Abstract
Background/Objectives:
Recent research has speculated that the risk of developing atherosclerosis is due to the accumulation of the effects of daily diet choices. The purpose of this study was to examine which of our previously identified preclinical disease risk biomarkers were further elevated when consuming a high-fat (644±50 kcal; 100% recommended dietary allowance for fat), high-calorie (1118±100 kcal; 70% daily caloric needs) breakfast on consecutive days. Young, normal weight females (N=7) participated in this study.
Subjects/Methods:
Blood samples were taken premeal and hourly for 5-h postprandial. Serum biomarkers (C-peptide, eotaxin, gastric inhibitory polypeptide, granulocyte colony-stimulating factor (G-CSF), granulocyte-monocyte colony-stimulating factor (GM-CSF), insulin, leptin, monocyte chemoattractant protein 1, pancreatic polypeptide (PPY) and tumor necrosis factor-α), monocyte concentration, and adhesion molecule expression (CD11a, CD18 and CD54) were measured. Area under the curve was calculated for each outcome variable as a function of day and data were analyzed for significance.
Results:
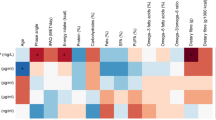
We found significant (P<0.05) increases on Day 2 for: GM-CSF (+47%; P=0.041), G-CSF (+31%; P=0.012), PPY (+51%; P=0.049), total monocyte (+110%; P=0.043), pro-inflammatory (PI) monocyte (+60%; P=0.012), PI monocyte CD18 (+960%; P=0.003), PI monocyte CD11a (+230%; P=0.006), and PI monocyte CD54 (+208%; P=0.015).
Conclusions:
To our knowledge, the present study is the first to report changes in selected biomarkers and monocytes following eating a high-fat, high-calorie breakfast on consecutive days in humans. More research is needed to determine how transient the observed changes are and what the long-term implications for disease risk are.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Scheffer PG, Tushuizen ME, Vermue HP, Schindhelm RK, Rustemeijer C, Diamant M . Effect of three consecutive meals on the physicochemical properties of HDL and LDL in individuals with the metabolic syndrome and patients with type 2 diabetes. Eur J Clin Nutr 2011; 65: 1242–1249.
Tushuizen ME, Nieuwland R, Scheffer PG, Sturk A, Heine RJ, Diamant M . Two consecutive high-fat meals affect endothelial-dependent vasodilation, oxidative stress and cellular microparticles in healthy men. J Thromb Haemost 2006; 4: 1003–1010.
McFarlin BK, Carpenter KC, Venable AS, Prado EA, Henning AL . Consumption of a high-fat breakfast on consecutive days alters area-under-the-curve for selected cardiovascular disease biomarkers. J Mol Pathophysiol 2015; 4: 6.
Strohacker K, Breslin WL, Carpenter KC, Davidson TR, Agha NH, McFarlin BK . Moderate-intensity, premeal cycling blunts postprandial increases in monocyte cell surface CD18 and CD11a and endothelial microparticles following a high-fat meal in young adults. Appl Physiol Nutr Metab 2012; 37: 530–539.
Strohacker K, McFarlin BK . Influence of obesity, physical inactivity, and weight cycling on chronic inflammation. Front Biosci (Elite Ed) 2010; 2: 98–104.
Astrup A . Dietary management of obesity. JPEN J Parenter Enteral Nutr 2008; 32: 575–577.
Ferrara LA, Capaldo B, Mancusi C, Lee ET, Howard BV, Devereux RB et al. Cardiometabolic risk in overweight subjects with or without relative fat-free mass deficiency: the Strong Heart Study. Nutr Metab Cardiovasc Dis 2013; 24: 271–276.
Herieka M, Erridge C . High-fat meal induced postprandial inflammation. Mol Nutr Food Res 2014; 58: 136–146.
Raz O, Steinvil A, Berliner S, Rosenzweig T, Justo D, Shapira I . The effect of two iso-caloric meals containing equal amounts of fats with a different fat composition on the inflammatory and metabolic markers in apparently healthy volunteers. J Inflamm 2013; 10: 3.
Teeman CS, Kurti SP, Cull BJ, Emerson SR, Haub MD, Rosenkranz SK . The effect of moderate intensity exercise in the postprandial period on the inflammatory response to a high-fat meal: an experimental study. Nutr J 2016; 15: 24.
Carpenter KC, Strohacker K, McFarlin BK . Considerations to maximize fat mass gain in a mouse model of diet-induced weight gain. Lab Anim 2013; 47: 266–273.
Strohacker K, Breslin WL, Carpenter KC, McFarlin BK . Aged mice have increased inflammatory monocyte concentration and altered expression of cell-surface functional receptors. J Biosci 2012; 37: 55–62.
Pamir N, Liu NC, Irwin A, Becker L, Peng Y, Ronsein GE et al. Granulocyte/macrophage colony-stimulating factor-dependent dendritic cells restrain lean adipose tissue expansion. J Biol Chem 2015; 290: 14656–14667.
Navarro A, Marin S, Riol N, Carbonell-Uberos F, Minana MD . Human adipose tissue-resident monocytes exhibit an endothelial-like phenotype and display angiogenic properties. Stem Cell Res Ther 2014; 5: 50.
McFarlin BK, Venable AS, Henning AL, Prado EA, Best Sampson JN, Vingren JL et al. Natural cocoa consumption: potential to reduce atherogenic factors? J Nutr Biochem 2015; 26: 626–632.
Henning AL, Venable AS, Prado EA, Best Sampson JN, McFarlin BK . Using image-based flow cytometry to measure monocyte oxidized LDL phagocytosis: a potential risk factor for CVD? J Immunol Methods 2015; 423: 78–84.
McFarlin BK, Johnston CJ, Carpenter KC, Davidson T, Moreno JL, Strohacker K et al. A one-year school-based diet/exercise intervention improves non-traditional disease biomarkers in Mexican-American children. Matern Child Nutr 2013; 9: 524–532.
McFarlin BK, Johnson CA, Moreno JP, Foreyt JP . Mexican American children have differential elevation of metabolic biomarkers proportional to obesity status. J Pediatr Gastroenterol Nutr 2013; 57: 718–721.
Breslin WL, Johnston CA, Strohacker K, Carpenter KC, Davidson TR, Moreno JP et al. Obese Mexican American children have elevated MCP-1, TNF-alpha, monocyte concentration, and dyslipidemia. Pediatrics 2012; 129: e1180–e1186.
McFarlin BK, Johnston CA, Tyler C, O'Connor DP, Strohacker KA, Reeves R et al. Relation between adiposity and disease risk factors in Mexican American children. J Pediatr Gastroenterol Nutr 2009; 49: 450–455.
Kueht ML, McFarlin BK, Lee RE . Severely obese have greater LPS-stimulated TNF-alpha production than normal weight African-American women. Obesity (Silver Spring) 2009; 17: 447–451.
McFarlin BK, Venable AS . Measurement of low concentration human serum cytokines using a Millipore high-sensitivity Milliplex assay. J Vis Exp 2014,. Available at: https://www.jove.com/video/5088/measurement-low-concentration-human-serum-cytokines-using-millipore.
Carpenter KC, Breslin WL, Davidson T, Adams A, McFarlin BK . Baker's yeast beta-glucan supplementation increases monocytes and cytokines post-exercise: implications for infection risk? Br J Nutr 2013; 109: 478–486.
Perez-Martinez P, Alcala-Diaz J, Delgado-Lista J, Garcia-Rios A, Gomez-Delgado F, Marin-Hinojosa C et al. Metabolical phenotypes of obesity influence triglyceride and inflammation homeostasis. Eur J Clin Invest 2014; 44: 1053–1064.
Aoi W, Yamauchi H, Iwasa M, Mune K, Furuta K, Tanimura Y et al. Combined light exercise after meal intake suppresses postprandial serum triglyceride. Med Sci Sports Exerc 2013; 45: 245–252.
Kim DH, Sandoval D, Reed JA, Matter EK, Tolod EG, Woods SC et al. The role of GM-CSF in adipose tissue inflammation. Am J Physiol Endocrinol Metab 2008; 295: E1038–E1046.
McFarlin BK, Carpenter KC, Strohacker K, Breslin WL . Comparison of blood monocytes and adipose tissue macrophages in a mouse model diet-induced weight gain. Comp Med 2012; 62: 462–465.
Carpenter KC, Strohacker K, Breslin WL, Lowder TW, Agha NH, McFarlin BK . Effects of exercise on weight loss and monocytes in obese mice. Comp Med 2012; 62: 21–26.
Sam AH, Sleeth ML, Thomas EL, Ismail NA, Mat Daud N, Chambers E et al. Circulating pancreatic polypeptide concentrations predict visceral and liver fat content. J Clin Endocrinol Metab 2015; 100: 1048–1052.
Kursawe R, Dixit VD, Scherer PE, Santoro N, Narayan D, Gordillo R et al. A role of the inflammasome in the low storage capacity of the abdominal subcutaneous adipose tissue in obese adolescents. Diabetes 2016; 65: 610–618.
Acknowledgements
This project was funded in part by grant to Dr McFarlin from the University of North Texas (RIG Program) and a TACSM Student Research Development Grant (SRDA) to Dr Carpenter. We also thank Ms Jill Best Sampson (calculation of AUC values for the biomarker responses) and Dr Erin Bowman (editorial advice) for their assistance with the present study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
McFarlin, B., Carpenter, K., Henning, A. et al. Consumption of a high-fat breakfast on consecutive days alters preclinical biomarkers for atherosclerosis. Eur J Clin Nutr 71, 239–244 (2017). https://doi.org/10.1038/ejcn.2016.242
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2016.242
This article is cited by
-
Acute, but not chronic, aerobic exercise alters the impact of ex vivo LDL and fatty acid stimulation on monocytes and macrophages from healthy, young adults
European Journal of Applied Physiology (2023)
-
Prebiotic/probiotic supplementation resulted in reduced visceral fat and mRNA expression associated with adipose tissue inflammation, systemic inflammation, and chronic disease risk
Genes & Nutrition (2022)
-
Breakfast skipping and prevalence of heartburn syndrome among Iranian adults
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2021)
-
Effect of food intake on 92 oncological biomarkers by the Proseek Oncology II panel
BMC Research Notes (2019)