX consortium. The majority of patients were from families with no more than two affected brothers. After obtaining written informed consent from the probands or their parents, DNA was extracted from patient blood or blood-derived lymphoblastoid cell lines using standard methods. The study was approved by the relevant institutional review board.
Resequencing array
A custom resequencing array was designed based on the Affymetrix 50k platform (Affymetrix, Santa Clara, CA, USA), allowing up to 50 kb of DNA to be sequenced in both orientations in a single hybridisation experiment.
The oligonucleotides on the array contain sequences that include the coding regions and splice sites (10 nucleotides flanking each exon) of ACSL4, ARX, ATRX, DLG3, FTSJ1, GDI1, IL1RAPL1, JARID1C, MECP2, NLGN4, PAK3, PHF6, PHF8, PQBP1, SLC6A8, TM4SF2 and ZNF41.
PCR amplification of DNA, purification and hybridisation
A total of 151 PCR amplicons were produced from genomic DNA (Supplementary Material) and subsequently purified by alcohol. The purified DNA fragments were pooled in equimolar quantities (0.055 pmol of each PCR product, that is, 36.3 ng per 1000 bp) and the volume was reduced by evaporation using a vacuum centrifuge.
Fragmentation of the products, labelling of the products with biotin, hybridisation, washing and scanning procedures were carried out according to the CustomSeq Resequencing Array Protocol version 2.0 (Affymetrix).
Data analysis
The raw sequencing data were analysed using the Affymetrix GeneChip Analysis Software (GSEQ) version 4.0 (Affymetrix). Only nucleotides that were called on both DNA strands using a quality score threshold equal to 0 were considered. As we only used DNA from male patients (hemizygous for X-chromosomal genes), we did not consider heterozygous base calls. The entire data set was also analysed using SeqC (JSI medical systems, Kippenheim, Germany) as previously described.4
RT-PCR and measurement of ACSL4 and SLC6A8 activity
RT-PCR was performed according to standard protocols. Enzymatic activity of ACSL4 and the urinary creatine/creatinine ratio were measured as described previously.5, 6
Protein extraction and western blot analysis
Cells from control and patient lymphoblastoid cell lines were lysed in buffer containing 48% urea, 15 mM Tris (pH 7.5), 8.7% glycerol, 1% SDS, 0.004% bromophenol blue and 143 mM β-mercaptoethanol. Western blot analysis was performed as previously described.7
Results and discussion
Using a combination of automated and manual PCR, we produced 151 amplicons, containing the coding regions and splice sites of 17 known XLID genes (Table 1), from each of 135 ID patient DNAs (Supplementary Table 1).
As all PCR products had the expected size, we could exclude the presence of larger deletions or insertions in these 17 genes. Small in-dels cannot be detected because of the nature of hybridisation-based sequencing,8, 9 however, as in-dels in the 17 investigated genes are much less frequent than missense mutations (Human Mutation Database), it is possible, but not very likely, that undetected in-dels are present in these 17 genes in the analysed patient cohort.
In addition, we sequenced the amplicons containing the tri-nucleotide repeats in ARX by Sanger sequencing to rule out mutations in this region, as repeat expansions are also not detectable by array-based resequencing.
The remaining PCR products were submitted to fragmentation and labelling. After hybridisation, washing and scanning of the arrays, we obtained call rates between 90 and 96% and found 478 different nucleotide changes (excluding known SNPs). The specified call accuracy for this array type is 99.99% (1 error in 10 000 nucleotide calls) when – like in this study – no heterozygous base calls are expected. Thus, four to five falsely called nucleotides per patient DNA (600 in 135 patients) had to be expected. As a filtering criterion to remove false-positive sequence changes from the data set, we used the call rate among the five immediately adjacent bases on either side of a given base. Assuming that fragments with poor sequence quality harboured a substantial amount of falsely called bases, we focused on sequence changes for which the 10 surrounding nucleotides contained at least 6 positions with a base call. This threshold reduced the number of putative nucleotide changes from 478 to 75. The amplicons containing these changes were then investigated by Sanger sequencing, which led to the identification of 10 verifiable nucleotide substitutions in 9 families. All these sequence changes were found in fragments in which at least 8 called bases were present in the 10 surrounding nucleotide positions.
To test the validity of the filtering procedure, we applied SeqC, a module of the Sequence Pilot software (JSI medical systems), for an independent analysis of the whole data set, and identified one additional change in the intron of ACSL4. This change was not detected with the previously applied filtering procedure, because it is located close to the end of an amplicon and, therefore, lacked the mandatory five nucleotides on one side.
For each verified nucleotide alteration, we then sequenced DNA from all available family members to investigate co-segregation with the disorder. Furthermore, we analysed DNA from 138 healthy males to exclude common polymorphisms. This ruled out the change in PHF8 c.441T>G, which was found once in the control panel, and the change in NLGN4X c.968A>G, which did not segregate with the disorder in the family. These two changes are therefore unlikely to be pathologically relevant. The remaining eight potentially disease-causing changes are listed in Table 2.
For the silent change in JARID1C and the intronic change in ACSL4, RT-PCR experiments showed normal levels of gene expression and a normal splicing pattern in patient lymphoblastoid cell lines (data not shown), indicating that these changes are probably benign. What is more, in case of the missense change in ACSL4 (c.1382C>T, p.461P>L), the functional integrity of the gene product seemed uncompromised, as enzymatic activity of ACSL4 in a lymphoblastoid cell line from affected individual was normal. In addition to the intronic change in ACSL4, we also found an intronic change in PQBP1 in the same patient DNA (P122). The intronic change (c.586+25G>A) in the main known PQBP1 transcript (NM_005710.2) did not alter the PQBP1 splicing pattern, as investigated by RT-PCR. However, the change also introduces a missense change (p.201G>D) in one PQBP1 isoform (AJ973600.1). This isoform is very weakly expressed, and further studies are required to determine whether this change is pathogenic or not.
The patient in whom we found a p.1761M>T missense change in ATRX was previously considered to have a non-syndromic phenotype. As our finding indicated that he was actually suffering from ATRX (Alpha-thalassemia X-linked mental retardation) syndrome, we initiated a clinical re-examination. This revealed the presence of characteristic dysmorphic features, providing strong evidence for the pathological relevance of this novel mutation.
One change in SLC6A8 (c.1169C>T, p.390P>L) is identical to a change previously reported in a family with ID10 and later shown to be pathogenic.11
The second change (c.1430C>T, p.477S>L) in SLC6A8 was not observed before, and investigation of the urine creatine/creatinine ratio in the index patient revealed an abnormally elevated value of 1.01 (normal levels in adults: <0.25), confirming the molecular finding.
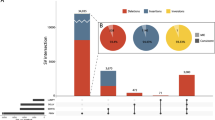
Interestingly, we also identified a novel nonsense mutation (c.463C>T) in exon 4 of PQBP1, which is frequently mutated in ID patients.12 The change results in the introduction of a premature stop codon (p.155R>X). Western blot analysis demonstrated that truncated PQBP1 protein resulting from this mutation is present in the patient (Figure 1), as already shown for other patients with similar PQBP1 mutations,7 supporting its pathological relevance.
PQBP1 expression in control and patient lymphoblastoid cell lines. Whole-cell lysates from a control and a patient lymphoblastoid cell line that harbours a truncating mutation in PQBP1 (N143) were run in parallel on an SDS-PAGE gel. The gel was blotted and probed with an antibody specific for the N-terminal part of PQBP1 (α-N1-PQBP1).7 In the control cell line lysate, a band corresponding to wild-type PQBP1 protein was observed at ∼37 kDa, and in the patient cell line lysate, a truncated PQBP1 protein was observed at ∼22 kDa.
In summary, the discovery of 4 putative disease-causing mutations in 7 out of 135 XLID patients equals a proportion of ∼3%, which is well within the expected range. First because, on the basis of observations by the EURO-MRX consortium, only ∼40% of the male patients (ie, here 54 out of 135) from small families can be assumed to carry a single gene defect on the X chromosome13 and second because the frequencies of disease-causing mutations in the selected genes are each below a few percent.1, 14 The fact that we found an excess of missense mutations, as compared with protein-truncating mutations, is also in line with previous findings.14 The advantages of array-based resequencing include the potential for automation of sample preparation, the speed with which base calling is performed and the comparatively low cost. Array-based resequencing is therefore an option when large cohorts are analysed for sequence changes in defined DNA regions. Considerations for array design and the limitations of array-based resequencing have been thoroughly discussed.15 However, alternatives to array-based resequencing are now available in the form of next-generation sequencing methods, which use sequencing by synthesis. Recently, a protocol for enrichment and subsequent sequencing of DNA fragments that contain the desired sequences has been published.16 This or similar approaches can reduce the time involved in the sequencing procedure considerably and will provide new options for elucidating the aetiology of ID in the so far unresolved cases.
References
Ropers HH : Genetics of intellectual disability. Curr Opin Genet Dev 2008; 18: 241–250.
Leonard H, Wen X : The epidemiology of mental retardation: challenges and opportunities in the new millennium. Ment Retard Dev Disabil Res Rev 2002; 8: 117–134.
Gécz J, Shoubridge C, Corbett M : The genetic landscape of intellectual disability arising from chromosome X. Trends Genet 2009; 25: 308–316.
Schroeder C, Stutzmann F, Weber BH, Riess O, Bonin M : High-throughput resequencing in the diagnosis of BRCA 1/2 mutations using oligonucleotide resequencing microarrays. Breast Cancer Res Treat 2010; 122: 287–297.
Longo I, Frints SG, Fryns JP et al: A third MRX family (MRX68) is the result of mutation in the long chain fatty acid-CoA ligase 4 (FACL4) gene: proposal of a rapid enzymatic assay for screening mentally retarded patients. J Med Genet 2003; 40: 11–17.
Almeida LS, Verhoeven NM, Roos B et al: Creatine and guanidinoacetate: diagnostic markers for inborn errors in creatine biosynthesis and transport. Mol Genet Metab 2004; 82: 214–219.
Musante L, Kunde SA, Sulistio TO et al: Common pathological mutations in PQBP1 induce nonsense-mediated mRNA decay and enhance exclusion of the mutant exon. Hum Mutat 2010; 31: 90–98.
Hartmann A, Thieme M, Nanduri LK et al: Validation of microarray-based resequencing of 93 worldwide mitochondrial genomes. Hum Mutat 2009; 30: 115–122.
Fokstuen S, Lyle R, Munoz A et al: A DNA resequencing array for pathogenic mutation detection in hypertrophic cardiomyopathy. Hum Mutat 2008; 29: 879–885.
Rosenberg EH, Almeida LS, Kleefstra T et al: High prevalence of SLC6A8 deficiency in X-linked mental retardation. Am J Hum Genet 2004; 75: 97–105.
Rosenberg EH, Martínez Muñoz C, Betsalel OT et al: Functional characterization of missense variants in the creatine transporter gene (SLC6A8): improved diagnostic application. Hum Mutat 2007; 28: 890–896.
Kalscheuer VM, Freude K, Musante L et al: Mutations in the polyglutamine binding protein 1 gene cause X-linked mental retardation. Nat Genet 2003; 35: 313–315.
de Brouwer AP, Yntema HG, Kleefstra T et al: Mutation frequencies of X-linked mental retardation genes in families from the EuroMRX consortium. Hum Mutat 2007; 28: 207–208.
Tarpey PS, Smith R, Pleasance E et al: A systematic, large-scale resequencing screen of X-chromosome coding exons in mental retardation. Nat Genet 2009; 41: 535–543.
Kothiyal P, Cox S, Ebert J, Aronow BJ, Greinwald JH, Rehm HL : An overview of custom array sequencing. Curr Protoc Hum Genet 2009 Chapter 7:Unit 7.17.
Hodges E, Rooks M, Xuan Z et al: Hybrid selection of discrete genomic intervals on custom-designed microarrays for massively parallel sequencing. Nat Protoc 2009; 4: 960–974.
Acknowledgements
We thank Sven Poths for technical assistance. This study was supported by the Max Planck Innovation Fund. Additional funding was provided to HHR by the German Federal Ministry of Education and Research (MRNET 01GS08161-2).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Databases
UCSC Genome Browser: http://genome.ucsc.edu/cgi-bin/hgTracks?org=human
The Human Gene Mutation Database: http://www.hgmd.cf.ac.uk/ac/validate.php
Ensembl: http://www.ensembl.org/index.html
Euro-MRX Consortium: http://www.euromrx.com
Supplementary Information accompanies the paper on European Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Jensen, L., Chen, W., Moser, B. et al. Hybridisation-based resequencing of 17 X-linked intellectual disability genes in 135 patients reveals novel mutations in ATRX, SLC6A8 and PQBP1. Eur J Hum Genet 19, 717–720 (2011). https://doi.org/10.1038/ejhg.2010.244
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2010.244
Keywords
This article is cited by
-
Brief Report: Evidence of Autism Spectrum Disorder Caused by a Mutation in ATRX Gene: A Case Report
Journal of Autism and Developmental Disorders (2024)
-
Molecular consequences of PQBP1 deficiency, involved in the X-linked Renpenning syndrome
Molecular Psychiatry (2023)
-
Mapping the landscape of tandem repeat variability by targeted long read single molecule sequencing in familial X-linked intellectual disability
BMC Medical Genomics (2018)
-
Changes in the folding landscape of the WW domain provide a molecular mechanism for an inherited genetic syndrome
Scientific Reports (2016)
-
Downregulation of the Creatine Transporter SLC6A8 by JAK2
The Journal of Membrane Biology (2012)