Abstract
Background/Objectives:
Studies suggest that the Mediterranean-style diet (MSD) may improve glucose metabolism in patients with type 2 diabetes (T2D), but the results are inconsistent. We conducted a meta-analysis of randomized controlled trials (RCTs) to explore the effects of MSD on glycemic control, weight loss and cardiovascular risk factors in T2D patients.
Subjects/Methods:
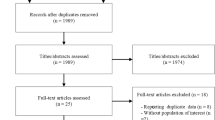
We performed searches of EMBASE, Cochrane Library and PubMed databases up to February 2014. We included RCTs that compared the MSD with control diets in patients with T2D. Effect size was estimated as mean difference with 95% confidence interval (CI) by using random effect models.
Results:
The meta-analysis included nine studies with 1178 patients. Compared with control diets, MSD led to greater reductions in hemoglobin A1c (mean difference, −0.30; 95% CI, −0.46 to −0.14), fasting plasma glucose (−0.72 mmol/l; CI, −1.24 to −0.21), fasting insulin (−0.55 μU/ml; CI, −0.81 to −0.29), body mass index (−0.29 kg/m2; CI, −0.46 to −0.12) and body weight (−0.29 kg; CI, −0.55 to −0.04). Likewise, concentrations of total cholesterol and triglyceride were decreased (−0.14 mmol/l; CI, −0.19 to −0.09 and −0.29 mmol/l; CI, −0.47 to −0.10, respectively), and high-density lipoprotein was increased (0.06 mmol/l; CI, 0.02 to 0.10). In addition, MSD was associated with a decline of 1.45 mm Hg (CI, −1.97 to −0.94) for systolic blood pressure and 1.41 mm Hg (CI, −1.84 to −0.97) for diastolic blood pressure.
Conclusions:
The present meta-analysis provides evidence that MSD improves outcomes of glycemic control, body weight and cardiovascular risk factors in T2D patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Whiting DR, Guariguata L, Weil C, Shaw J . IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract 2011; 94: 311–321.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403.
Li G, Zhang P, Wang J, Gregg EW, Yang W, Gong Q et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet 2008; 371: 1783–1789.
Lindstrom J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson JG, Hemio K et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet 2006; 368: 1673–1679.
Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001; 344: 1343–1350.
Yamaoka K, Tango T . Efficacy of lifestyle education to prevent type 2 diabetes: a meta-analysis of randomized controlled trials. Diabetes Care 2005; 28: 2780–2786.
Sofi F, Macchi C, Abbate R, Gensini GF, Casini A . Mediterranean diet and health status: an updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr 2013; 1–14.
Serra-Majem L, Roman B, Estruch R . Scientific evidence of interventions using the Mediterranean diet: a systematic review. Nutr Rev 2006; 64: S27–S47.
Keys A, Menotti A, Karvonen MJ, Aravanis C, Blackburn H, Buzina R et al. The diet and 15-year death rate in the seven countries study. Am J Epidemiol 1986; 124: 903–915.
Sofi F . The Mediterranean diet revisited: evidence of its effectiveness grows. Curr Opin Cardiol 2009; 24: 442–446.
Dominguez LJ, Bes-Rastrollo M, de la Fuente-Arrillaga C, Toledo E, Beunza JJ, Barbagallo M et al. Similar prediction of total mortality, diabetes incidence and cardiovascular events using relative- and absolute-component Mediterranean diet score: the SUN cohort. Nutr Metab Cardiovasc Dis 2013; 23: 451–458.
Salas-Salvado J, Bullo M, Estruch R, Ros E, Covas MI, Ibarrola-Jurado N et al. Prevention of diabetes with Mediterranean diets: a subgroup analysis of a randomized trial. Ann Intern Med 2014; 160: 1–10.
Koloverou E, Esposito K, Giugliano D, Panagiotakos D . The effect of Mediterranean diet on the development of type 2 diabetes mellitus: A meta-analysis of 10 prospective studies and 136,846 participants. Metabolism 2014; 63: 903–911.
Jensen A, Sherman S . In patients at high CV risk, a Mediterranean diet plus olive oil reduced diabetes more than advising a low-fat diet. Ann Intern Med 2014; 160: JC2.
Esposito K, Chiodini P, Maiorino MI, Bellastella G, Panagiotakos D, Giugliano D . Which diet for prevention of type 2 diabetes? A meta-analysis of prospective studies. Endocrine 2014; 47: 107–116.
Rossi M, Turati F, Lagiou P, Trichopoulos D, Augustin LS, La Vecchia C et al. Mediterranean diet and glycaemic load in relation to incidence of type 2 diabetes: results from the Greek cohort of the population-based European Prospective Investigation into Cancer and Nutrition (EPIC). Diabetologia 2013; 56: 2405–2413.
Salas-Salvado J, Bullo M, Babio N, Martinez-Gonzalez MA, Ibarrola-Jurado N, Basora J et al. Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care 2011; 34: 14–19.
Martinez-Gonzalez MA, de la Fuente-Arrillaga C, Nunez-Cordoba JM, Basterra-Gortari FJ, Beunza JJ, Vazquez Z et al. Adherence to Mediterranean diet and risk of developing diabetes: prospective cohort study. BMJ 2008; 336: 1348–1351.
Toobert DJ, Glasgow RE, Strycker LA, Barrera M Jr., Radcliffe JL, Wander RC et al. Biologic and quality-of-life outcomes from the Mediterranean Lifestyle Program: a randomized clinical trial. Diabetes Care 2003; 26: 2288–2293.
Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, Greenberg I et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med 2008; 359: 229–241.
Esposito K, Maiorino MI, Ciotola M, Di Palo C, Scognamiglio P, Gicchino M et al. Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: a randomized trial. Ann Intern Med 2009; 151: 306–314.
Itsiopoulos C, Brazionis L, Kaimakamis M, Cameron M, Best JD, O'Dea K et al. Can the Mediterranean diet lower HbA1c in type 2 diabetes? Results from a randomized cross-over study. Nutr Metab Cardiovasc Dis 2011; 21: 740–747.
Elhayany A, Lustman A, Abel R, Attal-Singer J, Vinker S . A low carbohydrate Mediterranean diet improves cardiovascular risk factors and diabetes control among overweight patients with type 2 diabetes mellitus: a 1-year prospective randomized intervention study. Diabetes Obes Metab 2010; 12: 204–209.
Toobert DJ, Strycker LA, King DK, Barrera M Jr., Osuna D, Glasgow RE . Long-term outcomes from a multiple-risk-factor diabetes trial for Latinas: inverted exclamation markViva Bien!. Transl Behav Med 2011; 1: 416–426.
Rodriguez-Villar C, Perez-Heras A, Mercade I, Casals E, Ros E . Comparison of a high-carbohydrate and a high-monounsaturated fat, olive oil-rich diet on the susceptibility of LDL to oxidative modification in subjects with Type 2 diabetes mellitus. Diabet Med 2004; 21: 142–149.
Karantonis HC, Fragopoulou E, Antonopoulou S, Rementzis J, Phenekos C, Demopoulos CA . Effect of fast-food Mediterranean-type diet on type 2 diabetics and healthy human subjects' platelet aggregation. Diabetes Res Clin Pract 2006; 72: 33–41.
Brehm BJ, Lattin BL, Summer SS, Boback JA, Gilchrist GM, Jandacek RJ et al. One-year comparison of a high-monounsaturated fat diet with a high-carbohydrate diet in type 2 diabetes. Diabetes Care 2009; 32: 215–220.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Br Med J 2009; 339: b2700.
Higgins JPT, Green S . Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions. Wiley-Blackwell: Chichester, UK; Hoboken, NJ, USA, 2008.
Wiebe N, Vandermeer B, Platt RW, Klassen TP, Moher D, Barrowman NJ . A systematic review identifies a lack of standardization in methods for handling missing variance data. J Clin Epidemiol 2006; 59: 342–353.
Higgins JP, Thompson SG, Deeks JJ, Altman DG . Br Med J 2003; 327: 557–560.
Higgins JP . Commentary: heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol 2008; 37: 1158–1160.
Begg CB, Mazumdar M . Operating characteristics of a rank correlation test for publication bias. Biometrics 1994; 50: 1088–1101.
Egger M, Davey Smith G, Schneider M, Minder C . Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315: 629–634.
Clifton P, Fletcher E, Gailbraith C, Coles L . Diet choice in Type 2 diabetes. Obes Res Clin Pract 2012; 6: 26 (abstract).
Lasa A, Miranda J, Bullo M, Casas R, Salas-Salvado J, Larretxi I et al. Comparative effect of two Mediterranean diets versus a low-fat diet on glycaemic control in individuals with type 2 diabetes. Eur J Clin Nutr 2014; 68: 767–772.
Ajala O, English P, Pinkney J . Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr 2013; 97: 505–516.
Carter P, Achana F, Troughton J, Gray LJ, Khunti K, Davies MJ . A Mediterranean diet improves HbA1c but not fasting blood glucose compared to alternative dietary strategies: a network meta-analysis. J Hum Nutr Diet 2014; 27: 280–297.
Esposito K, Kastorini CM, Panagiotakos DB, Giugliano D . Mediterranean diet and weight loss: meta-analysis of randomized controlled trials. Metab Syndr Relat Disord 2011; 9: 1–12.
Buckland G, Bach A, Serra-Majem L . Obesity and the Mediterranean diet: a systematic review of observational and intervention studies. Obes Rev 2008; 9: 582–593.
Ros E, Martinez-Gonzalez MA, Estruch R, Salas-Salvado J, Fito M, Martinez JA et al. Mediterranean diet and cardiovascular health: teachings of the PREDIMED study. Adv Nutr 2014; 5: 330S–336S.
Bedard A, Riverin M, Dodin S, Corneau L, Lemieux S . Sex differences in the impact of the Mediterranean diet on cardiovascular risk profile. Br J Nutr 2012; 108: 1428–1434.
Georgoulis M, Kontogianni MD, Yiannakouris N . Mediterranean diet and diabetes: prevention and treatment. Nutrients 2014; 6: 1406–1423.
Esposito K, Giugliano D . Mediterranean diet and type 2 diabetes. Diabetes Metab Res Rev 2014; 30: 34–40.
Ortega R . Importance of functional foods in the Mediterranean diet. Public Health Nutr 2006; 9: 1136–1140.
Mantzoros CS, Williams CJ, Manson JE, Meigs JB, Hu FB . Adherence to the Mediterranean dietary pattern is positively associated with plasma adiponectin concentrations in diabetic women. Am J Clin Nutr 2006; 84: 328–335.
Estruch R, Martínez-González MA, Corella D, Basora-Gallisá J, Ruiz-Gutiérrez V, Covas MI et al. Effects of dietary fibre intake on risk factors for cardiovascular disease in subjects at high risk. J Epidemiol Community Health 2009; 63: 582–588.
Micha R, Wallace SK, Mozaffarian D . Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation 2010; 121: 2271–2283.
Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Covas MI et al. Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med 2006; 145: 1–11.
Acknowledgements
This study was funded by the research grants from National Nature Science Foundation of China (30772207 to X Yu).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on European Journal of Clinical Nutrition website
Supplementary information
Rights and permissions
About this article
Cite this article
Huo, R., Du, T., Xu, Y. et al. Effects of Mediterranean-style diet on glycemic control, weight loss and cardiovascular risk factors among type 2 diabetes individuals: a meta-analysis. Eur J Clin Nutr 69, 1200–1208 (2015). https://doi.org/10.1038/ejcn.2014.243
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2014.243
This article is cited by
-
Global, regional, and national time trends in cancer mortality attributable to high fasting plasma glucose: an age-period cohort analysis
BMC Public Health (2023)
-
Mediterranean diet adherence and glycemic control in children and adolescents with type 1 diabetes
European Journal of Pediatrics (2023)
-
Diets for weight management in adults with type 2 diabetes: an umbrella review of published meta-analyses and systematic review of trials of diets for diabetes remission
Diabetologia (2022)
-
Adherence to the Dutch healthy diet index and change in glycemic control and cardiometabolic markers in people with type 2 diabetes
European Journal of Nutrition (2022)
-
Mediterranean Diet and Obesity-related Disorders: What is the Evidence?
Current Obesity Reports (2022)