Abstract
Background/Objectives:
The current study was performed to investigate the effects of the Dietary Approaches to Stop Hypertension (DASH) eating plan on pregnancy outcomes in pregnant women with gestational diabetes mellitus (GDM).
Subjects/Methods:
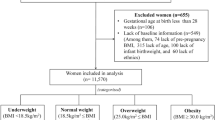
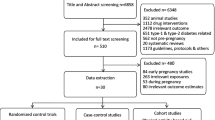
This randomized controlled clinical trial was performed among 52 women diagnosed with GDM. Participants were randomly assigned to consume either the control (n=26) or the DASH diet (n=26) for 4 weeks. The control diet was designed to contain 45–55% carbohydrates, 15–20% protein and 25–30% total fat. The DASH diet was rich in fruits, vegetables, whole grains and low-fat dairy products, and contained lower amounts of saturated fats, cholesterol and refined grains with a total of 2400 mg/day sodium. The numbers of women who commenced insulin therapy after dietary intervention, the mode of delivery and prevalence of polyhydramnios were assessed. The length, weight and head circumference of infants were measured during the first 24 h after birth.
Results:
Whereas 46.2% of women in the DASH diet needed to have a cesarean section, this percentage for the control group was 80.8% (P=0.01). The percentage of those who needed to commence insulin therapy after intervention was also significantly different between the two groups (23% for DASH vs 73% for control group, P<0.0001). Infants born to mothers on the DASH diet had significantly lower weight (3222.7 vs 3818.8 g, P<0.0001), head circumference (34.2 vs 35.1 cm, P=0.01) and ponderal index (2.50 vs 2.87 kg/m3, P<0.0001) compared with those born to mothers on the control diet.
Conclusions:
In conclusion, consumption of DASH diet for 4 weeks among pregnant women with GDM resulted in improved pregnancy outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Change history
04 May 2020
Editor's Note: The Co-Editors-in-Chief are currently investigating this article as concerns have been raised about integrity of the clinical trial reported here. There is also an ongoing investigation by the Iranian National Committee for Ethics in Biomedical Researches. Further editorial action will be taken as appropriate once the investigation into the concerns is complete and all parties have been given an opportunity to respond in full.
References
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2009; 32 (Suppl 1), S62–S67.
Schaefer-Graf UM, Klavehn S, Hartmann R, Kleinwechter H, Demandt N, Sorger M et al. How do we reduce the number of cases of missed postpartum diabetes in women with recent gestational diabetes mellitus? Diabetes Care 2009; 32: 1960–1964.
Karcaaltincaba D, Kandemir O, Yalvac S, Guvendag-Guven S, Haberal A . Prevalence of gestational diabetes mellitus and gestational impaired glucose tolerance in pregnant women evaluated by National Diabetes Data Group and Carpenter and Coustan criteria. Int J Gynaecol Obstet 2009; 106: 246–249.
Hossein-Nezhad A, Maghbooli Z, Vassigh AR, Larijani B . Prevalence of gestational diabetes mellitus and pregnancy outcomes in Iranian women. Taiwan J Obstet Gynecol 2007; 46: 236–241.
Reece EA . The fetal and maternal consequences of gestational diabetes mellitus. J Matern Fetal Neonatal Med 2010; 23: 199–203.
Boney CM, Verma A, Tucker R, Vohr BR . Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics 2005; 115: e290–e296.
Linne Y, Barkeling B, Rossner S . Natural course of gestational diabetes mellitus: long term follow up of women in the SPAWN study. BJOG 2002; 109: 1227–1231.
Gabbe SG, Graves CR . Management of diabetes mellitus complicating pregnancy. Obstet Gynecol 2003; 102: 857–868.
Louie JC, Brand-Miller JC, Markovic TP, Ross GP, Moses RG . Glycemic index and pregnancy: a systematic literature review. J Nutr Metab 2010; 2010: 282464.
Oostdam N, van Poppel MN, Wouters MG, van Mechelen W . Interventions for preventing gestational diabetes mellitus: a systematic review and meta-analysis. J Womens Health (Larchmt) 2011; 20: 1551–1563.
Moses RG, Barker M, Winter M, Petocz P, Brand-Miller JC . Can a low-glycemic index diet reduce the need for insulin in gestational diabetes mellitus? A randomized trial. Diabetes Care 2009; 32: 996–1000.
Louie JC, Markovic TP, Perera N, Foote D, Petocz P, Ross GP et al. A randomized controlled trial investigating the effects of a low-glycemic index diet on pregnancy outcomes in gestational diabetes mellitus. Diabetes Care 2011; 34: 2341–2346.
Vollmer WM, Sacks FM, Ard J, Appel LJ, Bray GA, Simons-Morton DG et al. Effects of diet and sodium intake on blood pressure: subgroup analysis of the DASH-sodium trial. Ann Intern Med 2001; 135: 1019–1028.
Azadbakht L, Fard NR, Karimi M, Baghaei MH, Surkan PJ, Rahimi M et al. Effects of the Dietary Approaches to Stop Hypertension (DASH) eating plan on cardiovascular risks among type 2 diabetic patients: a randomized crossover clinical trial. Diabetes Care 2011; 34: 55–57.
Azadbakht L, Mirmiran P, Esmaillzadeh A, Azizi T, Azizi F . Beneficial effects of a Dietary Approaches to Stop Hypertension eating plan on features of the metabolic syndrome. Diabetes Care 2005; 28: 2823–2831.
Azadbakht L, Surkan PJ, Esmaillzadeh A, Willett WC . The Dietary Approaches to Stop Hypertension eating plan affects C-reactive protein, coagulation abnormalities, and hepatic function tests among type 2 diabetic patients. J Nutr 2011; 141: 1083–1088.
Moses RG, Luebcke M, Davis WS, Coleman KJ, Tapsell LC, Petocz P et al. Effect of a low-glycemic-index diet during pregnancy on obstetric outcomes. Am J Clin Nutr 2006; 84: 807–812.
Jehan I, Zaidi S, Rizvi S, Mobeen N, McClure EM, Munoz B et al. Dating gestational age by last menstrual period, symphysis-fundal height, and ultrasound in urban Pakistan. Int J Gynaecol Obstet 2010; 110: 231–234.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2012; 35 (Suppl 1), S64–S71.
Boulet SL, Alexander GR, Salihu HM, Pass M . Macrosomic births in the United States: determinants, outcomes, and proposed grades of risk. Am J Obstet Gynecol 2003; 188: 1372–1378.
Bener A, Saleh NM, Al-Hamaq A . Prevalence of gestational diabetes and associated maternal and neonatal complications in a fast-developing community: global comparisons. Int J Womens Health 2011; 3: 367–373.
Jelsema RD . Management of diabetes mellitus complicating pregnancy. Obstet Gynecol 2004; 103: 586.
Scholl TO, Chen X, Stein P . Maternal vitamin D status and delivery by cesarean. Nutrients 2012; 4: 319–330.
Merewood A, Mehta SD, Chen TC, Bauchner H, Holick MF . Association between vitamin D deficiency and primary cesarean section. J Clin Endocrinol Metab 2009; 94: 940–945.
Peticca P, Keely EJ, Walker MC, Yang Q, Bottomley J . Pregnancy outcomes in diabetes subtypes: how do they compare? A province-based study of Ontario, 2005-2006. J Obstet Gynaecol Can 2009; 31: 487–496.
Tan PC, Ling LP, Omar SZ . The 50-g glucose challenge test and pregnancy outcome in a multiethnic Asian population at high risk for gestational diabetes. Int J Gynaecol Obstet 2009; 105: 50–55.
Moini A, Riazi K, Ebrahimi A, Ostovan N . Caesarean section rates in teaching hospitals of Tehran: 1999–2003. East Mediterr Health J 2007; 13: 457–460.
Bozorgan TJ, Lashgari MM . Association of the serum glucose level with fetal-maternal complications of gestational diabetes with insulin therapy. Acta Med Iran 2011; 49: 442–446.
Badakhsh MH, Khamseh ME, Malek M, Shafiee G, Aghili R, Moghimi S et al. A thirty-year analysis of cesarean section rate in gestational diabetes and normal pregnant population in Tehran, Iran: a concerning trend. Gynecol Endocrinol 2012; 28: 436–439.
Lee YM, D'Alton ME . Cesarean delivery on maternal request: maternal and neonatal complications. Curr Opin Obstet Gynecol 2008; 20: 597–601.
Papandreou L, Chasiotis G, Seferiadis K, Thanasoulias NC, Dousias V, Tsanadis G et al. Calcium levels during the initiation of labor. Eur J Obstet Gynecol Reprod Biol 2004; 115: 17–22.
Lewis S, Lucas RM, Halliday J, Ponsonby AL . Vitamin D deficiency and pregnancy: from preconception to birth. Mol Nutr Food Res 2010; 54: 1092–1102.
Kisters K, Gremmler B, Hausberg M . Preventing pregnancy-induced hypertension: the role of calcium and magnesium. J Hypertens 2006; 24: 201.
Bar J, Ben-Haroush A, Feldberg D, Hod M . The pharmacologic approach to the prevention of preeclampsia: from antiplatelet, antithrombosis and antioxidant therapy to anticonvulsants. Curr Med Chem Cardiovasc Hematol Agents 2005; 3: 181–185.
Tomkins A . Nutrition and maternal morbidity and mortality. Br J Nutr 2001; 85 (Suppl 2), S93–S99.
Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, Illuzzi JL . Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol 2011; 118: 29–38.
Niromanesh S, Alavi A, Sharbaf FR, Amjadi N, Moosavi S, Akbari S . Metformin compared with insulin in the management of gestational diabetes mellitus: a randomized clinical trial. Diabetes Res Clin Pract 2012; 98: 422–429.
Grant SM, Wolever TM, O'Connor DL, Nisenbaum R, Josse RG . Effect of a low glycaemic index diet on blood glucose in women with gestational hyperglycaemia. Diabetes Res Clin Pract 2011; 91: 15–22.
Hinderliter AL, Babyak MA, Sherwood A, Blumenthal JA . The DASH diet and insulin sensitivity. Curr Hypertens Rep 2011; 13: 67–73.
Ard JD, Grambow SC, Liu D, Slentz CA, Kraus WE, Svetkey LP . The effect of the PREMIER interventions on insulin sensitivity. Diabetes Care 2004; 27: 340–347.
Lien LF, Brown AJ, Ard JD, Loria C, Erlinger TP, Feldstein AC et al. Effects of PREMIER lifestyle modifications on participants with and without the metabolic syndrome. Hypertension 2007; 50: 609–616.
Macan M, Vrkic N, Vrdoljak AL, Radic B, Bradamante V . Effects of high sucrose diet, gemfibrozil, and their combination on plasma paraoxonase 1 activity and lipid levels in rats. Acta Biochim Pol 2010; 57: 321–326.
Tay A, Ozcelikay AT, Altan VM . Effects of L-arginine on blood pressure and metabolic changes in fructose-hypertensive rats. Am J Hypertens 2002; 15: 72–77.
Rowe WJ . Correcting magnesium deficiencies may prolong life. Clin Interv Aging 2012; 7: 51–54.
Kew S, Ye C, Sermer M, Connelly PW, Hanley AJ, Zinman B et al. Postpartum metabolic function in women delivering a macrosomic infant in the absence of gestational diabetes mellitus. Diabetes Care 2011; 34: 2608–2613.
Ostlund I, Hanson U, Bjorklund A, Hjertberg R, Eva N, Nordlander E et al. Maternal and fetal outcomes if gestational impaired glucose tolerance is not treated. Diabetes Care 2003; 26: 2107–2111.
Clapp JF . Effect of dietary carbohydrate on the glucose and insulin response to mixed caloric intake and exercise in both nonpregnant and pregnant women. Diabetes Care 1998; 21 (Suppl 2), B107–B112.
Scholl TO, Chen X, Khoo CS, Lenders C . The dietary glycemic index during pregnancy: influence on infant birth weight, fetal growth, and biomarkers of carbohydrate metabolism. Am J Epidemiol 2004; 159: 467–474.
Catalano PM, Hauguel-De Mouzon S . Is it time to revisit the Pedersen hypothesis in the face of the obesity epidemic? Am J Obstet Gynecol 2011; 204: 479–487.
Ornoy A . Prenatal origin of obesity and their complications: gestational diabetes, maternal overweight and the paradoxical effects of fetal growth restriction and macrosomia. Reprod Toxicol 2011; 32: 205–212.
Acknowledgements
The present study was supported by a Grant (No. 91104) from the Vice-Chancellor for Research, KUMS, Kashan, Iran. We thank the staff of Naghavi and Shaheed Beheshti Clinics (Kashan, Iran) for their assistance in this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Contributors: ZA conducted the study, carried out the statistical analysis, wrote the manuscript and contributed in the interpretation of the findings; ZT supervised the study; MS supervised the study and assisted in writing the manuscript; AE contributed in conception and study design and advised on statistical analyses, contributed in drafting the manuscript and assisted in interpretation of the findings. All authors approved the final version of the manuscript.
Rights and permissions
About this article
Cite this article
Asemi, Z., Samimi, M., Tabassi, Z. et al. The effect of DASH diet on pregnancy outcomes in gestational diabetes: a randomized controlled clinical trial. Eur J Clin Nutr 68, 490–495 (2014). https://doi.org/10.1038/ejcn.2013.296
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2013.296
Keywords
This article is cited by
-
Does a high dietary intake of resistant starch affect glycaemic control and alter the gut microbiome in women with gestational diabetes? A randomised control trial protocol
BMC Pregnancy and Childbirth (2022)
-
Community-based non-pharmacological interventions for pregnant women with gestational diabetes mellitus: a systematic review
BMC Women's Health (2022)
-
Gestational diabetes mellitus in association with macrosomia in Iran: a meta-analysis
Journal of Diabetes & Metabolic Disorders (2019)
-
Associations of the dietary approaches to stop hypertension (DASH) diet with pregnancy complications in Project Viva
European Journal of Clinical Nutrition (2018)
-
Is gestational diabetes mellitus an independent risk factor for macrosomia: a meta-analysis?
Archives of Gynecology and Obstetrics (2015)