Abstract
BACKGROUND/OBJECTIVES:
Although malnutrition commonly affects stroke patients, there are no validated screening tools. We verified the usefulness of non-paralytic anthropometric measurements for the nutritional screening of stroke.
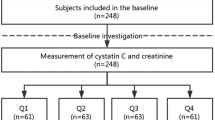
SUBJECTS/METHODS:
A cross-sectional study was conducted in consecutive stroke patients with hemiplegia aged ⩾65 years, with Mini Nutritional Assessment Short Form score ⩽11. Diagnostic malnutrition criteria from the European Society for Clinical Nutrition and Metabolism were the reference standards: body mass index (BMI) <18.5 kg/m2 or weight loss >10%+BMI <22 or 20 kg/m2. Non-paralytic anthropometric measurements (calf circumference (CC), arm circumference (AC), triceps skinfold (TSF) and arm muscle circumference (AMC)) and serum albumin concentration (Alb) at admission were the index tests. Cutoffs were determined by receiver operation curve and Youden index, and accuracy by area under the curve (AUC) and kappa value. Functional independence measures at discharge and discharge destination were collected.
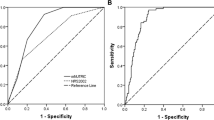
RESULTS:
We included 488 patients (224 men and 264 women) with a mean age of 78.8 years and mean BMI of 22.0 and 21.1 kg/m2, respectively. Eighty-one men and 124 women had malnutrition. The AUC for CC, AC, TSF, AMC and Alb was 0.859, 0.825, 0.764, 0.745 and 0.670 for men, and 0.881, 0.843, 0.796, 0.742 and 0.658 for women, respectively. In both sexes, CC had the highest kappa (0.533, 0.608; both P<0.001) with cutoff values ⩽31 and ⩽30 cm. Patients with lower CC showed significantly worse functional outcomes and lower proportion of return to home (P<0.001).
CONCLUSIONS:
Non-paralytic CC indicated malnutrition with sufficient accuracy and good correlation with functional capacity; it may be a useful nutritional screening tool for stroke.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
World Health Organization. The Global Burden of Disease: 2004 Update. 2014 http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/ (accessed May 2016).
Ministry of Health, Labour and Welfare of Japan. Comprehensive Survey of Living Conditions. 2013 http://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa13/dl/05.pdf (accessed May 2016). [In Japanese].
The FOOD Trial Collaboration. Poor nutritional status on admission predicts poor outcomes after stroke: observational data from the FOOD trial. Stroke 2003; 34: 1450–1456.
Davalos A, Ricart W, Gonzalez-Huix F, Soler S, Marrugat J, Molins A et al. Effect of malnutrition after acute stroke on clinical outcome. Stroke 1996; 27: 1028–1032.
Nishioka S, Takayama M, Watanabe M, Urushihara M, Kiriya Y, Hijioka S . Prevalence of malnutrition in convalescent rehabilitation wards in Japan and correlation of malnutrition with ADL and discharge outcome in elderly stroke patients. J Jpn Soc Parenter Enteral Nutr 2015; 30: 1145–1151. [In Japanese].
Kokura Y, Maeda K, Wakabayashi H, Nishioka S, Higashi S . High nutritional-related risk on admission predicts less improvement of functional independence measure in geriatric stroke patients: a retrospective cohort study. J Stroke Cerebrovasc Dis 2016; 25: 1335–1341.
Nii M, Maeda K, Wakabayashi H, Nishioka S, Tanaka A . Nutritional improvement and energy intake are associated with functional recovery in patients after cerebrovascular disorders. J Stroke Cerebrovasc Dis 2016; 25: 57–62.
Nishioka S, Wakabayashi H, Nishioka E, Yoshida T, Mori N, Watanabe R . Nutritional improvement correlates with recovery of activities of daily living among malnourished elderly stroke patients in the convalescent stage: a cross-sectional study. J Acad Nutr Diet 2016; 116: 837–843.
Foley NC, Salter KL, Robertson J, Teasell R, Gail M . Which reported estimate of the prevalence of malnutrition after stroke is valid? Stroke 2009; 40: e66–e74.
Peters L, O'Connor C, Giroux I, Teasell R, Foley N . Screening and assessment of nutritional status following stroke: results from a national survey of registered dietitians in Canada. Disabil Rehabil 2015; 37: 2413–2417.
Hirsch S, de Obaldia N, Petermann M, Rojo P, Barrientos C, Iturriaga H et al. Subjective global assessment of nutritional status: further validation. Nutrition 1991; 7: 35–37.
Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, Klek S . Diagnostic criteria for malnutrition – an ESPEN consensus statement. Clin Nutr 2015; 34: 335–340.
Doehner W, Schenkel J, Anker SD, Springer J, Audebert H . Overweight and obesity are associated with improved survival, functional outcome, and stroke recurrence after acute stroke or transient ischaemic attack: observations from the TEMPiS trial. Eur Heart J 2013; 34: 268–277.
Olsen TS, Dehlendorff C, Petersen HG, Andersen KK . Body mass index and poststroke mortality. Neuroepidemiology 2008; 30: 93–100.
Leandro-Merhi VA, de Aquino JL, de Camargo JG . Agreement between body mass index, calf circumference, arm circumference, habitual energy intake and the MNA in hospitalized elderly. J Nutr Health Aging 2012; 16: 128–132.
Bonnefoy M, Jauffret M, Kostka T, Jusot JF . Usefulness of calf circumference measurement in assessing the nutritional state of hospitalized elderly people. Gerontology 2002; 48: 162–169.
Nishioka S, Wakabayashi H, Yoshida T, Mori N, Watanbe R, Nishioka E . Obese Japanese patients with stroke have higher functional recovery in convalescent rehabilitation wards: a retrospective cohort study. J Stroke Cerebrovasc Dis 2016; 25: 26–33.
Miyai I, Sonoda S, Nagai S, Takayama Y, Inoue Y, Kakehi A et al. Results of new policies for inpatient rehabilitation coverage in Japan. Neurorehabil Neural Repair 2011; 25: 540–547.
Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging 2009; 13: 782–788.
Shimomura Y, Katsuura T . [Ergonomic design of calf circumference measuring tape for assessing nutritional status]. Ningen Kogaku 2012; 48: 1–6. [Article in Japanese].
Chumney D, Nollinger K, Shesko K, Skop K, Spencer M, Newton RA . Ability of functional independence measure to accurately predict functional outcome of stroke-specific population: systematic review. J Rehabil Res Dev 2010; 47: 17–29.
Youden WJ . Index for rating diagnostic tests. Cancer 1950; 3: 32–35.
Landis JR, Koch GG . The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–174.
Portero-McLellan KC, Staudt C, Silva FR, Delbue Bernardi JL, Baston Frenhani P et al. The use of calf circumference measurement as an anthropometric tool to monitor nutritional status in elderly inpatients. J Nutr Heal Aging 2010; 14: 266–270.
Wijnhoven HA, van Bokhorst-de van der Schueren MA, Heymans MW, de Vet HC, Kruizenga HM, Twisk JW et al. Low mid-upper arm circumference, calf circumference, and body mass index and mortality in older persons. J Gerontol A Biol Sci Med Sci 2010; 65: 1107–1114.
Landi F, Onder G, Russo A, Liperoti R, Tosato M, Martone AM et al. Calf circumference, frailty and physical performance among older adults living in the community. Clin Nutr 2014; 33: 539–544.
Kawakami R, Murakami H, Sanada K, Tanaka N, Sawada SS, Tabata I et al. Calf circumference as a surrogate marker of muscle mass for diagnosing sarcopenia in Japanese men and women. Geriatr Gerontol Int 2015; 15: 969–976.
Velazquez-Alva M, Irigoyen Camacho M, Lazarevich I, Delgadillo Velazquez J, Acosta Dominguez P, Zepeda Zepeda M . Comparison of the prevalence of sarcopenia using skeletal muscle mass index and calf circumference applying the European consensus definition in elderly Mexican women. Geriatr Gerontol Int 2015, e-pub ahead of print 4 November 2015 doi:10.1111/ggi.12652.
Rojer AGM, Kruizenga HM, Trappenburg MC, Reijnierse EM, Sipila S, Narici MV et al. The prevalence of malnutrition according to the new ESPEN definition in four diverse populations. Clin Nutr 2016; 35: 758–762.
Sanz-Paris A, Gomez-Candela C, Martín-Palmero A, García-Almeida JM, Burgos-Pelaez R, Matía-Martin P et al. Application of the new ESPEN definition of malnutrition in geriatric diabetic patients during hospitalization: a multicentric study. Clin Nutr 2016, e-pub ahead of print 8 March 2016 doi:10.1016/j.clnu.2016.02.018.
Acknowledgements
We are grateful to Emi Nishioka, RD, Natsumi Mori, RD and Riko Watanabe, RD for conducting the anthropometric measures. This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
HW received reimbursement for travel expenses from Nestlé Health Sciences outside the submitted work. SN and TY declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Nishioka, S., Wakabayashi, H. & Yoshida, T. Accuracy of non-paralytic anthropometric data for nutritional screening in older patients with stroke and hemiplegia. Eur J Clin Nutr 71, 173–179 (2017). https://doi.org/10.1038/ejcn.2016.191
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2016.191