Abstract
Background/Objectives:
Anthropometric measurement is a noninvasive and cost-efficient method for nutritional assessment. The study aims to present age- and gender-specific anthropometric reference data for Swedish elderly in relation to common medical conditions, and also formulate prediction equations for such anthropometric measurements.
Subjects/Methods:
A cross-sectional study among random heterogeneous sample of 3360 subjects, aged 60–99 years, from a population study ‘Good Aging in Scania. Means (±s.d.) and percentiles for height, weight, waist-, hip-, arm-, calf circumferences, triceps- (TST) and subscapular skinfold thickness (SST), body mass index (BMI), waist-hip ratio (WHR) and arm muscle circumference (AMC) were presented. The values were estimated based on the prevalence of myocardial infarction (MI), cardiac failure (CHF), stroke, cognitive impairment, dementia and dependence in daily living activities (ADL). Linear regression analysis was used to formulate the prediction equations.
Results:
Mean BMI was 27.5±5.8 kg/m2 (men) and 27.2±8.1 kg/m2 (women). WHR was higher among men (Men: 0.98±0.3, women: 0.87±0.2), except at age 85+ (women: 0.91±0.6). TST was 6.7±0.4 mm higher among women. Men with MI had BMI: 28.6±4.8 kg/m2 and SST: 21±9.2 mm, whereas subjects with dementia had lower weight (by 9.5±2.9 kg) compared with the non-demented. ADL-dependent women had BMI= 29.0±3.9 kg/m2, TST=19.2±1.3 mm.
Conclusion:
New normative data on gender- and age-specific anthropometrics on the general elderly population are presented. Cardiovascular diseases are associated with subcutaneous and central adiposity opposed to fat loss with dementia. ADL dependence indicates inadequate physical activity. The prediction models could be used as possible indicators monitoring physical activity and adiposity among the general elderly population hence potential health indicators in health promotion.
Similar content being viewed by others
Introduction
Monitoring and evaluation of health status of elderly individuals principally takes into account genetics, sociodemographic, dietary and lifestyle factors.1 Anthropometric testing is noninvasive and cost-efficient, effective in population-based studies.2 World Health Organization has assembled international anthropometric data for health assessment, nutrition and well-being emphasizing the significance of phenotypic impact of aging, senility and associated diseases. This urges the collection of normative anthropometric data specific for elderly.3 There have been several such international publications previously,1, 4, 5, 6, 7 such as, the SENECA study on nutritional health in 13 Western European countries.8 In Scandinavia, similar studies have been conducted where only height, weight and body mass index (BMI) were measured. Hence, there is a need for additional measurements that help in the better and holistic understanding of the anthropometric status. In this regard, it is worthy to mention the gerontological and geriatric population studies of Gothenburg (H-70) that additionally presented skinfold thicknesses (SST) and circumference measurements, although only among 70-year olds.9, 10 Longitudinal studies on anthropometric changes were done among 75-year olds in three Scandinavian localities (NORA)11 and middle-aged Swedish women.12 However, these studies have not considered the influence of underlying medical status and were targeted among specific gender- or age groups (70–75 years). In addition, NORA study included a relatively small sample size of 450 individuals.
There are certain ageing-related common medical conditions (CMC) and nutritional disorders that can be independent and interactive risk factors for mortality from systemic and metabolic conditions.13 To the best of our knowledge, there is no recent publication on gender- and age-specific anthropometric reference data for Swedish elderly population taking into account underlying diseases. It is therefore important to estimate this based on a large nationally representative sample. This study aims to describe the gender- and age-specific normative anthropometric data for a large national cohort of Swedish elderly, categorized based on the incidence of CMC namely myocardial infarction (MI), cardiac failure (CHF), stroke, cognitive impairment, dementia, instrument and personal dependence in instrumental (iADL) and personal activities of daily living (pADL).
Materials and methods
Study design
A cross-sectional study was conducted among subjects from a longitudinal, population study ‘Good Aging in Skåne’ (GÅS), part of Swedish National survey on Aging and Care (SNAC).14, 15 The study was approved by the Ethical Committee at Lund University (LU 744–00).
Study population
The study involved a heterogeneous sample of men and women, from five urban (third largest and midsize cities) and rural municipalities of the province of Scania, south Sweden, with similar sociodemographic characteristics as the rest of the country. GÅS included subjects from age cohorts 60, 66, 72, 78, 81, 84, 87, 90 and 93 years, with an oversampling of youngest and oldest cohorts. The aim was to recruit 700 subjects in ages 60 and 66 years, respectively, 250 subjects in ages 78, 81, 84 and 87 years, respectively, 200 subjects in the age 90 years and 100 subjects in age 93 years. Target populations were randomly invited using the National Population Registry.
The current study consists of 3360 subjects, aged 60–99 years, who accepted to participate in the follow-up examination of GÅS conducted in 2007–2010. Response rate was 80%. Of the 3360 subjects, 1832 subjects had participated in the GÅS baseline examination and 1528 were newly added. On the basis of a pre-established criteria a total of 3142 subjects (1688 from baseline and 1454 newcomers) formed the study population and 218 (144 from baseline and 74 newcomers) were excluded because they had missing data for one or more of the anthropometric variables under study. An attrition analysis was carried out to examine and compare the nonparticipants (n=1099) with the participants. The nonparticipants were recruited at baseline who dropped out for various reasons like death or migration (data not shown).
Data collection
All examinations were done at the Clinical Research Center, Malmö, Medical Faculty, Lund University and Skåne University Hospital. Home visits were offered if the participants so wanted. An informed consent was obtained from all subjects. Qualified physicians and nurses conducted the survey, medical examinations and physical functioning tests. Data on sociodemographics, physical, mental health and social factors were collected using a questionnaire from SNAC including previously validated variables.15
The descriptive variables were age, sex, place of birth, marital status, education, alcohol consumption, smoking habits and physical activity. The marital status denoted if single, married, divorced or living with a partner. Education was stratified into primary, secondary, higher secondary or university level. Smoking status indicated if regular, irregular or quit smoking. Alcohol frequency included responses as ‘have never drunk’, ‘a few times in the last year but not since last month’, ‘have had alcohol a few times in the last month’. The degree of physical activity was investigated in terms of intensity of training and categorized into barely physically active (‘nothing at all’ and ‘very light activity, that is, mostly sedentary, rarely a walk, light gardening or similar, sometimes light housework such as heating food, dusting’), mild (‘easier physical exertion ~2–4 h per week such as, walking, dancing and so on. Primary responsibility for light housework, like cooking, dusting, assisting in the weekly cleaning’), moderate (‘strenuous exercise 1–2 h per week, for example, jogging, swimming, fitness classes, heavier gardening and light exercises >4 h per week, responsible for all easy and heavy housework. Weekly chores including by vacuuming, floor/window cleaning’), heavy (‘strenuous exercise at least 3 h per week, such as tennis, swimming, jogging’) and very heavy (‘Hard exercise regularly/several times a week, such as running, skiing’).
Anthropometrics
Measurements were made by trained nurses, using validated and standardized protocols and calibrated instruments. Height, weight, waist-, hip-, arm- and calf circumferences and TST and SST were measured.14, 16, 17 BMI, waist-hip ratio (WHR) and arm muscle circumference (AMC) were calculated using respective mathematical formulae. BMI=weight (kg)/height (m2); WHR=waist circumference (cm)/hip circumference (cm); AMC=arm circumference (cm)−3.142 × TST (cm).18, 19
Height was measured using a measuring tape with the individual standing erect with shoulder blades, buttocks and heels against a wall and straight fixed gaze. Arms were along the sides, shoulders relaxed, legs straight, knees touching each other, feet flat and heels together. Readings were made in cm with one decimal value. Bedridden patients and those using a wheel chair were excluded from our study.
Weight (in kg) was measured with a precision balance scales in the morning with light clothes and no shoes, after voiding bowels and bladder in nonfasting conditions. The balance was manufactured by Tanita Corporation, Japan, and calibrated annually by the Technical Medical Division at Skåne University Hospital, Malmö, Sweden. The precision of the scale was ±50 g.
Waist circumference was measured at a level midway between the lowest rib and the iliac crest. Hip circumference was measured at the level of the great trochanters with the legs close together. Arm- and calf circumference were measured at the point of maximum convexity of biceps and calf muscles, respectively, with the limbs in completely relaxed position. All circumference measurements using a soft, nonelastic measuring tape, calibrated in millimeters, wound free from tension around the appropriate anatomic site.
SST (in mm) measured the double thickness of skin, underlying connective tissue and subcutaneous fat, but not the muscle. The Harpenden caliper (Baty International, Burgess Hill, West Sussex, UK) was applied 1 cm below and at right angles to the pinch. TST was measured at the level of the midpoint between the bony upper tip of shoulder (acromiale) and elbow joint (radiale) on the back of the left arm over the surface of the triceps muscle. SST was measured at the level of lower angle of scapula. TST and SST were measured in mm with one decimal and rounded to the nearest 0.2 mm.20
All measurements were made on the right side unless there was previous amputation, paralysis or contracture. All tests were made by two and the same nurses, who repeated the observations twice and calculated the average. No adjustments were made for possible interobserver variation.
Common medical conditions
Information from medical records, medical examination and functional tests were used to investigate the presence of CMC namely MI, CHF, stroke, dementia, cognitive impairment, iADL and pADL dependence.
The categorization of somatic diseases was based on the International Classification of Diseases (ICD-10) criteria. The category ‘MI’ also included angina and arrhythmia. Symptomatic CHF was defined from the NYHA (New York Heart Association) criteria and included subjects with NYHA class II-IV symptoms.21 The category ‘stroke’ included cerebral infarction, hemorrhage and transient ischemic attack. Dementia was defined based on the criteria in the Diagnostic and Statistical Manual of Mental Disorders IV according to the American Psychiatric Association Diagnostic and Statistical Manual.22 Cognitive impairment was defined as scoring below 24 points on the MMSE (Mini-Mental State Examination).23
Functional ability was assessed by self-reporting on Hulter–Åsberg’s ADL scale that has demonstrated high validity and reliability.24, 25 The variable was coded into independence in daily living activities, dependence in iADL and dependence in pADL. It is an 11-step scale (0–10) where score-0 corresponds to completely independent individuals and score-10 to those who are dependent on all 10 instrumental and personal activities. pADL includes questions relating to hygiene, dressing/undressing, toilet use, mobility and food intake and iADL includes questions on grocery shopping, cooking and cleaning. A reduced pADL means also a reduction in IADL; however, the opposite does not apply.26
Statistical analysis
Data were categorized according to sex and age groups of 60–64, 65–69, 70–74, 75–79, 80–84 and 85+ years.
Results are expressed as means, s.d. and 10th, 25th, 50th, 75th and 90th percentiles. The assumptions of analysis of variance were tested by inspecting P–P plots of the standardized regression residuals. This did not raise any serious concerns regarding normality and homoscedasticity. One-way analysis of variance analysis was used in two settings: to test the differences in the mean values of the all the anthropometric measures across the different age groups and between the groups with and without each CMC.
The association between the CMC and anthropometric measures was investigated using linear regression analysis. Age-adjusted, gender-specific regression equations to predict weight, BMI and waist-hip ratio were formulated. SPSSv.20 (Armonk, NY, USA) was used. P⩽0.05 was considered statistically significant.
Results
A total of 3142 subjects, mean age 71±10.4 years, included 44.4% men and 55.6% women. There were 62.4% who were married, 39.5% smokers, 33.2% who consumed alcohol at least until last month, 6.9% barely physically active, 26.4% had moderate activity and 51.5% had at least primary education. The attrition analysis showed the nonparticipants were generally older, with greater burden of those diseases under study and particularly those aged >80 years had lower weight, TST, SST, hip, arm- and calf circumferences than the study subjects.
Table 1 shows the anthropometric status of men and women stratified into six age groups. Mean BMI and WHR were higher among men than women, among all ages, except WHR among women aged 85+ years (0.91±0.59). TST was 6.7±0.4 mm higher among women with an age-related decline in both sexes (difference between 60–64 and 85+ years in men: 6.0±4.7 men; women: 7.6±1.2 mm). SST, arm- and calf circumferences and AMC significantly declined with age in both sexes.
Table 2 presents the number and percentage of men and women with CMC stratified among the age categories. MI prevalence was 21.2% among 75–79 years and 23.3% among 80–84 years men, whereas it was roughly 11.4% among 80+ years women. iADL prevalence was higher among men (8.8%), especially among 85+ year olds (23.9%). pADL was higher among women (33.7%) in all age groups. CHF prevalence increased with age and approximately doubled after age 70 years, among both men and women.
Table 3 presents the anthropometric measurements among men and women with and without the CMC. In comparison with those without or asymptomatic CMC (referred to as reference group), BMI, waist, hip- and arm circumferences and SST were higher, among men with MI. Similar findings added to higher weight, waist and calf circumferences were observed in both sexes with CHF.
Men with dementia had significantly lower weight (by 7.9±0.2 kg), SST (by 3±2.8 mm), TST (by 3.1±1.7 mm) and calf circumference (by 2.7±1.1 cm) compared with those without dementia. Likewise, women with dementia showed significant lower weight (by 11.3 kg±4.7 kg), BMI (by 3.6±1.9 kg/m2), hip circumference (by 7.4±3.8 cm) and calf circumference (by 3.6±0.6 cm). Decrease in height (men: 4±0.9 cm, women: 5.6±0.8 cm), weight (men: 4.3±0.2 kg, women: 3.7±6.3 kg), SST, arm- and calf circumferences were seen in both sexes with cognitive impairment. All the above-mentioned anthropometric differences were statistically significant (P⩽ 0.05).
Subjects with ADL dependence, particularly women, showed significantly higher values of BMI (by ~3.0±3.9 kg/m2), waist, hip, arm- and calf circumference and lower TST and SST (by 2±1.3 mm).
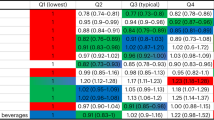
Table 4 presents the age- and gender-adjusted linear regression coefficient for every anthropometric variable among those with CMC compared with their respective reference groups.
Presence of dementia showed a significant negative relationship with weight, BMI, hip-, arm- and calf circumferences. Stroke patients on the other hand presented with a positive association with weight and waist circumference. MI cases presented significantly higher value with respect to weight, BMI, waist-, hip-, arm circumferences and SST compared with their healthier counterparts. Similar positive association at further higher rate was observed among CHF cases. No significant age-independent associations were seen in ADL dependence.
Table 5 presents the gender-specific regression model formulated for every anthropometric measurement with age, to enable the prediction of age-specific normative anthropometric values with 95% confidence intervals. The general equation is: predicted value=Intercept+(gender-specific coefficient) × age. Graphs depicting such gender-specific regression models for weight, BMI and WHR were drawn (Figure 1).
Age- and gender-specific regression equations to predict the weight, BMI and WHR among elderly men (i) and women (ii) aged ⩾60 years. The corresponding regression equations represented in the graphs include: (i) men weight: 110.04–0.37 x age, BMI: 31.36–0.06 x age, waist:hip ratio: 1.11–0.002 x age. (ii) Women weight: 92.19–0.30 x age, BMI: 29.73–0.04 x age, waist:hip ratio: 0.78+0.001 x age.
Discussion
Normative data on anthropometric measurements for Swedish elderly are presented together with gender-specific regression models aimed to predict these measurements. This can facilitate the interpretation of differences and patterns in phenotypic changes with ageing. We found significant anthropometric differences between elderly with or without CMC. Subjects with MI and CHF had values indicating subcutaneous and central adiposity, in contrast to low weight among subjects with dementia and cognitive impairment. The anthropometric profile of ADL dependent indicated physical inactivity.
Men are taller, heavier and have higher BMI than women (as expected) with a gradual age-related decline in height in both sexes that can be attributed to bone degenerative diseases.27 Loss of ~10 kg in weight with age, mostly at 80+ years, could be due to sarcopenia from disuse atrophy and senility.13, 28 Such gender- and age differences were similar to SENECA study (men: 75±10.4 kg, 71.1±12 kg; women: 64.5±12.4 kg, 62.8±1 kg, in Denmark, Norway, respectively);8 however, the mean values were higher in our study. Weight loss from 70 to 85+ years (Men: 8.8 ±1.2 kg; Women: 9.4±1.3 kg) was almost twice that according to H-70 study (men: 3.2 kg; women: 5.1 kg).7
BMI initially increases with age, but declines after 75–79 years. This inverted U-trend is also noted in a similar Italian study.28 It can be related to physical inactivity and sarcopenia, as well as the possibility of selective attrition of subjects with very high BMI-associated medical conditions, such as MI and stroke.13, 28 Mean BMI was similar to SENECA (Finland: 27.3 kg/m2), whereas that for 75 years was higher compared with the Swedish cohort of NORA75 study (25.3 kg/m2).8 Obesity is denoted by BMI ⩾30 kg/m2. Our data (75th percentiles) clearly indicated overweight and risk for obesity in both sexes. This has to be interpreted with caution taking into account the possibility of selection bias where morbidly obese and severely undernourished were excluded. There is also a possible effect of height loss with age translated into increasing BMI.27 Lack of distinction between fat and fat-free weight can lead to misinterpretation of high BMI (from muscle mass) as overweight or risk for obesity.29 Despite these factors, mean BMI shows an overall growing tendency in both men and women compared with the past two decades, according to SENECA and H-70 studies.7, 8
Increasing pattern in WHR among women 60–80 years could indicate age-related increase in adiposity. TST was also higher among women similar to SENECA’s Norwegian (women: 24.3 cm; men: 18.4 cm) and Danish population (women: 20.7 cm; men: 11.3 cm) and NHANES study’s American population (women: 22.5 cm; men: 15.3 cm).30, 31 Studies suggest the effects of late post-menopausal nonestrogenic condition on fat redistribution, and the sarcopenia associated with loss of type-2 glycolytic fibers.8, 28 Visceral adiposity is often coupled with progressive loss in the extremities.28, 32 This can be appreciated by lower arm circumference, AMC among women similar to SENECA Norwegian and Danish populations.8, 19
Association between anthropometrics and CMC
Anthropometric measurements in relation to MI, CHF, stroke, ADL dependence, cognitive impairment and dementia were assessed.
Subjects with MI had significantly higher weight, BMI, waist-, hip- and arm circumference and SST, indicating a higher prevalence of subcutaneous and central adiposity.33 Central obesity, a predisposing factor to MI and progressing to CHF, can cause patients to present with the above-mentioned anthropometric profile.34
Similarly, CHF patients had higher weight, waist circumference and skinfold measurement indicating a strong association and/or predisposition to the disease.33, 35 It has been reported that MI and CHF patients are associated with weight gain due to fluid retention and use of beta-blockers.35, 36 After MI, cardiac adaptation to excess body fat could significantly affect cardiac function directly or through increased the risk of diabetes, hypertension and release of inflammatory cytokines, leading to cardiac failure.34, 35
ADL-dependent patients, particularly women, had higher BMI, waist- and hip circumference and lower TST. This could indicate inadequate physical training leading to replacement of muscle mass, fat accumulation and weight gain.37
Patients with cognitive impairment had a lower weight and WHR and patients with dementia had in addition, lower skinfold, arm- and calf circumferences. This could be explained by two reasons—the inability of coherent control and disinterest stemming from impaired mental state, could affect healthy diet and exercises.38, 39 Dementia is also related to dysphagia that could interfere with dietary intake.40
Finally, a generalized equation (intercept+coefficient (B) x age) to estimate age- and gender-specific anthropometric measurements was formulated as an indicator of nutritional status and physical activity of elderly at a population level. Information on changes of anthropometrics changes, particularly decreasing muscle mass or increasing central adiposity in the general population could be useful in preventive strategies in public health.
The main strength of our study is the large population sample that is nationally representative owing to a random age- and gender-stratified selection, inclusion of both urban and rural areas of Scania thereby increasing generalization of data. Previous studies have shown that there were substantial anthropometric differences between rural and urban populations, where the former being heavier and having more muscle mass.41 However, a significant limitation might be a possible cohort effect. The anthropometric differences between age groups could be attributed to a generational difference. Although our results were consistent with other longitudinal findings, we aim to test the effect of generation and birth cohorts on physical activity and dietary intake that could influence anthropometrics in our forthcoming follow-up study. Examinations were done at the hospital or patient’s home to reduce selection bias that might however not be completely eliminated. The attrition analysis indicated that the nonparticipants who were relatively older and frail, had measurements indicating central adiposity and muscle loss. The underrepresentation of this group may have affected the estimated mean anthropometric measures.
The data collection was done by trained professionals using standardized protocols and calibrated instruments. Hematologic test and biochemical profile are considered to validate the anthropometric nutritional health assessment in future studies.
In conclusion, new normative data on gender- and age-specific anthropometrics on the elderly general population are presented. Cardiovascular diseases are associated with adiposity opposed to dementia with fat loss. ADL dependence indicates inadequate physical activity. The prediction models could be used as a tool monitoring physical activity and adiposity among the general elderly population hence potential health risk indicators in health promotion.
References
Sanchez-Garcia S, Garcia-Pena C, Duque-Lopez MX, Juarez-Cedillo T, Cortes-Nunez AR, Reyes-Beaman S . Anthropometric measures and nutritional status in a healthy elderly population. BMC Public Health 2007; 7: 2.
World Health Organization. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 1995; 854: 1–452.
de Onis M, Habicht JP . Anthropometric reference data for international use: recommendations from a World Health Organization Expert Committee. Am J Clin Nutr 1996; 64: 650–658.
Munoz AM, Falque-Madrid L, Zambrano RC, Maestre GE . Basic anthropometry and health status of elderly: findings of the Maracaibo Aging Study. J Aging Health 2010; 22: 242–261.
Kuczmarski MF, Kuczmarski RJ, Najjar M . Descriptive anthropometric reference data for older Americans. J Am Diet Assoc 2000; 100: 59–66.
Coqueiro Rda S, Barbosa AR, Borgatto AF . Anthropometric measurements in the elderly of Havana, Cuba: age and sex differences. Nutrition 2009; 25: 33–39.
Dey DK, Rothenberg E, Sundh V, Bosaeus I, Steen B . Height and body weight in the elderly. I. A 25-year longitudinal study of a population aged 70 to 95 years. Eur J Clin Nutr 1999; 53: 905–914.
de Groot CP, Perdigao AL, Deurenberg P . Longitudinal changes in anthropometric characteristics of elderly Europeans. SENECA Investigators. Eur J Clin Nutr 1996; 50 (Suppl 2), S9–S15.
Rinder L, Roupe S, Steen B, Svanborg A . Seventy-year-old people in Gothenburg. A population study in an industrialized Swedish city. Acta Med Scand 1975; 198: 397–407.
Steen B, Djurfeldt H . The gerontological and geriatric population studies in Gothenburg, Sweden. Z Gerontol 1993; 26: 163–169.
Gause-Nilsson I, Suominen H, Laukkanen P, Schroll M, Steen B . Body composition, smoking and physical activity in 75-year-old men and women in three Nordic localities with special reference to diagnosed diseases. J Nutr Health Aging 1999; 3: 172–176.
Noppa H, Andersson M, Bengtsson C, Bruce A, Isaksson B . Longitudinal studies of anthropometric data and body composition. The population study of women in Gotenberg, Sweden. Am J Clin Nutr 1980; 33: 155–162.
Dey DK, Rothenberg E, Sundh V, Bosaeus I, Steen B . Body mass index, weight change and mortality in the elderly. A 15 y longitudinal population study of 70 y olds. Eur J Clin Nutr 2001; 55: 482–492.
Lagergren M, Fratiglioni L, Hallberg IR, Berglund J, Elmstahl S, Hagberg B et al. A longitudinal study integrating population, care and social services data. The Swedish National study on Aging and Care (SNAC). Aging Clin Exp Res 2004; 16: 158–168.
Ekstrom H, Elmstahl S . Pain and fractures are independently related to lower walking speed and grip strength: results from the population study ‘Good Ageing in Skane’. Acta Orthop 2006; 77: 902–911.
Gibson R . Principles of Nutritional Assessment. 2nd edn. Oxford University Press: New York, NY, 1990.
Gibson R . Nutritional Assessment: A Laboratory Manual. Oxford University Press: New York, NY, 1993.
Weber J, Kelley J . Assessing nutrition. In: Nieginski E (ed). Health Assessment in Nursing. 3rd edn. Lippincott Williams & Wilkins: Philadelphia: Philadelphia, 2003; 165.
Noori N, Kopple JD, Kovesdy CP, Feroze U, Sim JJ, Murali SB et al. Mid-arm muscle circumference and quality of life and survival in maintenance hemodialysis patients. Clin J Am Soc Nephrol 2010; 5: 2258–2268.
Simko MD, Cowell C, Gilbride JA . Nutrition Assessment: A Comprehensive Guide for Planning Intervention. 2nd edn. Aspen Publications Inc: Gaithersburg, MD, USA, 1984.
American Heart Association. Classes of heart failure 2013, Available at http://www.heart.org/HEARTORG/Conditions/HeartFailure/AboutHeartFailure/Classes-of-Heart-Failure_UCM_306328_Article.jsp. Accessed on 14 January 2014.
American Psychiatric Association Diagnostic and Statistical Manual Diagnostic and Statistical Manual 1994.
Folstein MF, Folstein SE, McHugh PR . ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12: 189–198.
Asberg KH, Sonn U . The cumulative structure of personal and instrumental ADL. A study of elderly people in a health service district. Scand J Rehabil Med 1989; 21: 171–177.
Sonn U, Asberg KH . Assessment of activities of daily living in the elderly. A study of a population of 76-year-olds in Gothenburg, Sweden. Scand J Rehabil Med 1991; 23: 193–202.
Elmståhl S, Ekström H . Prediktorer för livstillfredsställelse, funktionsförmåga och aktiviteter i det dagliga livet - Data från den longitudinella befolkningsstudien ’Gott Åldrande i Skåne’. En sexårsuppföljning av 60 till 93 år gamla Malmöbor 2012, pp 1–23.
Gavriilidou NN, Pihlsgard M, Elmstahl S . High degree of BMI misclassification of malnutrition among Swedish elderly population: Age-adjusted height estimation using knee height and demispan. Eur J Clin Nutr 2014, e-pub ahead of print 10 September 2014 doi:10.1038/ejcn.2014.183.
Perissinotto E, Pisent C, Sergi G, Grigoletto F, ILSA Working Group (Italian Longitudinal Study on Ageing). Anthropometric measurements in the elderly: age and gender differences. Br J Nutr 2002; 87: 177–186.
Price GM, Uauy R, Breeze E, Bulpitt CJ, Fletcher AE . Weight, shape, and mortality risk in older persons: elevated waist-hip ratio, not high body mass index, is associated with a greater risk of death. Am J Clin Nutr 2006; 84: 449–460.
de Groot CP, Perdigao AL, Deurenberg P . Longitudinal changes in anthropometric characteristics of elderly Europeans. SENECA Investigators. Eur J Clin Nutr 1996; 50 (Suppl 2), S9–S15.
Kuczmarski MF, Kuczmarski RJ, Najjar M . Descriptive anthropometric reference data for older Americans. J Am Diet Assoc 2000; 100: 59–66.
Wang Q, Hassager C, Ravn P, Wang S, Christiansen C . Total and regional body-composition changes in early postmenopausal women: age-related or menopause-related? Am J Clin Nutr 1994; 60: 843–848.
Kumar A, Sivakanesan R . Anthropometric profile in normolipidaemic myocardial infarction patients In South Asia: a case-control study. J Clin Diagn Res 2008; 2: 997–1000.
Azarfarin R, Samadikhah J, Shahvalizadeh R, Golzari SE . Evaluation of anthropometric indices of patients with left ventricle dysfunction fallowing first acute anterior myocardial infarction. J Cardiovasc Thorac Res 2012; 4: 11–15.
Borne Y, Hedblad B, Essen B, Engstrom G . Anthropometric measures in relation to risk of heart failure hospitalization: a Swedish population-based cohort study. Eur J Public Health 2014; 24: 215–220.
Rossner S, Taylor CL, Byington RP, Furberg CD . Long term propranolol treatment and changes in body weight after myocardial infarction. BMJ 1990; 300: 902–903.
Corona LP, Nunes DP, Alexandre Tda S, Santos JL, Duarte YA, Lebrao ML . Weight gain among elderly women as risk factor for disability: Health, Well-being and Aging Study (SABE Study). J Aging Health 2013; 25: 119–135.
Miyamoto K, Higashino S, Mochizuki K, Goda T, Koyama H . Evaluation of weight loss in the community-dwelling elderly with dementia as assessed by eating behavior and mental status. Asia Pac J Clin Nutr 2011; 20: 9–13.
Camina Martin MA, de Mateo Silleras B, Redondo del Rio MP . Body composition analysis in older adults with dementia. Anthropometry and bioelectrical impedance analysis: a critical review. Eur J Clin Nutr 2014; 68: 1228–1233.
Petersson S, Mathillas J, Wallin K, Olofsson B, Allard P, Gustafson Y . Risk factors for depressive disorders in very old age: a population-based cohort study with a 5-year follow-up. Soc Psychiatry Psychiatr Epidemiol 2014; 49: 831–839.
Elmstahl S, Gardsell P, Ringsberg K, Sernbo I . Body composition and its relation to bone mass and fractures in an urban and a rural population. Aging (Milano) 1993; 5: 47–54.
Acknowledgements
The project Good Aging in Skåne (GÅS), a part of the Swedish National study on Aging and Care (SNAC) was supported by the Swedish Ministry of Social Affairs, the county Region Skåne, Medical faculty of Lund University and Vårdal Institute.
Author Contributions
NNG was responsible for study design, analysis and interpretation of data and preparation of manuscript. MP was responsible for study design and preparation of manuscript. SE was responsible for study concept and design, acquisition and maintenance of study cohort, analysis and interpretation of data and preparation of manuscript, study design, analysis and interpretation of data, preparation of manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Gavriilidou, N., Pihlsgård, M. & Elmståhl, S. Anthropometric reference data for elderly Swedes and its disease-related pattern. Eur J Clin Nutr 69, 1066–1075 (2015). https://doi.org/10.1038/ejcn.2015.73
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2015.73
This article is cited by
-
Calf circumference as a surrogate indicator for detecting low muscle mass in hospitalized geriatric patients
Aging Clinical and Experimental Research (2024)
-
A comparison of the different anthropometric indices for assessing malnutrition among older people in Turkey: a large population-based screening
Journal of Health, Population and Nutrition (2021)
-
Sarcopenia in hospitalized geriatric patients: insights into prevalence and associated parameters using new EWGSOP2 guidelines
European Journal of Clinical Nutrition (2021)
-
Validation of an automated home blood pressure measurement device in oldest-old populations
Hypertension Research (2020)
-
Effect of monosodium l-glutamate (umami substance) on cognitive function in people with dementia
European Journal of Clinical Nutrition (2019)