Abstract
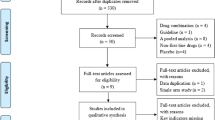
Randomised controlled trials (RCTs) have observed contrasting results on the effects of vitamin C on circulating biomarkers of glycaemic and insulin regulation. We conducted a systematic review and meta-analysis of RCTs testing the effect of vitamin C administration on glucose, HbA1c and insulin concentrations. Four databases (PubMed, Embase, Scopus and Cochrane Library) were used to retrieve RCTs published from inception until April 2016 and testing the effects of vitamin C in adult participants. The screening of 2008 articles yielded 22 eligible studies (937 participants). Overall, vitamin C did not modify glucose, HbA1c and insulin concentrations. However, subgroup analyses showed that vitamin C significantly reduced glucose concentrations (−0.44 mmol/l, 95% CI: −0.81, −0.07, P=0.01) in patients with type 2 diabetes and in interventions with a duration greater than 30 days (−0.53%, 95% CI: −0.79, −0.10, P=0.02). Vitamin C administration had greater effects on fasting (−13.63 pmol/l, 95% CI: −22.73, −4.54, P<0.01) compared to postprandial insulin concentration. Meta-regression analyses showed that age was a modifier of the effect of vitamin C on insulin concentration. Furthermore, the effect size was associated with baseline BMI and plasma glucose levels, and with the duration of the intervention. In conclusion, greater reduction in glucose concentrations observed in patients with diabetes, older individuals and with more prolonged supplementation. Personalised interventions with vitamin C may represent a feasible future strategy to enhance benefits and efficacy of interventions. Nevertheless, results need to be interpreted cautiously due to limitations in the primary studies analysed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Tsilidis KK, Kasimis JC, Lopez DS, Ntzani EE, Ioannidis JP . Type 2 diabetes and cancer: umbrella review of meta-analyses of observational studies. BMJ 2015; 350: g7607.
Garcia-Bailo B, El-Sohemy A, Haddad PS, Arora P, Benzaied F, Karmali M et al. Vitamins D, C, and E in the prevention of type 2 diabetes mellitus: modulation of inflammation and oxidative stress. Biol Targets Ther 2011; 5: 7–19.
Styskal J, Van Remmen H, Richardson A, Salmon AB . Oxidative stress and diabetes: what can we learn about insulin resistance from antioxidant mutant mouse models? Free Radic Biol Med 2012; 52: 46–58.
Padayatty SJ, Katz A, Wang Y, Eck P, Kwon O, Lee JH et al. Vitamin C as an antioxidant: evaluation of its role in disease prevention. J Am Coll Nutr 2003; 22: 18–35.
Carr A, Frei B . Does vitamin C act as a pro-oxidant under physiological conditions? FASEB J 1999; 13: 1007–1024.
Sargeant LA, Wareham NJ, Bingham S, Day NE, Luben RN, Oakes S et al. Vitamin C and hyperglycemia in the European Prospective Investigation into Cancer–Norfolk (EPIC-Norfolk) study: a population-based study. Diabetes Care 2000; 23: 726–732.
Feskens EJ, Virtanen SM, Rasanen L, Tuomilehto J, Stengard J, Pekkanen J et al. Dietary factors determining diabetes and impaired glucose tolerance. A 20-year follow-up of the Finnish and Dutch cohorts of the Seven Countries Study. Diabetes Care 1995; 18: 1104–1112.
Sinclair AJ, Taylor PB, Lunec J, Girling AJ, Barnett AH . Low plasma ascorbate levels in patients with type 2 diabetes mellitus consuming adequate dietary vitamin C. Diabetic Med 1994; 11: 893–898.
Will JC, Ford ES, Bowman BA . Serum vitamin C concentrations and diabetes: findings from the Third National Health and Nutrition Examination Survey, 1988-1994. Am J Clin Nutr 1999; 70: 49–52.
Harding AH, Wareham NJ, Bingham SA, Khaw K, Luben R, Welch A et al. Plasma vitamin C level, fruit and vegetable consumption, and the risk of new-onset type 2 diabetes mellitus: the European prospective investigation of cancer—Norfolk prospective study. Arch Internal Med 2008; 168: 1493–1499.
Song Y, Cook NR, Albert CM, Van Denburgh M, Manson JE . Effects of vitamins C and E and beta-carotene on the risk of type 2 diabetes in women at high risk of cardiovascular disease: a randomized controlled trial. Am J Clin Nutr 2009; 90: 429–437.
Davison GW, Ashton T, George L, Young IS, McEneny J, Davies B et al. Molecular detection of exercise-induced free radicals following ascorbate prophylaxis in type 1 diabetes mellitus: a randomised controlled trial. Diabetologia 2008; 51: 2049–2059.
Ellulu MS, Rahmat A, Patimah I, Khaza'ai H, Abed Y . Effect of vitamin C on inflammation and metabolic markers in hypertensive and/or diabetic obese adults: a randomized controlled trial. Drug Des Devel Ther 2015; 9: 3405–3412.
Gutierrez AD, Duran-Valdez E, Robinson I, de Serna DG, Schade DS . Does short-term vitamin C reduce cardiovascular risk in type 2 diabetes? Endocr Pract 2013; 19: 785–791.
Klein F, Juhl B, Christiansen JS . Unchanged renal haemodynamics following high dose ascorbic acid administration in normoalbuminuric IDDM patients. Scand J Clin Lab Invest 1995; 55: 53–59.
Higgins JPT, Green S . (eds) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011 Available at www.cochrane-handbook.org.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009; 339: b2700.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996; 17: 1–12.
Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A . Meta-analyses involving cross-over trials: methodological issues. Int J Epidemiol 2002; 31: 140–149.
Egger M, Davey Smith G, Schneider M, Minder C . Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315: 629–634.
Higgins JP, Thompson SG, Deeks JJ, Altman DG . Measuring inconsistency in meta-analyses. BMJ 2003; 327: 557–560.
Bhatt JK, Thomas S, Nanjan MJ . Effect of oral supplementation of vitamin C on glycemic control and lipid profile in patients with type 2 diabetes mellitus. Int J Pharm Pharm Sci 2012; 4: 524–527.
Mason SA, Della Gatta PA, Snow RJ, Russell AP, Wadley GD . Ascorbic acid supplementation improves skeletal muscle oxidative stress and insulin sensitivity in people with type 2 diabetes: Findings of a randomized controlled study. Free Radical Biol Med 2016; 93: 227–238.
Bishop N, Schorah CJ, Wales JK . The effect of vitamin C supplementation on diabetic hyperlipidaemia: a double blind, crossover study. Diabet Med 1985; 2: 121–124.
Bo S, Ciccone G, Durazzo M, Gambino R, Massarenti P, Baldi I et al. Efficacy of antioxidant treatment in reducing resistin serum levels: a randomized study. PLoS Clin Trials 2007; 2: e17.
Rafighi Z, Shiva A, Arab S, Mohd Yousof R . Association of dietary vitamin C and e intake and antioxidant enzymes in type 2 diabetes mellitus patients. Glob J Health Sci 2013; 5: 183–187.
Chen H, Karne RJ, Hall G, Campia U, Panza JA, Cannon IRO et al. High-dose oral vitamin C partially replenishes vitamin C levels in patients with Type 2 diabetes and low vitamin C levels but does not improve endothelial dysfunction or insulin resistance. Am J Physiol Heart Circ Physiol 2006; 290: H137–H145.
Dakhale GN, Chaudhari HV, Shrivastava M . Supplementation of vitamin C reduces blood glucose and improves glycosylated hemoglobin in type 2 diabetes mellitus: A randomized, double-blind study. Adv Pharmacol Sci 2011; 2011: 195271.
Gokce N, Keaney Jr JF, Frei B, Holbrook M, Olesiak M, Zachariah BJ et al. Long-term ascorbic acid administration reverses endothelial vasomotor dysfunction in patients with coronary artery disease. Circulation 1999; 99: 3234–3240.
Siavash M, Amini M . Vitamin C may have similar beneficial effects to Gemfibrozil on serum high-density lipoprotein-cholesterol in type 2 diabetic patients. J Res Pharmacy Pract 2014; 3: 77–82.
Johnston CS, Yen MF . Megadose of vitamin C delays insulin response to a glucose challenge in normoglycemic adults. Am j Clin Nutr 1994; 60: 735–738.
Mahmoudabadi MMS, Djalali M, Djazayery SA, Keshavarz SA, Eshraghian MR, Yaraghi AAS et al. Effects of eicosapentaenoic acid and vitamin C on glycemic indices, blood pressure, and serum lipids in type 2 diabetic Iranian males. J Res Med Sci 2011; 16 (SPEC. ISSUE), 361–367.
Mullan BA, Ennis CN, Fee HJ, Young IS, McCance DR . Pretreatment with intravenous ascorbic acid preserves endothelial function during acute hyperglycaemia (R1). Clin Exp Pharmacol Physiol 2005; 32: 340–345.
Nieman DC, Henson DA, McAnulty SR, McAnulty L, Swick NS, Utter AC et al. Influence of vitamin C supplementation on oxidative and immune changes after an ultramarathon. J Appl Physiol 2002; 92: 1970–1977.
Pirbudak L, Balat O, Cekmen M, Ugur MG, Aygun S, Oner U . Effect of ascorbic acid on surgical stress response in gynecologic surgery. Int J Clin Pract 2004; 58: 928–931.
Pleiner J, Schaller G, Mittermayer F, Bayerle-Eder M, Roden M, Wolzt M . FFA-induced endothelial dysfunction can be corrected by vitamin C. J Clin Endocrinol Metab 2002; 87: 2913–2917.
Ghaffari P, Nadiri M, Gharib A, Rahimi F . The effects of vitamin C on diabetic patients. Der Pharmacia Lett 2015; 7: 68–71.
Tousoulis D, Antoniades C, Vasiliadou C, Kourtellaris P, Koniari K, Marinou K et al. Effects of atorvastatin and vitamin C on forearm hyperaemic blood flow, asymmentrical dimethylarginine levels and the inflammatory process in patients with type 2 diabetes mellitus. Heart Br Cardiac Soc 2007; 93: 244–246.
Camargo JL, Stifft J, Gross JL . The effect of aspirin and vitamins C and E on HbA1c assays. Int J Clin Chem 2006; 372: 206–209.
Henriksen EJ, Diamond-Stanic MK, Marchionne EM . Oxidative stress and the etiology of insulin resistance and type 2 diabetes. Free Radic Biol Med 2011; 51: 993–999.
Kim JS, Saengsirisuwan V, Sloniger JA, Teachey MK, Henriksen EJ . Oxidant stress and skeletal muscle glucose transport: roles of insulin signaling and p38 MAPK. Free Radic Biol Med 2006; 41: 818–824.
Ceriello A, Motz E . Is oxidative stress the pathogenic mechanism underlying insulin resistance, diabetes, and cardiovascular disease? The common soil hypothesis revisited. Arterioscler Thromb Vasc Biol 2004; 24: 816–823.
Padayatty SJ, Levine M . Vitamin C: the known, the unknown, and goldilocks. Oral Dis 2016; 22: 463–493.
Mandl J, Szarka A, Banhegyi G . Vitamin C: update on physiology and pharmacology. Br J Pharmacol 2009; 157: 1097–1110.
Will JC, Byers T . Does diabetes mellitus increase the requirement for vitamin C? Nutr Rev 1996; 54: 193–202.
Seghieri G, Martinoli L, Miceli M, Ciuti M, D'Alessandri G, Gironi A et al. Renal excretion of ascorbic acid in insulin dependent diabetes mellitus. Int J Vitam Nutr Res 1994; 64: 119–124.
Hirsch IB, Atchley DH, Tsai E, Labbé RF, Chait A . Ascorbic acid clearance in diabetic nephropathy. J Diabetes Complications 12: 259–263.
Christie-David DJ . effects of vitamins C and D in type 2 diabetes mellitus. Nutr Diet Suppl 2015; 7: 21–28.
Cunningham JJ . The glucose/insulin system and vitamin C: implications in insulin-dependent diabetes mellitus. J Am Coll Nutr 1998; 17: 105–108.
Akbar S, Bellary S, Griffiths HR . Dietary antioxidant interventions in type 2 diabetes patients: a meta-analysis. Br J Diabetes Vasc Dis 2011; 11: 62–68.
Khodaeian M, Tabatabaei-Malazy O, Qorbani M, Farzadfar F, Amini P, Larijani B . Effect of vitamins C and E on insulin resistance in diabetes: a meta-analysis study. Eur J Clin Invest 2015; 45: 1161–1174.
Tabatabaei-Malazy O, Nikfar S, Larijani B, Abdollahi M . Influence of ascorbic acid supplementation on type 2 diabetes mellitus in observational and randomized controlled trials; a systematic review with meta-analysis. J Pharm Pharm Sci 2014; 17: 554–582.
Dietrich M, Block G, Hudes M, Morrow JD, Norkus EP, Traber MG et al. Antioxidant supplementation decreases lipid peroxidation biomarker F(2)-isoprostanes in plasma of smokers. Cancer Epidemiol Biomarkers Prev 2002; 11: 7–13.
Khan F, Ray S, Craigie AM, Kennedy G, Hill A, Barton KL et al. Lowering of oxidative stress improves endothelial function in healthy subjects with habitually low intake of fruit and vegetables: a randomized controlled trial of antioxidant- and polyphenol-rich blackcurrant juice. Free Radic Biol Med 2014; 72: 232–237.
Mark SD, Wang W, Fraumeni Jr JF, Li JY, Taylor PR, Wang GQ et al. Lowered risks of hypertension and cerebrovascular disease after vitamin/mineral supplementation: the Linxian Nutrition Intervention Trial. Am J Epidemiol 1996; 143: 658–664.
Lykkesfeldt J, Poulsen HE . Is vitamin C supplementation beneficial? Lessons learned from randomised controlled trials. Br J Nutr 2010; 103: 1251–1259.
Acknowledgements
AWA is funded by the Republic of Iraq. PROSPERO Database registration: CRD42015023344.
Author contributions
The authors’ were responsible for the following tasks: AWA drafted the manuscript; AWA, JL, MS and JCM conceived the idea for the study and developed the search strategy; AWA, NDW and ADW conducted the search and summarised the data. All authors contributed to the data analysis, verification, writing and revising the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on European Journal of Clinical Nutrition website
Supplementary information
Rights and permissions
About this article
Cite this article
Ashor, A., Werner, A., Lara, J. et al. Effects of vitamin C supplementation on glycaemic control: a systematic review and meta-analysis of randomised controlled trials. Eur J Clin Nutr 71, 1371–1380 (2017). https://doi.org/10.1038/ejcn.2017.24
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2017.24
This article is cited by
-
Empfehlungen zur Ernährung von Personen mit Typ-2-Diabetes mellitus
Die Diabetologie (2024)
-
Empfehlungen zur Ernährung von Personen mit Typ-2-Diabetes mellitus
Die Diabetologie (2023)
-
Vitamin C status and its change in relation to glucose-lipid metabolism in overweight and obesity patients following laparoscopic sleeve gastrectomy
European Journal of Clinical Nutrition (2022)
-
Empfehlungen zur Ernährung von Personen mit Diabetes mellitus Typ 2
Die Diabetologie (2022)
-
Therapeutic effects of dietary antioxidative supplements on the management of type 2 diabetes and its complications; umbrella review of observational/trials meta-analysis studies
Journal of Diabetes & Metabolic Disorders (2022)