Abstract
Background/Objectives:
There are several biomarkers for measuring iron deficiency (ID) in pregnancy, but the prevalence of ID and its association with inflammation and adverse pregnancy outcomes is inconclusive. The aim of this work was to describe the prevalence and determinants of first trimester ID and associations with pregnancy and birth outcomes.
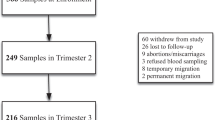
Subjects/Methods:
A record-linkage cohort study of archived serum samples of women attending first trimester screening and birth and hospital data to ascertain maternal characteristics and pregnancy outcomes. Sera were analysed for iron stores (ferritin; μg/l), lack of iron in the tissues (soluble transferrin receptor (sTfR); nmol/l) and inflammatory (C-reactive protein (CRP); mg/dl) biomarkers. Total body iron (TBI) was calculated from serum ferritin (SF) and sTfR concentrations. Multivariate logistic regression analysed risk factors and pregnancy outcomes associated with ID using the definitions: SF<12 μg/l, TfR⩾21.0 nmol/l, and TBI<0 mg/kg.
Results:
Of the 4420 women, the prevalence of ID based on ferritin, sTfR and TBI was 19.6, 15.3 and 15.7%, respectively. Risk factors of ID varied depending on which iron parameter was used and included maternal age <25 years, multiparity, socioeconomic disadvantage, high maternal body weight and inflammation. ID, defined by SF and TBI but not TfR, was associated with reduced risk of gestational diabetes mellitus (GDM). ID defined using TBI only was associated with increased risk of large-for-gestation-age (LGA) infants.
Conclusions:
Nearly one in five Australian women begin pregnancy with ID. Further investigation of excess maternal weight and inflammation in the relationships between ID and GDM and LGA infants is needed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Scholl T . Iron status during pregnancy: setting the stage for mother and infant. Am J Clin Nutr 2005; 81: S1218–S1222.
WHO. Serum ferritin concentrations for the assessment of iron status and iron deficiency in populations. Vitamin and Mineral Nutrition Information System Geneva, World Health Organization, (WHO/NMH/NHD/MNM/112), 2011: http://www.who.int/vmnis/indicators/serum_ferritin.pdf (accessed 01 August 2014).
Milman N, Agger AO, Nielsen OJ . Iron status markers and serum erythropoietin in 120 mothers and newborn infants. Acta Obstet Gynecol Scand 1994; 73: 200–204.
Wish J . Assessing iron status: beyond serum ferritin and transferrin saturation. Clin J Am Soc Nephrol 2006; 1: S4–S8.
Skikne B, Flowers CH, Cook JD . Serum transferrin receptor: a quantitative measure of tissue iron deficiency. Blood 1990; 75: 1870–1876.
Righetti A, Wegmüller R, Glinz D, Ouattara M, Adiossan LG, N'Goran EK et al. Effects of inflammation and Plasmodium falciparum infection on soluble transferrin receptor and plasma ferritin concentration in different age groups: a prospective longitudinal study in Côte d'Ivoire. Am J Clin Nutr 2013; 97: 1364–1374.
Leonard A, Patterson AJ, Chalmers K, Collins CE . Is soluble transferrin receptor a useful marker in early stage iron deficiency? e-SPEN Journal 2013; 8: e210–e212.
Cook J, Flowers CH, Skikne BS . The quantitative assessment of body iron. Blood 2003; 101: 3359–3364.
Pavord S, Myers B, Robinson S, Allard S, Strong J, Oppenheimer C . British Committee for Standards in Haematology. UK guidelines on the management of iron deficiency in pregnancy. Br J Haematol 2012; 156: 588–600.
Haider B, Olofin I, Wang M, Spiegelman D, Ezzati M, Fawzi WW . Anaemia, prenatal iron use, and risk of adverse pregnancy outcomes: systematic review and meta-analysis. BMJ 2013; 346: 3443.
Cogswell M, Parvanta I, Ickes L, Yip R, Brittenham GM . Iron supplementation during pregnancy, anemia, and birth weight: a randomized controlled trial. Am J Clin Nutr 2003; 78: 773–781.
US Preventive Services Task Force. Routine iron supplementation during pregnancy. JAMA 1993; 270: 2848–2854.
Rasmussen K . Is there a causal relationship between iron deficiency or iron-deficiency anemia and weight at birth, length of gestation and perinatal mortality? J Nutr 2001; 131: 590 S–601 S.
Human sTfR Immunoassay Quantikine IVD Soluble Transferrin Receptor ELISA R&D Systems Inc. Catalog Number DTFR1 2013; R&D Systems China Co. Ltd.
Milman N . Iron in pregnancy: how do we secure an appropriate iron status in the mother and child? Ann Nutr Metab 2011; 59: 50–54.
Wen S, Smith G, Yang Q, Walker M . Epidemiology of preterm birth and neonatal outcome. Semin Fetal Neonatal Med 2004; 9: 429–435.
Lawrence G, Dinh I, Taylor L . The centre for health record linkage: a new resource for health services research and evaluation. HIM J 2008; 37: 60–62.
Roberts C, Cameron CA, Bell JC, Algert C, Morris J . Measuring maternal morbidity in routinely collected health data: development and validation of a maternal morbidity outcome indicator. Med Care 2008; 46: 786–794.
Taylor L, Travis S, Pym M, Olive E, Henderson-Smart DJ . How useful are hospital morbidity data for monitoring conditions occurring in the perinatal period? Aust N Z J Obstet Gynaecol 2005; 45: 36–41.
Australian Bureau of Statistics Socio-Economic Indexes for Areas (SEIFA), Technical Paper, 2008 2039:0.55.00.
Bell J, Ford JB, Cameron CA, Roberts CL . The accuracy of population health data for monitoring trends and outcomes among women with diabetes in pregnancy. Diabetes Res Clin Pract 2008; 81: 105–109.
Lain S, Hadfield RM, Raynes-Greenow CH, Ford JB, Mealing NM, Algert CS . Quality of data in perinatal population health databases: a systematic review. Med Care 2002; 50: e7–20.
Brown M, Lindheimer MD, de Swiet M, Van Assche A, Moutquin JM . The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy 2001; 20: IX–XIV.
Roberts C, Lancaster PA . Australian national birthweight percentiles by gestational age. Med J Aust 1999; 170: 114–118.
Hercberg S, Preziosi P, Galan P . Iron deficiency in Europe. Public Health Nutr 4 2001; 4: 537–545.
Lee J, Lee JH, Ahn S, Kim JW, Chang H, Kim YJ et al. Prevalence and risk factors for iron deficiency anemia in the korean population: results of the fifth Korea National Health and Nutrition Examination Survey. J Korean Med Sci 2014; 29: 224–229.
Mei Z, Cogswell ME, Looker AC, Pfeiffer CM, Cusick SE, Lacher DA et al. Assessment of iron status in US pregnant women from the National Health and Nutrition Examination Survey (NHANES), 1999–2006. Am J Clin Nutr 2011; 93: 1312–1320.
Engle-Stone R, Nankap M, Ndjebayi AO, Erhardt JG, Brown KH . Plasma ferritin and soluble transferrin receptor concentrations and body iron stores identify similar risk factors for iron deficiency but result in different estimates of the national prevalence of iron deficiency and iron-deficiency anemia among women and children in Cameroon. J Nutr 2013; 143: 369–377.
Knowles J, Thurnham DI, Phengdy B, Houamboun K, Philavong K, Keomoungkhone I et al. Impact of inflammation on the biomarkers of iron status in a cross-sectional survey of Lao women and children. Br J Nutr 2013; 110: 2285–2297.
Vandevijvere S, Amsalkhir S, Van Oyen H, Egli I, Moreno-Reyes R . Iron status and its determinants in a nationally representative sample of pregnant women. J Acad Nutr Diet 2013; 113: 659–666.
Andrews N . Anemia of inflammation: the cytokine-hepcidin link. J Clin Invest 2004; 113: 1251–1253.
Cepeda-Lopez A, Aeberli I, Zimmermann MB . Does obesity increase risk for iron deficiency? A review of the literature and the potential mechanisms. Int J Vitam Nutr Res 2010; 80: 263–270.
Knudsen V, Hansen HS, Ovesen L, Mikkelsen TB, Olsen SF . Iron supplement use among Danish pregnant women. Public Health Nutr 2007; 10: 1104–1110.
Allen L . Anemia and iron deficiency: effects on pregnancy outcome. Am J Clin Nutr 2000; 71: 280 s–284.
Siega-Riz A, Hartzema AG, Turnbull C, Thorp J, McDonald T, Cogswell ME . The effects of prophylactic iron given in prenatal supplements on iron status and birth outcomes: a randomized controlled trial. Am J Obstet Gynecol 2006; 194: 512–519.
Lao T, Ho LF . Impact of iron deficiency anemia on prevalence of gestational diabetes mellitus. Diabetes Care 2004; 27: 650–656.
Milman N, Bergholt T, Eriksen L, Byg KE, Graudal N, Pedersen P et al. Iron prophylaxis during pregnancy - How much iron is needed? A randomized dose-response study of 20–80 mg ferrous iron daily in pregnant women. Acta Obstet Gynecol Scand 2005; 84: 238–247.
Rioux F, LeBlanc CP . Iron supplementation during pregnancy: what are the risks and benefits of current practices? Appl Physiol Nutr Metab 2007; 32: 282–288.
Lao T, Tam KF, Chan LY . Third trimester iron status and pregnancy outcome in non-anaemic women; pregnancy unfavourably affected by maternal iron excess. Hum Reprod 2000; 15: 1843–1848.
Lao TT, C LY, Tam KF, Ho LF . Maternal hemoglobin and risk of gestational diabetes mellitus in Chinese women. Obstet Gynecol 2002; 99: 807–812.
Rao G, Morghom LO . Erythrocyte and hemoglobin levels in diabetic women. Eur J Appl Physiol 1984; 52: 272–275.
Harlan L, Harlan WR, Landis JR, Goldstein NG . Factors associated with glucose tolerance in adults in the United States. Am J Epidemiol 1987; 126: 674–684.
Lao T, Pun TC . Anaemia in pregnancy: is the current definition meaningful? Eur J Obstet Gynecol Reprod Biol 1996; 68: 53–58.
Pfeiffer C, Cook JD, Mei Z, Cogswell ME, Looker AC, Lacher DA . Evaluation of an automated soluble transferrin receptor (sTfR) assay on the Roche Hitachi analyzer and its comparison to two ELISA assays. Clin Chim Acta 2007; 382: 112–116.
Flowers C, Skikne BS, Covell AM, Cook JD . The clinical measurement of serum transferrin receptor. J Lab Clin Med 1989; 114: 368–377.
Acknowledgements
We thank the New South Wales PaLMS Pathology service and Ministry of Health for provision of population data and the NSW Centre for Health Record Linkage for record linkage. This work was funded by a National Health and Medical Research Council (NHMRC) Project Grant (no. 632653). Funding for Amina Khambalia is by an Australian NHMRC Centers for Research Excellence (APP1001066), to Natasha Nassar by an NHMRC Career Development Fellowship (no. APP1067066) and to Christine Roberts by an NHMRC Senior Research Fellowship (no. APP1021025). Clare Collins is supported by a Faculty of Health and Medicine Strategic Research Fellowship at the University of Newcastle.
Author contributions
AZK, NN, CLR, JM and VT conceived and designed the study; NN, CLR, JM and VT acquired data; AZK was responsible for the integrity of data and statistical analysis; AZK drafted the manuscript; and all authors approved the manuscript and critically reviewed the manuscript for important intellectual content.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Khambalia, A., Collins, C., Roberts, C. et al. Iron deficiency in early pregnancy using serum ferritin and soluble transferrin receptor concentrations are associated with pregnancy and birth outcomes. Eur J Clin Nutr 70, 358–363 (2016). https://doi.org/10.1038/ejcn.2015.157
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2015.157
This article is cited by
-
Maternal factors associated with iron deficiency without anaemia in early pregnancy: ECLIPSES study
Annals of Hematology (2023)
-
Beyond hemoglobin: uncovering iron deficiency and iron deficiency anemia using serum ferritin concentration among pregnant women in eastern Ethiopia: a community-based study
BMC Nutrition (2022)
-
Iron deficiency anaemia associated with increased placenta praevia and placental abruption: a retrospective case-control study
European Journal of Clinical Nutrition (2022)
-
Maternal first trimester iron status and its association with obstetric and perinatal outcomes
Archives of Gynecology and Obstetrics (2022)
-
Iron Deficiency Anaemia and Atonic Postpartum Haemorrhage Following Labour
Reproductive Sciences (2022)