Abstract
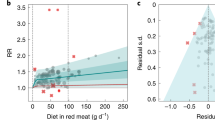
This review summarizes published meta-analysis outcomes on the associations between meat intakes and burden of diseases. A novel assessment process was developed, combining selected Cochrane Review measures, AMSTAR checklist, and other quality measures identified by authors during preliminary phases of the review process. Meat intakes have been found to be statistically significant associated with 21 burden of diseases. A total of 37 risk-outcome best dose–response estimations were identified, all were positively associated, and 21 of them with low to moderate, or insignificant heterogeneity. The highest dose–responses per 50 g increases in processed meat intake at 95% confident levels were 1.81 (1.32, 2.48) for esophageal cancer, 1.71 (1.34, 2.19) for stomach cancer, 1.42 (1.07, 1.89) for CHD, 1.32 (1.19, 1.48) for diabetes, and 1.24 (1.13, 1.35) for colon cancer incidences, and 1.24 (1.09, 1.40) for CVD mortality. The highest dose–responses per each 65 g increases in total red meat intake were 1.36 (1.16, 1.58) for endometrial cancer, 1.25 (1.10, 1.41) esophageal cancer, and 1.22 (1.16, 1.23) for lung cancer incidences. In addition, 14 statistically significant associations in terms of high vs low meat intake relative risks were also identified. Total red meat intakes were found negatively associated with CVD and cancer mortalities, and poultry meat intakes were found negatively associated with all-cause and cancer mortalities, and rectal cancer incidences in low meat consumption Asian countries. Current global and dietary Comparative Risk Assessments may underestimate burden of diseases attributed to meat intakes. More investigation is needed in low-meat consumption countries.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Alexandratos N, Bruinsma J . World agriculture towards 2030/2050: the 2012 revision. ESA Working Paper 2012; 3.
Food Balances [Internet]. Food and Agriculture Organization of the United Nations Statistics Division. 2017. Available from: http://faostat3.fao.org/home/E.
The International Agency for Research on Cancer (IARC) IARC Monographs evaluate consumption of red meat and processed meat [press release]. The Cancer Agency of the World Health Organization: Lyon, France, 2015.
WHO Global status report on noncommunicable diseases 2010. World Health Organization: Italy, 2010.
Garwood P . New WHO report: deaths from noncommunicable diseases on the rise, with developing world hit hardest. World Health Organization. 4 October 2011.
Ezzati M, Hoorn SV, Lopez AD, Danaei G, Rodgers A, Mathers CD et al Comparative quantification of mortality and burden of disease attributable to selected risk factors. in Global Burden of Disease and Risk Factors: The International Bank for Reconstruction and Development/The World Bank. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL (eds). Washington (DC): The International Bank for Reconstruction and Development/The World Bank; 2006. Chapter 4.
Ezzati M, Lopez A, Rodgers A, Murray C . Comparative Quantification of Health risks: Global and Regional Burden of Disease Attributable to Selected Risk Factors. World Health Organization: Geneva, 2004.
Hoorn S, Ezzati M, A R, Lopez A, Murray C Estimating attributable burden of disease from exposure and hazard. In: Ezzati M, Lopez A, Rodgers A, Murray C (eds). Comparative Quantification of Health risks: Global and Regional Burden of Disease Attributable to Selected Risk Factors. World Health Organization: Geneva, 2004; 2129–2140.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2013; 380: 2224–2260.
WCRFI-AICR Food, nutrition, physical activity, and the prevention of cancer: a global perspective. In: World Cancer Research Fund International AIfCR (ed). 2007.
Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Willett WC et al. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. Am J Clin Nutr 2011; 94: 1088–1096.
Micha R, Wallace SK, Mozaffarian D . Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation 2010; 121: 2271–2283.
Feskens EJ, Sluik D, van Woudenbergh GJ . Meat consumption, diabetes, and its complications. Curr Diab Rep 2013; 13: 298–306.
InterAct Consortium. Association between dietary meat consumption and incident type 2 diabetes: the EPIC-InterAct study. Diabetologia 2013; 56: 47–59.
Alexander DD, Miller AJ, Cushing CA, Lowe KA . Processed meat and colorectal cancer: a quantitative review of prospective epidemiologic studies. Eur J Cancer Prev 2010; 19: 328–341.
Chan DS, Lau R, Aune D, Vieira R, Greenwood DC, Kampman E et al. Red and processed meat and colorectal cancer incidence: meta-analysis of prospective studies. PLoS One 2011; 6: e20456.
Abete I, Romaguera D, Vieira AR, Lopez de Munain A, Norat T . Association between total, processed, red and white meat consumption and all-cause, CVD and IHD mortality: a meta-analysis of cohort studies. Br J Nutr 2014; 112: 762–775.
Wang X, Lin X, Ouyang YY, Liu J, Zhao G, Pan A et al. Red and processed meat consumption and mortality: dose-response meta-analysis of prospective cohort studies. Public Health Nutr 2016; 19: 893–905.
Kaluza J, Wolk A, Larsson SC . Red meat consumption and risk of stroke: a meta-analysis of prospective studies. Stroke 2012; 43: 2556–2560.
Chen GC, Lv DB, Pang Z, Liu QF . Red and processed meat consumption and risk of stroke: a meta-analysis of prospective cohort studies. Eur J Clin Nutr 2013; 67: 91–95.
Bandera EV, Kushi LH, Moore DF, Gifkins DM, McCullough ML . Consumption of animal foods and endometrial cancer risk: a systematic literature review and meta-analysis. Cancer Causes Control 2007; 18: 967–988.
Huang W, Han Y, Xu J, Zhu W, Li Z . Red and processed meat intake and risk of esophageal adenocarcinoma: a meta-analysis of observational studies. Cancer Causes Control 2013; 24: 193–201.
Qu X, Ben Q, Jiang Y . Consumption of red and processed meat and risk for esophageal squamous cell carcinoma based on a meta-analysis. Ann Epidemiol 2013; 23: 762–770. e1.
Larsson SC, Wolk A . Red and processed meat consumption and risk of pancreatic cancer: meta-analysis of prospective studies. Br J Cancer 2012; 106: 603–607.
Guo J, Wei W, Zhan L . Red and processed meat intake and risk of breast cancer: a meta-analysis of prospective studies. Breast Cancer Res Treat 2015; 151: 191–198.
Song P, Lu M, Yin Q, Wu L, Zhang D, Fu B et al. Red meat consumption and stomach cancer risk: a meta-analysis. J Cancer Res Clin Oncol 2014; 140: 979–992.
Bonequi P, Meneses-Gonzalez F, Correa P, Rabkin CS, Camargo MC . Risk factors for gastric cancer in Latin America: a meta-analysis. Cancer Causes Control 2013; 24: 217–231.
Zhu H, Yang X, Zhang C, Zhu C, Tao G, Zhao L et al. Red and processed meat intake is associated with higher gastric cancer risk: a meta-analysis of epidemiological observational studies. PLoS One 2013; 8: e70955.
Woo HD, Park S, Oh K, Kim HJ, Shin HR, Moon HK et al. Diet and cancer risk in the Korean population: a meta- analysis. Asian Pacific J Cancer Prev 2014; 15: 8509–8519.
Yang WS, Wong MY, Vogtmann E, Tang RQ, Xie L, Yang YS et al. Meat consumption and risk of lung cancer: evidence from observational studies. Ann Oncol: Off J Eur Soc Med Oncol 2012; 23: 3163–3170.
Xue XJ, Gao Q, Qiao JH, Zhang J, Xu CP, Liu J . Red and processed meat consumption and the risk of lung cancer: a dose-response meta-analysis of 33 published studies. Int J. Clin Exp Med 2014; 7: 1542–1553.
Xu J, Yang XX, Wu YG, Li XY, Bai B . Meat consumption and risk of oral cavity and oropharynx cancer: a meta-analysis of observational studies. PLoS One 2014; 9: e95048.
Aston LM, Smith JN, Powles JW . Impact of a reduced red and processed meat dietary pattern on disease risks and greenhouse gas emissions in the UK: a modelling study. Br Med J 2012; 2: 1–9.
Friel S, Dangour AD, Garnett T, Lock K, Chalabi Z, Roberts I et al. Public health benefits of strategies to reduce greenhouse-gas emissions: food and agriculture. Lancet 2009; 374: 2016–2025.
Scarborough P, Allender S, Clarke D, Wickramasinghe K, Rayner M . Modelling the health impact of environmentally sustainable dietary scenarios in the UK. Eur J Clin Nutr 2012; 66: 710–715.
Springmann M, Godfray HCJ, Rayner M, Scarborough P . Analysis and valuation of the health and climate change cobenefits of dietary change. Proc Natl Acad Sci 2016; 113: 4146–4151.
Yip CSC, Glenis C, Karnon J . Systematic review of reducing population meat consumption to reduce greenhouse gas emissions and obtain health benefits: effectiveness and models assessments. Int J Public Health 2013; 58: 683–693.
MLA, Red Meat, Matters: Fresh red meat is different to processed meat fact 5: Meat & Livestock Australia; 2012 Available from http://www.themainmeal.com.au/NR/rdonlyres/B960B363-4A71-4F18-9E28-CD241F50B3D6/0/Factsheet5FreshvsProcessed_107k.pdf.
Higgins JP, Green S . Cochrane Handbook for Systematic Reviews of Interventions: Wiley Online Library; 2011.
Iorio A, Spencer FA, Falavigna M, Alba C, Lang E, Burnand B et al. Use of GRADE for assessment of evidence about prognosis: rating confidence in estimates of event rates in broad categories of patients. Br Med J 2015; 350: h870.
AMSTAR Checklist [Internet]. http://amstar.ca/ 2015.
NHMRC A Modelling System to Inform the Revision of the Australian Guide to Healthy Eating National Health and Medical Research Council, Department of Health and Ageing, Australian Government; 2011.
Alexander DD, Cushing CA . Quantitative assessment of red meat or processed meat consumption and kidney cancer. Cancer Detect Prev 2009; 32: 340–351.
Alexander DD, Mink PJ, Cushing CA, Sceurman B . A review and meta-analysis of prospective studies of red and processed meat intake and prostate cancer. Nutr J 2010; 9: 50.
Alexander DD, Morimoto LM, Mink PJ, Cushing CA . A review and meta-analysis of red and processed meat consumption and breast cancer. Nutr Res Rev 2010; 23: 349–365.
Alexander DD, Weed DL, Cushing CA, Lowe KA . Meta-analysis of prospective studies of red meat consumption and colorectal cancer. Eur J Cancer Prev 2011; 20: 293–307.
Carr PR, Walter V, Brenner H, Hoffmeister M . Meat subtypes and their association with colorectal cancer: systematic review and meta-analysis. Int J Cancer 2015; 138: 293–302.
Choi Y, Song S, Song Y, Lee JE . Consumption of red and processed meat and esophageal cancer risk: meta-analysis. World J Gastroenterol 2013; 19: 1020–1029.
Fallahzadeh H, Cheraghi M, Amoori N, Alaf M . Red meat intake and risk of non-Hodgkin lymphoma: a meta-analysis. Asian Pacific J Cancer Prev 2014; 15: 10421–10425.
Huxley RR, Ansary-Moghaddam A, Clifton P, Czernichow S, Parr CL, Woodward M . The impact of dietary and lifestyle risk factors on risk of colorectal cancer: a quantitative overview of the epidemiological evidence. Int J Cancer 2009; 125: 171–180.
Kolahdooz F, van der Pols JC, Bain CJ, Marks GC, Hughes MC, Whiteman DC et al. Meat, fish, and ovarian cancer risk: Results from 2 Australian case-control studies, a systematic review, and meta-analysis. Am J Clin Nutr 2010; 91: 1752–1763.
Larsson SC, Orsini N . Red meat and processed meat consumption and all-cause mortality: a meta-analysis. Am J Epidemiol 2013; 179: 282–289.
Larsson SC, Orsini N, Wolk A . Processed meat consumption and stomach cancer risk: a meta-analysis. J Natl Cancer Inst 2006; 98: 1078–1087.
Larsson SC, Wolk A . Meat consumption and risk of colorectal cancer: a meta-analysis of prospective studies. Int J Cancer 2006; 119: 2657–2664.
Lee JE, McLerran DF, Rolland B, Chen Y, Grant EJ, Vedanthan R et al. Meat intake and cause-specific mortality: a pooled analysis of Asian prospective cohort studies. Am J Clin Nutr 2013; 98: 1032–1041.
Li F, An S, Hou L, Chen P, Lei C, Tan W . Red and processed meat intake and risk of bladder cancer: a meta-analysis. Int J Clin Exp Med 2014; 7: 2100.
Liu ZT, Lin AH . Dietary factors and thyroid cancer risk: a meta-analysis of observational studies. Nutr Cancer 2014; 66: 1165–1178.
Luo J, Yang Y, Liu J, Lu K, Tang Z, Liu P et al. Systematic review with meta-analysis: meat consumption and the risk of hepatocellular carcinoma. Aliment Pharmacol Ther 2014; 39: 913–922.
Missmer SA, Smith-Warner SA, Spiegelman D, Yaun SS, Adami HO, Beeson WL et al. Meat and dairy food consumption and breast cancer: a pooled analysis of cohort studies. Int J Epidemiol 2002; 31: 78–85.
Namiranian N, Moradi-Lakeh M, Razavi-Ratki SK, Doayie M, Nojomi M . Risk factors of breast cancer in the Eastern Mediterranean Region: a systematic review and meta-analysis. Asian Pacific J Cancer Prev 2014; 15: 9535–9541.
Norat T, Lukanova A, Ferrari P, Riboli E . Meat consumption and colorectal cancer risk: dose-response meta-analysis of epidemiological studies. Int J Cancer 2002; 98: 241–256.
Pham NM, Mizoue T, Tanaka K, Tsuji I, Tamakoshi A, Matsuo K et al. Meat consumption and colorectal cancer risk: an evaluation based on a systematic review of epidemiologic evidence among the Japanese population. Jpn J Clin Oncol 2014; 44: 641–650.
Rouhani MH, Salehi-Abargouei A, Surkan PJ, Azadbakht L . Is there a relationship between red or processed meat intake and obesity? A systematic review and meta-analysis of observational studies. Obes Rev 2014; 15: 740–748.
Salehi M, Moradi-Lakeh M, Salehi MH, Nojomi M, Kolahdooz F . Meat, fish, and esophageal cancer risk: a systematic review and dose-response meta-analysis. Nutr Rev 2013; 71: 257–267.
Sandhu MS, White IR, McPherson K . Systematic review of the prospective cohort studies on meat consumption and colorectal cancer risk: a meta- analytical approach. Cancer Epidemiol Biomarkers Prev 2001; 10: 439–446.
Smolinska K, Paluszkiewicz P . Risk of colorectal cancer in relation to frequency and total amount of red meat consumption. Systematic review and meta-analysis. Arch Med Sci 2010; 6: 605–610.
Wallin A, Orsini N, Wolk A . Red and processed meat consumption and risk of ovarian cancer: a dose-response meta-analysis of prospective studies. Br J Cancer 2011; 104: 1196–1201.
Wang C, Jiang H . Meat intake and risk of bladder cancer: a meta-analysis. Med Oncol 2012; 29: 848–855.
Wei Y, Zou D, Cao D, Xie P . Association between processed meat and red meat consumption and risk for glioma: a meta-analysis from 14 articles. Nutrition 2015; 31: 45–50.
Xu X, Yu E, Gao X, Song N, Liu L, Wei X et al. Red and processed meat intake and risk of colorectal adenomas: a meta-analysis of observational studies. Int J Cancer 2013; 132: 437–448.
Zhu HC, Yang X, Xu LP, Zhao LJ, Tao GZ, Zhang C et al. Meat consumption is associated with esophageal cancer risk in a meat- and cancer-histological-type dependent manner. Digest Dis Sci 2014; 59: 664–673.
Pan A, Sun Q, Bernstein AM, Manson JE, Willett WC, Hu FB . Changes in red meat consumption and subsequent risk of type 2 diabetes mellitus: three cohorts of US men and women. JAMA Int Med 2013; 173: 1328–1335.
Higgins JP, Green S . Cochrane Handbook for Systematic Reviews of Interventions. Wiley Online Library, 2008.
Scarborough P, Nnoaham K, Clarke D, Rayner M, Capewell S . Modelling the impact of a healthy diet on cardiovascular disease and cancer mortality. J Epidemiol Commun Health 2012; 66: 420–426.
AIHW Australia’s health 2010. Australia’s Health Series no. 12, cat. no. AUS 122. Australian Institute of Health and Welfare: Canberra, 2010.
Nordqvist C . Cut Down On Red Meat And Processed Meat To Reduce Cancer Risk. 2011.
Wyness L, Weichselbaum E, O’Connor A, Williams EB, Benelam B, Riley H et al. Red meat in the diet: an update. Nutr Bull 2011; 36: 34–77.
NHMRC. Nutrient Reference Values for Australia and New Zealand Including Recommended Dietary Intakes. National Health and Medical Research Council 2006; 12: 853–861.
Kinjo Y, Beral V, Akiba S, Key T, Mizuno S, Appleby P . Possible protective effect of milk, meat and fish for cerebrovascular disease mortality in Japan. J Epidemiol 1999; 9: 268–274.
Sauvaget CM, Nagano JM, Hayashi MB, Yamada MM . Animal protein, animal fat, and cholesterol intakes and risk of cerebral infarction mortality in the Adult Health Study. Stroke J Cerebr Circul 2004; 35: 1531–1537.
Yamagishi K, Iso H, Yatsuya H, Tanabe N, Date C, Kikuchi S et al. Dietary intake of saturated fatty acids and mortality from cardiovascular disease in Japanese: the Japan Collaborative Cohort Study for Evaluation of Cancer Risk (JACC) Study1–3. Am J Clin Nutr 2010; 92: 759–765.
Chen K, Jin M . Mortality, biochemistry, diet and lifestyle in rural China: geographic study of the characteristics of 69 counties in mainland China and 16 areas in Taiwan. Oxford University Press: Oxford, 2006.
Dinu M, Abbate R, Gensini GF, Casini A, Sofi F . Vegetarian, vegan diets and multiple health outcomes: a systematic review with meta-analysis of observational studies. Critic Rev Food Sci Nutr 2016; 57: 3640–3649.
Kudlackova M, Valachovicova M, Babinska K, Krivosikova Z, Paukova V, Spustova V et al. Possible health risks in subjects with dominant plant food consumption. J Cent Eur Agric 2013; 14: 894–904.
McConnell T, Appleby P, Key T . Vegetarian diet as a risk factor for symptomatic gallstone disease. Eur J Clin Nutr 2017; 71: 731–735.
Bech-Larsen T, Kazbare L . Perceptions of healthy eating in transitional phases of life: results of four focus groups with adolescents and older adults. Br Food J 2014; 116: 570–584.
Font-i-Furnols M, Guerrero L . Consumer preference, behavior and perception about meat and meat products: an overview. Meat Sci 2014; 98: 361–371.
Köster EP . Diversity in the determinants of food choice: a psychological perspective. Food Quality Preference 2009; 20: 70–82.
Brownie S, Coutts R . Older Australians’ perceptions and practices in relation to a healthy diet for old age: a qualitative study. J Nutr Health Aging 2013; 17: 125–129.
Charlebois S, Charlebois S, McCormick M, McCormick M, Juhasz M, Juhasz M . Meat consumption and higher prices: Discrete determinants affecting meat reduction or avoidance amidst retail price volatility. Br Food J 2016; 118: 2251–2270.
Piazza J, Ruby MB, Loughnan S, Luong M, Kulik J, Watkins HM et al. Rationalizing meat consumption. The 4Ns. Appetite 2015; 91: 114–128.
Jensen M, Heilmann T, Hedegaard Hansen JA, Rasmussen JL, Mølgaard IN, Fisker-Clausen R et al Meat consumption among Danish men 2016.
Pohjolainen P, Vinnari M, Jokinen P . Consumers’ perceived barriers to following a plant-based diet. Br Food J 2015; 117: 1150–1167.
Schösler H, De Boer J, Boersema JJ . Can we cut out the meat of the dish? Constructing consumer-oriented pathways towards meat substitution. Appetite 2012; 58: 39–47.
WCRFI. Limit consumption of red meats (such as beef, pork and lamb) and avoid processed meats: World Cancer Research Fund International 2016 Available from http://www.wcrf.org/int/research-we-fund/cancer-prevention-recommendations/animal-foods.
US Department of Agriculture (USDA)Dietary guidelines for Americans, 2010. In UDoH Human Services. ed., US Government Printing Office: Washington, DC, 2010.
DHUK. The eatwell plate: Department of Health, UK; 2011. Available from http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Publichealth/Nutrition/DH_126493#_5.
Yip CSC, Fielding R . Health and greenhouse gas emission implication of reducing meat intakes in Hong Kong. World Acad Sci Eng Technol Int J Biol Biomol Agric Food Biotechnol Eng 2017.
Kim HJ, Lim SY, Lee JS, Park S, Shin A, Choi BY et al. Fresh and pickled vegetable consumption and gastric cancer in Japanese and Korean populations: a meta-analysis of observational studies. Cancer Sci 2010; 101: 508–516.
Acknowledgements
We thank Sai Yin Ho, Linwei Tian and Lai Ming Ho for epidemiology and biostatistics advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on European Journal of Clinical Nutrition website
Supplementary information
Rights and permissions
About this article
Cite this article
Yip, C., Lam, W. & Fielding, R. A summary of meat intakes and health burdens. Eur J Clin Nutr 72, 18–29 (2018). https://doi.org/10.1038/ejcn.2017.117
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2017.117
This article is cited by
-
Global burden of ischemic heart disease associated with high red and processed meat consumption: an analysis of 204 countries and territories between 1990 and 2019
BMC Public Health (2023)
-
Changes in global food consumption increase GHG emissions despite efficiency gains along global supply chains
Nature Food (2023)
-
Sustainable meat consumption: global and regional greenhouse gas emission implications and counterfactual scenario analyses
Environment, Development and Sustainability (2023)