Abstract
Background/Objectives:
There is increasing evidence showing that handgrip strength (HGS) is an indicator of nutrition status and a promising undernutrition screening tool. However, HGS cutoff values for inpatient undernutrition screening remain to be studied. The present study aims to define gender- and age-specific HGS cutoff values for undernutrition screening of hospitalized patients at admission.
Subjects/Methods:
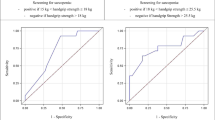
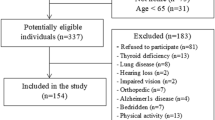
A cross-sectional study was conducted in a university hospital. Gender- and age-specific receiver operating characteristic curves were constructed to evaluate the performance of HGS for correctly screening undernourished patients on the basis of their classification by Patient-Generated Subjective Global Assessment. Sensitivity, specificity, areas under the curves (AUCs) and positive likelihood ratios (LRs) were calculated.
Results:
The study sample was composed of 712 participants between the ages of 18 and 91 years old, median (interquartile range) of 58 (22) years. For women, HGS cutoff values, sensitivities and specificities were as follows: 18–44 years, 20.2 kgf, 0.741 and 0.556; 45–64 years, 19.2 kgf, 0.795 and 0.522. For men, these values were as follows: 18–44 years, 41.7 kgf, 0.923 and 0.520; 45–64 years, 37.9 kgf, 0.817 and 0.402; ⩾65 years, 30.2 kgf, 0.736 and 0.567. The AUCs varied between 0.642 and 0.778 and LRs from 1.37 to 1.92.
Conclusions:
This study provides HGS cutoff values for men aged 18–91 years and for women aged 18–64 years.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Rasmussen HH, Holst M, Kondrup J . Measuring nutritional risk in hospitals. Clin Epidemiol 2010; 2: 209–216.
Barker LA, Gout BS, Crowe TC . Hospital malnutrition: prevalence, identification and impact on patients and the healthcare system. Int J Environ Res Public Health 2011; 8: 514–527.
Tappenden KA, Quatrara B, Parkhurst ML, Malone AM, Fanjiang G, Ziegler TR . Critical role of nutrition in improving quality of care: an interdisciplinary call to action to address adult hospital malnutrition. J Acad Nutr Diet 2013; 113: 1219–1237.
Norman K, Pichard C, Lochs H, Pirlich M . Prognostic impact of disease-related malnutrition. Clin Nutr 2008; 27: 5–15.
Sorensen J, Kondrup J, Prokopowicz J, Schiesser M, Krahenbuhl L, Meier R et al. EuroOOPS: an international, multicentre study to implement nutritional risk screening and evaluate clinical outcome. Clin Nutr 2008; 27: 340–349.
Kondrup J, Allison SP, Elia M, Vellas B, Plauth M . ESPEN guidelines for nutrition screening 2002. Clin Nutr 2003; 22: 415–421.
Lim SL, Ong KC, Chan YH, Loke WC, Ferguson M, Daniels L . Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin Nutr 2012; 31: 345–350.
van Bokhorst-de van der Schueren MA, Guaitoli PR, Jansma EP, de Vet HC . Nutrition screening tools: Does one size fit all? A systematic review of screening tools for the hospital setting. Clin Nutr 2014; 33: 39–58.
Leandro-Merhi VA, de Aquino JL, Sales Chagas JF . Nutrition status and risk factors associated with length of hospital stay for surgical patients. JPEN J Parenter Enteral Nutr 2011; 35: 241–248.
Hiesmayr M, Schindler K, Pernicka E, Schuh C, Schoeniger-Hekele A, Bauer P et al. Decreased food intake is a risk factor for mortality in hospitalised patients: the NutritionDay survey 2006. Clin Nutr 2009; 28: 484–491.
White JV, Guenter P, Jensen G, Malone A, Schofield M . Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). JPEN J Parenter Enteral Nutr 2012; 36: 275–283.
Ottery FD . Patient-Generated Subjective Global Assessment. In: McCallum PD, Polisena CG (eds) The Clinical Guide to Oncology Nutrition. The American Dietetic Association: Chicago, 2000, pp 11–23.
Kondrup J, Rasmussen HH, Hamberg O, Stanga Z . Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr 2003; 22: 321–336.
Elia M . The ‘MUST’ Report. Nutritional Screening of Adults: A Multidisciplinary Responsability. Development and Use of the ‘Malnutrition Universal Screening Tool’ (‘MUST’) for Adults. Malnutrition Advisory Group (MAG), a Standing Committee of the British Association of Parenteral and Enteral Nutrition (BAPEN): Redditch, 2003.
Lopes J, Russell DM, Whitwell J, Jeejeebhoy KN . Skeletal muscle function in malnutrition. Am J Clin Nutr 1982; 36: 602–610.
Humphreys J, de la Maza P, Hirsch S, Barrera G, Gattas V, Bunout D . Muscle strength as a predictor of loss of functional status in hospitalized patients. Nutrition 2002; 18: 616–620.
Russell DM, Leiter LA, Whitwell J, Marliss EB, Jeejeebhoy KN . Skeletal muscle function during hypocaloric diets and fasting: a comparison with standard nutritional assessment parameters. Am J Clin Nutr 1983; 37: 133–138.
Rantanen T, Volpato S, Ferrucci L, Heikkinen E, Fried LP, Guralnik JM . Handgrip strength and cause-specific and total mortality in older disabled women: exploring the mechanism. J Am Geriatr Soc 2003; 51: 636–641.
Norman K, Stobaus N, Gonzalez MC, Schulzke JD, Pirlich M . Hand grip strength: outcome predictor and marker of nutritional status. Clin Nutr 2011; 30: 135–142.
Windsor JA, Hill GL . Grip strength: a measure of the proportion of protein loss in surgical patients. Br J Surg 1988; 75: 880–882.
Guerra RS, Fonseca I, Pichel F, Restivo MT, Amaral TF . Handgrip strength and associated factors in hospitalized patients. JPEN J Parenter Enteral Nutr 2013; doi:10.1177/0148607113514113.
Flood A, Chung A, Parker H, Kearns V, O'Sullivan TA . The use of hand grip strength as a predictor of nutrition status in hospital patients. Clin Nutr 2014; 33: 106–114.
Matos LC, Tavares MM, Amaral TF . Handgrip strength as a hospital admission nutritional risk screening method. Eur J Clin Nutr 2007; 61: 1128–1135.
Luna-Heredia E, Martin-Pena G, Ruiz-Galiana J . Handgrip dynamometry in healthy adults. Clin Nutr 2005; 24: 250–258.
Frederiksen H, Hjelmborg J, Mortensen J, McGue M, Vaupel JW, Christensen K . Age trajectories of grip strength: cross-sectional and longitudinal data among 8,342 Danes aged 46 to 102. Ann Epidemiol 2006; 16: 554–562.
Gunther CM, Burger A, Rickert M, Crispin A, Schulz CU . Grip strength in healthy caucasian adults: reference values. J Hand Surg Am 2008; 33: 558–565.
Peolsson A, Hedlund R, Oberg B . Intra- and inter-tester reliability and reference values for hand strength. J Rehabil Med 2001; 33: 36–41.
Budziareck MB, Pureza Duarte RR, Barbosa-Silva MC . Reference values and determinants for handgrip strength in healthy subjects. Clin Nutr 2008; 27: 357–362.
Schlussel MM, dos Anjos LA, de Vasconcellos MT, Kac G . Reference values of handgrip dynamometry of healthy adults: a population-based study. Clin Nutr 2008; 27: 601–607.
Silva LF, Matos CM, Lopes GB, Martins MT, Martins MS, Arias LU et al. Handgrip strength as a simple indicator of possible malnutrition and inflammation in men and women on maintenance hemodialysis. J Ren Nutr 2011; 21: 235–245.
Mendes J, Azevedo A, Amaral TF . Handgrip strength at admission and time to discharge in medical and surgical inpatients. JPEN J Parenter Enteral Nutr 2014; 38: 481–488.
Kilgour RD, Vigano A, Trutschnigg B, Lucar E, Borod M, Morais JA . Handgrip strength predicts survival and is associated with markers of clinical and functional outcomes in advanced cancer patients. Support Care Cancer 2013; 21: 3261–3270.
Mahalakshmi VN, Ananthakrishnan N, Kate V, Sahai A, Trakroo M . Handgrip strength and endurance as a predictor of postoperative morbidity in surgical patients: can it serve as a simple bedside test? Int Surg 2004; 89: 115–121.
Bohannon RW, Schaubert KL . Test-retest reliability of grip-strength measures obtained over a 12-week interval from community-dwelling elders. J Hand Ther 2005; 18: 426–427.
ASPEN Board of Directors and the Clinical Guidelines Task Force. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enteral Nutr 2002; 26: 1SA–138SA.
Hodkinson HM . Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing 1972; 1: 233–238.
Charlson ME, Pompei P, Ales KL, MacKenzie CR . A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383.
Fess EE . Grip Strength, 2nd edn. American Society of Hand Therapists: Chicago, 1992.
Fess EE, Moran CA . Clinical Assessment Recommendations. American Society of Hand Therapists: Chicago, 1981.
Vaz M, Thangam S, Prabhu A, Shetty PS . Maximal voluntary contraction as a functional indicator of adult chronic undernutrition. Br J Nutr 1996; 76: 9–15.
Muscular weakness assessment: use of normal isometric strength data. The National Isometric Muscle Strength (NIMS) Database Consortium. Arch Phys Med Rehabil 1996; 77: 1251–1255.
Marfell-Jones M, Olds T, Stewart A, Carter L . International Standards for Anthropometric Assessment. International Standards for Anthropometric Assessment: Potchefstroom: South Africa, 2006.
Lee RD, Nieman DC . Assessment of the hospitalized patient. In: Lee RD, Nieman DC (eds). Nutritional Assessment, 4th edn. McGraw Hill Higher Education: Boston, 2007, pp 226–231.
Kwok T, Whitelaw MN . The use of armspan in nutritional assessment of the elderly. J Am Geriatr Soc 1991; 39: 492–496.
Chroni E, Paschalis C, Arvaniti C, Zotou K, Nikolakopoulou A, Papapetropoulos T . Carpal tunnel syndrome and hand configuration. Muscle Nerve 2001; 24: 1607–1611.
Guerra RS, Fonseca I, Pichel F, Restivo MT, Amaral TF . Hand length as an alternative measurement of height. Eur J Clin Nutr 2014; 68: 229–233.
Powell-Tuck J, Hennessy EM . A comparison of mid upper arm circumference, body mass index and weight loss as indices of undernutrition in acutely hospitalized patients. Clin Nutr 2003; 22: 307–312.
Pederson D, Gore C . Anthropometry Measurement Error. University of New South Wales Press: Sydney, Australia, 1996.
Fletcher RH, Fletcher SW . Diagnosis. In: Fletcher RW, Fletcher SW (eds). Clinical Epidemiology: The Essentials, 4th edn. Lippincott, Williams & Wilkins: Philadelphia, 2005, pp 35–58.
Hanley JA, McNeil BJ . The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 1982; 143: 29–36.
Kyle UG, Kossovsky MP, Karsegard VL, Pichard C . Comparison of tools for nutritional assessment and screening at hospital admission: a population study. Clin Nutr 2006; 25: 409–417.
Garcia MF, Meireles MS, Führ LM, Donini AB, Wazlawik E . Relationship between hand grip strength and nutritional assessment methods used of hospitalized patients. Rev Nutr 2013; 26: 49–57.
Haverkort EB, Binnekade JM, de Haan RJ, van Bokhorst-de van der Schueren MA . Handgrip strength by dynamometry does not identify malnutrition in individual preoperative outpatients. Clin Nutr 2012; 31: 647–651.
Pham NV, Cox-Reijven PL, Wodzig WK, Greve JW, Soeters PB . SGA and measures for muscle mass and strength in surgical Vietnamese patients. Nutrition 2007; 23: 283–291.
Mendes J, Alves P, Amaral TF . Comparison of nutritional status assessment parameters in predicting length of hospital stay in cancer patients. Clin Nutr 2014; 33: 466–470.
Norman K, Stobaus N, Reiss J, Schulzke J, Valentini L, Pirlich M . Effect of sexual dimorphism on muscle strength in cachexia. J Cachexia Sarcopenia Muscle 2012; 3: 111–116.
Mueller C, Compher C, Ellen DM . A.S.P.E.N. clinical guidelines: Nutrition screening, assessment, and intervention in adults. JPEN J Parenter Enteral Nutr 2011; 35: 16–24.
Acknowledgements
We thank Centro Hospitalar do Porto and all ward directors for facilitating the data collection. RSG as a Ph.D. student is receiving a scholarship from FCT – Fundação para a Ciência e a Tecnologia under the project (SFRH/BD/61656/2009).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Guerra, R., Fonseca, I., Pichel, F. et al. Handgrip strength cutoff values for undernutrition screening at hospital admission. Eur J Clin Nutr 68, 1315–1321 (2014). https://doi.org/10.1038/ejcn.2014.226
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2014.226
This article is cited by
-
Exploring grip strength as a predictor of depression in middle-aged and older adults
Scientific Reports (2021)
-
Post-traumatic stress disorder (PTSD) in mid-age and older adults differs by immigrant status and ethnicity, nutrition, and other determinants of health in the Canadian Longitudinal Study on Aging (CLSA)
Social Psychiatry and Psychiatric Epidemiology (2021)
-
Nutrition, Immigration and Health Determinants are Linked to Verbal Fluency among Anglophone Adults in the Canadian Longitudinal Study on Aging (CLSA)
The Journal of nutrition, health and aging (2020)
-
Depression in middle and older adulthood: the role of immigration, nutrition, and other determinants of health in the Canadian longitudinal study on aging
BMC Psychiatry (2019)