Abstract
Background/objectives:
Some studies document relationships of the incidence of gestational diabetes mellitus (GDM) with individual components of the diet, but studies exploring relationships with patterns of eating are lacking. This observational study aimed to explore a possible relationship between the incidence of GDM and the Mediterranean diet (MedDiet) pattern of eating.
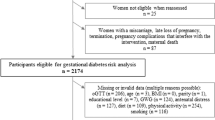
Subjects/methods:
In 10 Mediterranean countries, 1076 consecutive pregnant women underwent a 75-g OGTT at the 24th–32nd week of gestation, interpreted both by the ADA_2010 and the International Association of the Diabetes and Pregnancy Study Groups (IADPSG)_2012 criteria. The dietary habits were assessed by a previously validated questionnaire and a Mediterranean Diet Index (MDI) was computed, reflecting the degree of adherence to the MedDiet pattern of eating: a higher MDI denoting better adherence.
Results:
After adjustment for age, BMI, diabetes in the family, weight gain and energy intake, subjects with GDM, by either criterion, had lower MDI (ADA_2010, 5.8 vs 6.3, P=0.028; IADPSG_2012, 5.9 vs 6.4, P<0.001). Moreover, the incidence of GDM was lower in subjects with better adherence to the MedDiet (higher tertile of MDI distribution), 8.0% vs 12.3%, OR=0.618, P=0.030 by ADA_2010 and 24.3% vs 32.8%, OR=0.655, P=0.004 by IADPSG_2012 criteria. In subjects without GDM, MDI was negatively correlated with both fasting plasma glucose and AUC glucose, P<0.001 for both.
Conclusions:
Adherence to a MedDiet pattern of eating is associated with lower incidence of GDM and better degree of glucose tolerance, even in women without GDM. The possibility to use MedDiet for the prevention of GDM deserves further testing with intervention studies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
American Diabetes Association. Standards of medical care in diabetes. Diabetes Care 2012; 35: S11–S63.
Zimmet P, Alberti KG, Shaw J . Global and societal implications of the diabetes epidemic. Nature 2001; 414: 782–787.
Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care 1997; 20: 537–544.
American Diabetes Association. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care 2002; 25: 50–60.
Feskens EJ, Kromhout D . Cardiovascular risk factors and the 25-year incidence of diabetes mellitus in middle-aged men. The Zutphen Study. Am J Epidemiol 1989; 130: 1101–1108.
Colditz GA, Manson JE, Stampfer MJ, Rosner B, Willett WC, Speizer FE . Diet and risk of clinical diabetes in women. Am J Clin Nutr 1992; 55: 1018–1023.
Salmeron J, Manson JE, Stampfer MJ, Colditz GA, Wing AL, Willett WC . Dietary fiber, glycemic load and risk of noninsulin-dependent diabetes mellitus in women. JAMA 1997; 277: 472–477.
Salmeron J, Hu FB, Manson JE, Stampfer MJ, Colditz GA, Rimm EB et al. Dietary fiber intake and risk of type 2 diabetes in women. Am J Clin Nutr 2001; 13: 1019–1027.
Salmeron J, Ascherio A, Rimm EB, Colditz GA, Spiegelman D, Jenkins DJ et al. Dietary fiber, glycemic load and risk of NIDDM in men. Diabetes Care 1997; 20: 545–550.
Meyer KA, Kushi LH, Jacobs DR Jr, Slavin J, Sellers TA, Folsom AR . Carbohydrates, dietary fiber and incident type 2 diabetes in older women. Am J Clin Nutr 2000; 71: 921–930.
Feskens EJ, Kromhout D . Habitual dietary intake and glucose intolerance in euglycaemic men. The Zutphen Study. Int J Epidemiol 1990; 19: 953–959.
Trevisan M, Krogh V, Freudenheim J . Consumption of olive oil, butter and vegetable oils and coronary heart disease risk factors. The Research Group ATS-RF2 of the Italian National Research Council. JAMA 1990; 263: 688–692.
Thanopoulou A, Karamanos B, Angelico FV, Assaad-Khalil SH, Barbato AF, Del Ben MP et al. Dietary fat intake as risk factor for the development of diabetes. Multinational, multicenter study of the Mediterranean Group for the Study of Diabetes (MGSD) Diabetes Care 2003; 26: 302–307.
Perez-Jimenez F, Lopez-Mranda J, Pinillos MD, Gómez P, Paz-Rojas E, Montilla P et al. A Mediterranean and a high- CHO diet improve glucose metabolism in healthy young persons. Diabetologia 2001; 44: 2038–2043.
Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P et alfor the Finnish Diabetes Prevention Study Group. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001; 344: 1343–1350.
Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403.
Bo S, Menato G, Lezo A, Signorile A, Bardelli C, De Michieli F et al. Dietary fat and gestational hyperglycaemia. Diabetologia 2001; 44: 972–978.
González-Clemente JM, Carro O, Gallach I, Vioque J, Humanes A, Sauret C et al. Increased cholesterol intake in women with gestational diabetes. Diabetes Metab 2007; 33: 25–29.
Qiu C, Fredric IO, Zhang C, Sorensen TK, Enquobahrie DA, Williams MA . Risk of gestational diabetes in relation to maternal egg and cholesterol intake. Am J Epidemiol 2011; 173: 649–658.
Saldana TM, Siega-Riz AM, Adair LS . Effect of macronutrient intake on the development of glucose intolerance during pregnancy. Am J Clin Nutr 2004; 79: 479–486.
Wang Y, Storlien LH, Jenkins AB, Tapsell LC, Jin Y, Pan JF et al. Dietary variables and glucose tolerance in pregnancy. Diabetes Care 2000; 23: 460–464.
Moses RG, Shand JL, Tapsell LC . The recurrence of gestational diabetes: could dietary differences in fat intake be an explanation? Diabetes Care 1997; 20: 1647–1650.
Zhang C, Liu S, Solomon CG, Hu FB . Dietary fiber intake, dietary glycemic load, and the risk for gestational diabetes mellitus. Diabetes Care 2006; 29: 2223–2230.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2010; 33: S62–S69.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2012; 35: S64–S71.
Karamanos B, Thanopoulou A, Angelico F, Assaad-Khalil S, Barbato A, Del Ben M et al. Multi-centre study of the Mediterranean Group for the Study of Diabetes (MGSD). Nutritional habits in the Mediterranean Basin The macronutrient composition of diet and its relation with the traditional Mediterranean diet. Eur J Clin Nutr 2002; 56: 983–991.
Toeller M, Kiischan A, Heitkamp G, Schumacher W, Milne R, Buyken A et althe EURODIAB IDDM Complications Study Group. Nutritional intake of 2868 IDDM patients from 30 centres in Europe. Diabetologia 1996; 39: 929–939.
Erkkola M, Karppinen M, Javanainen J, Rasanen L, Knip M, Virtanen SM . Validity and reproducibility of a food frequency questionnaire for pregnant Finnish women. Am J Epidemiol 2001; 154: 466–476.
Willet WC, Sacks F, Trichopoulou A, Drescher C, Ferro-Luzzi A, Helsing E et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr 1995; 61: 1402S–1406S.
Trichopoulou A, Kouris-Blazos A, Wahlqvist ML, Gnardellis C, Lagiou P, Polychronopoulos E et al. Diet and overall survival in elderly people. Br Med J 1995; 311: 157–160.
Kromhout D, Keys A, Aravanis C, Buzina R, Fidanza F, Giampaoli S . Food consumption patterns in the 1960s in seven countries. Am J Clin Nutr 1989; 49: 889–894.
Thanopoulou AC, Karamanos BG, Angelico FV, Assaad-Khalil SH, Barbato AF, Del Ben MP et al. Dietary fat intake as risk factor for the development of diabetes: multinational, multicenter study of the Mediterranean Group for the Study of Diabetes (MGSD). Diabetes Care 2003; 26: 302–307.
Feskens EJ, Virtanen SM, Räsänen L, Tuomilehto J, Stengård J, Pekkanen J et al. Dietary factors determining diabetes and impaired glucose tolerance. A 20-year follow-up of the Finnish and Dutch cohorts of the Seven Countries Study. Diabetes Care 1995; 18: 1104–1112.
Gittelsohn J, Wolever TM, Harris SB, Harris-Giraldo R, Hanley AJ, Zinman B . Specific patterns of food consumption and preparation are associated with diabetes and obesity in a Native Canadian community. J Nutr 1998; 128: 541–547.
Martinez-Gonzalez MA, de la Fuente-Arrillaga C, Nunez-Cordoba JM, Basterra-Gortari FJ, Beunza JJ, Vazquez Z et al. Adherence to Mediterranean diet and risk of developing diabetes: prospective cohort study. BMJ 2008; 336: 1348–1351.
Panagiotakos DB, Pitsavos C, Chrysohoou C, Stefanadis C . The epidemiology of Type 2 diabetes mellitus in Greek adults: the ATTICA study. Diabet Med 2005; 22: 1581–1588.
Mozaffarian D, Marfisi R, Levantesi G, Silletta MG, Tavazzi L, Tognoni G et al. Incidence of new-onset diabetes and impaired fasting glucose in patients with recent myocardial infarction and the effect of clinical and lifestyle risk factors. Lancet 2007; 370: 667–675.
Salas-Salvadó J, Bulló M, Babio N, Martínez-González MÁ, Ibarrola-Jurado N, Basora J et al. Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial PREDIMED Study Investigators. Diabetes Care 2011; 34: 14–19.
Zhang C, Schulze MB, Solomon CG, Hu FB . A prospective study of dietary patterns, meat intake and risk of gestational diabetes mellitus. Diabetologia 2006; 49: 2604–2613.
Tobias DK, Zhang C, Chavarro J, Bowers K, Rich-Edwards J, Rosner B et al. Prepregnancy adherence to dietary patterns and lower risk of gestational diabetes mellitus. Am J Clin Nutr 2012; 96: 289–295.
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D . Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med 2003; 348: 2599–2608.
Trichopoulou A, Orfanos P, Norat T, Bueno-de-Mesquita B, Ocké MC, Peeters PH et al. Modified Mediterranean diet and survival: EPIC-elderly prospective cohort study. BMJ 2005; 330: 991–998.
Fung TT, McCullough ML, Newby PK, Manson JE, Meigs JB, Rifai N et al. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr 2005; 82: 163–173.
Salas-Salvado J, Martinez-Gonzalez MA, Bullo M, Ros E . The role of diet in the prevention of type 2 diabetes. Nutr Metab Cardiovasc Dis 2011; 21: B32–B48.
Acknowledgements
The study was supported by grants from the Mediterranean Group for the Study of Diabetes (MGSD).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix
Appendix
All participating investigators are listed, by country:
The MGSD-GDM study group was composed of key investigators in each collaborating country, including: Algeria (M Bachaoui, F Kolli, Z Benghanem); France (M Marre); Greece (B Karamanos, E Anastasiou); Italy (A Lapolla, M G Dalfra, A Filippi, A Barison, R Valentini); Lebanon (C Saab); Malta (C Savona-Ventura, J Vassallo, J Craus); Morocco (H El Ghomari, F Louda, H Addi, M Joubij, A Chraibi); Serbia (A Jotic, N M Lalic, A Ljubic, M Gojnic, T Milicic, L Lukic, J Seferovic, M Macesic); Syria (N Albache, A Jalek, K Kebbewaer, M Albache); and Tunisia (C Ben Slama).
Rights and permissions
About this article
Cite this article
Karamanos, B., Thanopoulou, A., Anastasiou, E. et al. Relation of the Mediterranean diet with the incidence of gestational diabetes. Eur J Clin Nutr 68, 8–13 (2014). https://doi.org/10.1038/ejcn.2013.177
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2013.177
Keywords
This article is cited by
-
Maternal dietary components in the development of gestational diabetes mellitus: a systematic review of observational studies to timely promotion of health
Nutrition Journal (2023)
-
Adherence to the Mediterranean diet and risk of gestational diabetes: a prospective cohort study
BMC Pregnancy and Childbirth (2023)
-
Vitamin B12 status and folic acid/vitamin B12 related to the risk of gestational diabetes mellitus in pregnancy: a systematic review and meta-analysis of observational studies
BMC Pregnancy and Childbirth (2022)
-
The prevention of gestational diabetes mellitus (The role of lifestyle): a meta-analysis
Diabetology & Metabolic Syndrome (2022)
-
Adherence to the Mediterranean diet and its association with environmental footprints among women of childbearing age in the United Arab Emirates
European Journal of Nutrition (2022)