Abstract
Background/objectives:
In the era of modern multidisciplinary clinical management, very little is known about the prevalence and presentation of malnutrition in children with gastrointestinal disorders (GastroD) particularly employing composite, global measures of nutritional status.
Subjects/methods:
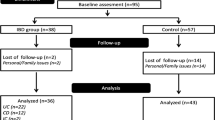
Anthropometry, body composition, dietary intake, eating habits and grip strength were assessed with bedside methods in 168 patients from outpatient gastroenterology clinics (n, median (IQR) years; Crohn’s disease (CD): n=53, 14.2 (11.6:15.4); ulcerative colitis (UC): n=27, 12.2 (10.7:14.2); coeliac disease: n=31, 9.3 (7.5:13.6); other GastroD: n=57, 9.8 (7.2:13.8)) and compared with 62 contemporary healthy controls (n, median (IQR): 9.8 (6.9:13.8)) and the results of the recent UK, National Diet and Nutritional Survey (NDNS).
Results:
Children with CD had lower BMI z-scores than controls (median (IQR): −0.3 (−0.9:0.4) vs 0.3 (−0.6:1.4); P=0.02) but only 2% were classified as thin (BMI z-score <−2 s.d.). The prevalence of obesity in children with UC was 19%, 6% in CD, 11% in children with other GastroD and 15% in controls. No difference was found in grip strength measurement between groups. Except for CD children, the proportion of patients with suboptimal micronutrient intake was similar to that of controls and the cohort of children from the latest NDNS. A higher proportion of children with CD had suboptimal intake for riboflavin, vitamin B6 and calcium and consumed significantly more meat products, juices (including carbonated drinks), spreads/jams and crisps and savoury snacks and significantly fewer portions of dairy, fish, fruits and vegetables compared with healthy controls.
Conclusions:
GastroD affect children’s body composition, growth, strength, dietary intake and eating habits, particularly CD, but to a lesser extent than expected.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Gee MI, Grace MG, Wensel RH, Sherbaniuk RW, Thomson AB . Nutritional status of gastroenterology outpatients: comparison of inflammatory bowel disease with functional disorders. J Am Diet Assoc 1985; 85: 1591–1599.
Sentongo TA, Semeao EJ, Piccoli DA, Stallings VA, Zemel BS . Growth, body composition, and nutritional status in children and adolescents with Crohn's disease. J Pediatr Gastroenterol Nutr 2000; 31: 33–40.
Filippi J, Al-Jaouni R, Wiroth JB, Hebuterne X, Schneider SM . Nutritional deficiencies in patients with Crohn's disease in remission. Inflamm Bowel Dis 2006; 12: 185–191.
Sousa GC, Cravo M, Costa AR, Miranda A, Tavares L, Moura-Santos P et al. A comprehensive approach to evaluate nutritional status in Crohn's patients in the era of biologic therapy: a case-control study. Am J Gastroenterol 2007; 102: 2551–2556.
Thomas AG, Taylor F, Miller V . Dietary intake and nutritional treatment in childhood Crohn's disease. J Pediatr Gastroenterol Nutr 1993; 17: 75–81.
Vasseur F, Gower-Rousseau C, Vernier-Massouille G, Dupas JL, Merle V, Merlin B et al. Nutritional status and growth in pediatric Crohn's disease: a population-based study. Am J Gastroenterol 2010; 105: 1893–1900.
Reilly NR, Aguilar K, Hassid BG, Cheng J, Defelice AR, Kazlow P et al. Celiac disease in normal-weight and overweight children: clinical features and growth outcomes following a gluten-free diet. J Pediatr Gastroenterol Nutr 2011; 53: 528–531.
McNeill G, Masson LF, Craig LC, Macdiarmid JI, Holmes BA, Nelson M et al. Sugar and fat intake among children in Scotland: what is needed to reach the dietary targets? Public Health Nutr 2010; 13: 1286–1294.
Department of Health. Dietary Reference Values for Food and energy and Nutrients for the United Kingdom. Report of the Panel on dietary Reference Values of the Committee on Medical Aspects of Food Policy 1991.
Department of Heath. National Diet and Nutritional Survey: Headline Results from Years 1, 2, 3 (combined) of the Rolling Programme 2008/2009-2010/11. 2012.
Cole TJ, Freeman JV, Preece MA . British 1990 growth reference centiles for weight, height, body mass index and head circumference fitted by maximum penalized likelihood. Stat Med 1998; 17: 407–429.
Wright CM, Sherriff A, Ward SC, McColl JH, Reilly JJ, Ness AR . Development of bioelectrical impedance-derived indices of fat and fat-free mass for assessment of nutritional status in childhood. Eur J Clin Nutr 2008; 62: 210–217.
Sherriff A, Wright CM, Reilly JJ, McColl J, Ness A, Emmett P . Age- and sex-standardised lean and fat indices derived from bioelectrical impedance analysis for ages 7-11 years: functional associations with cardio-respiratory fitness and grip strength. Br J Nutr 2009; 101: 1753–1760.
Rauch F, Neu CM, Wassmer G, Beck B, Rieger-Wettengl G, Rietschel E et al. Muscle analysis by measurement of maximal isometric grip force: new reference data and clinical applications in pediatrics. Pediatr Res 2002; 51: 505–510.
Kugathasan S, Nebel J, Skelton JA, Markowitz J, Keljo D, Rosh J et al. Body mass index in children with newly diagnosed inflammatory bowel disease: observations from two multicenter North American inception cohorts. J Pediatr 2007; 151: 523–527.
Burnham JM, Shults J, Semeao E, Foster BJ, Zemel BS, Stallings VA et al. Body-composition alterations consistent with cachexia in children and young adults with Crohn disease. Am J Clin Nutr 2005; 82: 413–420.
Wells JC, Fewtrell MS . Measuring body composition. Arch Dis Child 2006; 91: 612–617.
Reilly JJ, Gerasimidis K, Paparacleous N, Sherriff A, Carmichael A, Ness AR et al. Validation of dual-energy x-ray absorptiometry and foot-foot impedance against deuterium dilution measures of fatness in children. Int J Pediatr Obes 2010; 5: 111–115.
Williams JE, Wells JC, Wilson CM, Haroun D, Lucas A, Fewtrell MS . Evaluation of Lunar Prodigy dual-energy X-ray absorptiometry for assessing body composition in healthy persons and patients by comparison with the criterion 4-component model. Am J Clin Nutr 2006; 83: 1047–1054.
Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing 2011; 40: 423–429.
Hendricks KM, Williams E, Stoker TW, Schoenfeld DA, Walker WA, Kleinman RE . Dietary intake of adolescents with Crohn's disease. J Am Diet Assoc 1994; 94: 441–444.
Bingham SA . Limitations of the various methods for collecting dietary intake data. Ann Nutr Metab 1991; 35: 117–127.
Hou JK, Abraham B, El-Serag H . Dietary intake and risk of developing inflammatory bowel disease: a systematic review of the literature. Am J Gastroenterol 2011; 106: 563–573.
Ohlund K, Olsson C, Hernell O, Ohlund I . Dietary shortcomings in children on a gluten-free diet. J Hum Nutr Diet 2010; 23: 294–300.
Vagianos K, Bector S, McConnell J, Bernstein CN . Nutrition assessment of patients with inflammatory bowel disease. JPEN J Parenter Enteral Nutr 2007; 31: 311–319.
Scott EM, Gaywood I, Scott BB . Guidelines for osteoporosis in coeliac disease and inflammatory bowel disease. British Society of Gastroenterology. Gut 2000; 46 (Suppl 1), i1–i8.
Persad R, Jaffer I, Issenman RM . The prevalence of long bone fractures in pediatric inflammatory bowel disease. J Pediatr Gastroenterol Nutr 2006; 43: 597–602.
Abrams SA . Vitamin D requirements of children: ‘all my life's a circle’. Nutr Rev 2012; 70: 201–206.
Goodhand JR, Kamperidis N, Rao A, Laskaratos F, McDermott A, Wahed M et al. Prevalence and management of anemia in children, adolescents, and adults with inflammatory bowel disease. Inflamm Bowel Dis 2012; 18: 513–519.
Gerasimidis K, McGrogan P, Edwards CA . The aetiology and impact of malnutrition in paediatric inflammatory bowel disease. J Hum Nutr Diet 2011; 24: 313–326.
Gerasimidis K, McGrogan P, Hassan K, Edwards CA . Dietary modifications, nutritional supplements and alternative medicine in paediatric patients with inflammatory bowel disease. Aliment Pharmacol Ther 2008; 27: 155–165.
Jowett SL, Seal CJ, Phillips E, Gregory W, Barton JR, Welfare MR . Dietary beliefs of people with ulcerative colitis and their effect on relapse and nutrient intake. Clin Nutr 2004; 23: 161–170.
Cameron FL, Gerasimidis K, Papangelou A, Missiou D, Garrick V, Cardigan T et al. Clinical progress in the two years following a course of exclusive enteral nutrition in 109 paediatric patients with Crohn's disease. Aliment Pharmacol Ther 2013; 37: 622–629.
Acknowledgements
This study was funded by the Greek State Scholarship Foundation and the Hellenic Foundation of Gastroenterology & Nutrition. The IBD team at Yorkhill Hospital, Glasgow are supported by the Catherine McEwan Foundation and Yorkhill IBD fund. RKR is supported by an NHS Research Scotland career fellowship award.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
PM received an education grant from Cow & Gate and speaker’s fees from Nestle, MSD, Mead Johnson. RR received consultancy fees from Merck, Shape and Dome, honoraria from Nestle and MSD and an educational grant from Mead Johnson. DF received honoraria from Fresenius Kabi and financial support to attend conferences by Danone. CAE received travel expenses by ISLI Europe. None of the remaining co-authors has to declare a conflict of interest relevant to this study.
Additional information
Part of this work was presented at the Annual ESPEN conference 2012 in Barcelona, Spain.
Contributors: JEW, JU, KM, EB, TC and DD carried out the participants’ recruitment, MT and KG carried out statistical data analyses and drafted the manuscript. KG, CAE, PM, DF, JB, RKR and AB participated in the design of the study coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Rights and permissions
About this article
Cite this article
Tsiountsioura, M., Wong, J., Upton, J. et al. Detailed assessment of nutritional status and eating patterns in children with gastrointestinal diseases attending an outpatients clinic and contemporary healthy controls. Eur J Clin Nutr 68, 700–706 (2014). https://doi.org/10.1038/ejcn.2013.286
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2013.286
Keywords
This article is cited by
-
Habitual dietary intake of IBD patients differs from population controls: a case–control study
European Journal of Nutrition (2021)
-
Nutritional status and body composition in children with inflammatory bowel disease: a prospective, controlled, and longitudinal study
European Journal of Clinical Nutrition (2020)
-
Nutritional status and food intake in pediatric patients with inflammatory bowel disease at diagnosis significantly differs from healthy controls
European Journal of Pediatrics (2019)
-
Paediatric Patients with Coeliac Disease on a Gluten-Free Diet: Nutritional Adequacy and Macro- and Micronutrient Imbalances
Current Gastroenterology Reports (2018)
-
Environmental Triggers for IBD
Current Gastroenterology Reports (2014)