Abstract
Background/Objectives:
Low serum ferritin concentrations at birth, which reflect neonatal iron stores, track through to early childhood and have been associated with poorer neurodevelopmental outcomes. We aimed to identify maternal, antenatal and birth-associated factors that influence iron stores at birth in a prospective maternal–infant birth cohort.
Subjects/Methods:
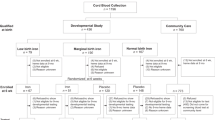
In a population-based, longitudinal, birth cohort in Ireland, 413 maternal–infant dyads with prospectively collected lifestyle and clinical data from 15 weeks’ gestation had umbilical cord serum ferritin concentrations measured. Regression models were developed to identify independent factors associated with cord ferritin concentrations.
Results:
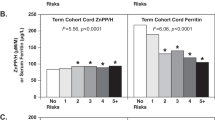
Median (IQR) cord ferritin concentrations were 185.7 (131.7, 385.5) μg/l, and 8% (n=33) of infants had low iron stores (ferritin <76 μg/l) at birth. Maternal obesity (BMI ⩾30 kg/m2) at 15 weeks’ gestation (adj. estimate (95% confidence interval (CI)): −66.4 (−106.9, −25.9) μg/l, P<0.0001) and delivery by caesarean section (−38.8 (−70.2, −7.4) μg/l, P=0.016) were inversely associated with cord ferritin concentrations. In addition, maternal smoking at 15 weeks’ gestation (adj. odds ratio (95% CI): 2.9 (1.2, 7), P=0.020) and being born small-for-gestational age (3.4 (1.3, 8.9), P=0.012) were associated with an increased risk of low iron stores (ferritin <76 μg/l) at birth.
Conclusions:
We have identified a number of potentially modifiable lifestyle factors that influence iron stores at birth, with the important role of overall maternal health and lifestyle during pregnancy highlighted. Public health policies targeting women of child-bearing age to improve nutrition and health outcomes should be prioritised for the health of the next generation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Domellof M, Braegger C, Campoy C, Colomb V, Decsi T, Fewtrell M et al. Iron requirements of infants and toddlers. J Pediatr Gastroenterol Nutr 2014; 58: 119–129.
Wintergerst ES, Maggini S, Hornig DH . Contribution of selected vitamins and trace elements to immune function. Ann Nutr Metab 2007; 51: 301–323.
Georgieff MK . Long-term brain and behavioral consequences of early iron deficiency. Nutr Rev 2011; 69: S43–S48.
Lozoff B, Beard J, Connor J, Barbara F, Georgieff M, Schallert T . Long-lasting neural and behavioral effects of iron deficiency in infancy. Nutr Rev 2006; 64: S34–S43.
Lozoff B, Smith JB, Kaciroti N, Clark KM, Guevara S, Jimenez E . Functional significance of early-life iron deficiency: outcomes at 25 years. J Pediatr 2013; 163: 1260–1266.
Siimes MA, Addiego JE Jr, Dallman PR . Ferritin in serum: diagnosis of iron deficiency and iron overload in infants and children. Blood 1974; 43: 581–590.
MacPhail AP, Charlton RW, Bothwell TH, Torrance JD . The relationship between maternal and infant iron status. Scand J Haematol 1980; 25: 141–150.
Georgieff MK, Wewerka SW, Nelson CA, Deregnier RA . Iron status at 9 months of infants with low iron stores at birth. J Pediatr 2002; 141: 405–409.
Hay G, Refsum H, Whitelaw A, Melbye EL, Haug E, Borch-Iohnsen B . Predictors of serum ferritin and serum soluble transferrin receptor in newborns and their associations with iron status during the first 2 y of life. Am J Clin Nutr 2007; 86: 64–73.
Tamura T, Goldenberg RL, Hou J, Johnston KE, Cliver SP, Ramey SL et al. Cord serum ferritin concentrations and mental and psychomotor development of children at five years of age. J Pediatr 2002; 140: 165–170.
Siddappa AM, Georgieff MK, Wewerka S, Worwa C, Nelson CA, Deregnier RA . Iron deficiency alters auditory recognition memory in newborn infants of diabetic mothers. Pediatr Res 2004; 55: 1034–1041.
Rao R, Georgieff MK . Neonatal iron nutrition. Semin Neonatol 2001; 6: 425–435.
Kenny LC, Black MA, Poston L, Taylor R, Myers JE, Baker PN et al. Early pregnancy prediction of preeclampsia in nulliparous women, combining clinical risk and biomarkers: the Screening for Pregnancy Endpoints (SCOPE) international cohort study. Hypertension 2014; 64: 644–652.
North RA, McCowan LM, Dekker GA, Poston L, Chan EH, Stewart AW et al. Clinical risk prediction for pre-eclampsia in nulliparous women: development of model in international prospective cohort. Brit Med J 2011; 342: d1875.
O'Donovan SM, Murray DM, Hourihane JO, Kenny LC, Irvine AD, Kiely M . Cohort profile: the Cork BASELINE Birth Cohort Study: babies after SCOPE: evaluating the longitudinal impact on neurological and nutritional endpoints. Int J Epidemiol 2015; 44: 764–775.
World Health Organisation Iron Deficiency Anaemia. Assessment, Prevention and Control. A Guide for Programme Managers. WHO: Geneva, Switzerland, 2001.
Masukume G, Khashan AS, Kenny LC, Baker PN, Nelson G . Risk factors and birth outcomes of anaemia in early pregnancy in a nulliparous cohort. PLoS One 2015; 10: e0122729.
McCowan LM, Thompson JM, Taylor RS, North RA, Poston L, Baker PN et al. Clinical prediction in early pregnancy of infants small for gestational age by customised birthweight centiles: findings from a healthy nulliparous cohort. PLoS One 2013; 8: e70917.
World Health Organisation/Centers for Disease Control and Prevention. Assessing the Iron Status of Populations. WHO: Geneva, Switzerland, 2004.
Poston L, Harthoorn LF, Van Der Beek EM . Obesity in pregnancy: implications for the mother and lifelong health of the child. A consensus statement. Pediatr Res 2011; 69: 175–180.
Shao J, Lou J, Rao R, Georgieff MK, Kaciroti N, Felt BT et al. Maternal serum ferritin concentration is positively associated with newborn iron stores in women with low ferritin status in late pregnancy. J Nutr 2012; 142: 2004–2009.
Chockalingam UM, Murphy E, Ophoven JC, Weisdorf SA, Georgieff MK . Cord transferrin and ferritin values in newborn infants at risk for prenatal uteroplacental insufficiency and chronic hypoxia. J Pediatr 1987; 111: 283–286.
Chelchowska M, Laskowska-Klita T . Effect of maternal smoking on some markers of iron status in umbilical cord blood. Rocz Akad Med Bialymst 2002; 47: 235–240.
Morton SB, Saraf R, Bandara DK, Bartholomew K, Gilchrist CA, Atatoa Carr PE et al. Maternal and perinatal predictors of newborn iron status. N Z Med J 2014; 127: 62–77.
McLimore HM, Phillips AK, Blohowiak SE, Pham DQ, Coe CL, Fischer BA et al. Impact of multiple prenatal risk factors on newborn iron status at delivery. J Pediatr Hematol Oncol 2013; 35: 473–477.
Colomer J, Colomer C, Gutierrez D, Jubert A, Nolasco A, Donat J et al. Anaemia during pregnancy as a risk factor for infant iron deficiency: report from the Valencia Infant Anaemia Cohort (VIAC) study. Paediatr Perinat Epidemiol 1990; 4: 196–204.
Sweet DG, Savage G, Tubman TR, Lappin TR, Halliday HL . Study of maternal influences on fetal iron status at term using cord blood transferrin receptors. Arch Dis Child Fetal Neonatal Ed 2001; 84: F40–F43.
Jaime-Perez JC, Herrera-Garza JL, Gomez-Almaguer D . Sub-optimal fetal iron acquisition under a maternal environment. Arch Med Res 2005; 36: 598–602.
Dao MC, Sen S, Iyer C, Klebenov D, Meydani SN . Obesity during pregnancy and fetal iron status: is Hepcidin the link? J Perinatol 2013; 33: 177–181.
Phillips AK, Roy SC, Lundberg R, Guilbert TW, Auger AP, Blohowiak SE et al. Neonatal iron status is impaired by maternal obesity and excessive weight gain during pregnancy. J Perinatol 2014; 34: 513–518.
Garcia-Valdes L, Campoy C, Hayes H, Florido J, Rusanova I, Miranda MT et al. The impact of maternal obesity on iron status, placental transferrin receptor expression and hepcidin expression in human pregnancy. Int J Obes 2015; 39: 571–578.
Jones AD, Zhao G, Jiang YP, Zhou M, Xu G, Kaciroti N et al. Maternal obesity during pregnancy is negatively associated with maternal and neonatal iron status. Eur J Clin Nutr 2016; 70: 918–924.
Rao R, Georgieff MK . Iron in fetal and neonatal nutrition. Semin Fetal Neonatal Med 2007; 12: 54–63.
Zhou YB, Li HT, Zhu LP, Liu JM . Impact of cesarean section on placental transfusion and iron-related hematological indices in term neonates: a systematic review and meta-analysis. Placenta 2014; 35: 1–8.
Pisacane A . Neonatal prevention of iron deficiency. Br Med J 1996; 312: 136–137.
Andersson O, Hellstrom-Westas L, Andersson D, Domellof M . Effect of delayed versus early umbilical cord clamping on neonatal outcomes and iron status at 4 months: a randomised controlled trial. Br Med J 2011; 343: d7157.
World Health Organisation. Guideline: Delayed Umbilical Cord Clamping for Improved Maternal and Infant Health and Nutrition Outcomes. WHO: Geneva, Switzerland, 2014.
National Institute for Health and Care Excellence.. Intrapartum care: care of healthy women and their babies during childbirth. National Institute for Health and Care Excellence. BMJ 2014; 249: g6886.
Khashan AS, Kenny LC . The effects of maternal body mass index on pregnancy outcome. Eur J Epidemiol 2009; 24: 697–705.
Acknowledgements
We thank the participants and their families for their continued support, and both the SCOPE Ireland and Cork BASELINE Birth Cohort Study research teams. Funding A grant from the National Children’s Research Centre to DMM, JOBH, ADI, LCK and MEK is the primary funding source for the Cork BASELINE Birth Cohort Study. Additional support came from grants from the UK Food Standards Agency to JOBH and ADI and from Danone Nutricia Early Life Nutrition to MEK and DMM. The SCOPE Ireland Study was funded by a grant from the Health Research Board of Ireland (CSA 02/2007) to LCK. The INFANT Research Centre is Science Foundation Ireland funded (Grant No. 12/RC/2272). No funding agencies had any role in the design, analysis or writing of this article.
Author contributions
EKM carried out data collection, database construction and data analysis. EKM and MEK designed the study and drafted the manuscript. DMM is the overall principal investigator (PI) of the Cork BASELINE Birth Cohort Study; and JOBH, LCK, ADI and MEK are co-PIs and specialist leads. LCK is the PI of the SCOPE Ireland pregnancy cohort study. All authors reviewed and approved the final submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
McCarthy, E., Kenny, L., Hourihane, J. et al. Impact of maternal, antenatal and birth-associated factors on iron stores at birth: data from a prospective maternal–infant birth cohort. Eur J Clin Nutr 71, 782–787 (2017). https://doi.org/10.1038/ejcn.2016.255
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2016.255
This article is cited by
-
Association of cesarean delivery on maternal request with neonatal iron stores at birth
European Journal of Clinical Nutrition (2021)
-
Baseline iron and low-grade inflammation modulate the effectiveness of iron supplementation: evidence from follow-up of pregnant Sri Lankan women
European Journal of Nutrition (2021)