Abstract
Background/Objectives:
Postprandial hyperglycemia increases the risks of development of type 2 diabetes and cardiovascular diseases. The purpose of this study was to determine whether a 3-day low-carbohydrate/high-fat diet (LC/HFD) alters postprandial plasma glucose and incretin levels during oral glucose tolerance test (OGTT) in healthy men.
Subjects/Methods:
Nine healthy young men (age (mean±s.e.), 27±1 years; body mass index, 22±1 kg/m2) consumed either a normal diet (ND: energy from ∼22% fat) or a LC/HFD (energy from ∼69% fat) for 3 days each. The total energy intake from each diet was similar. An OGTT was performed after each 3-day dietary intervention. Postprandial plasma glucose, insulin, free fatty acid and glucagon-like peptide-1 (GLP-1) levels were determined at rest and during the OGTT.
Results:
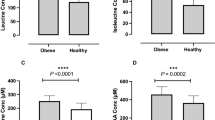
Plasma glucose levels and incremental area under the curve during the OGTT were significantly higher in the LC/HFD trial than in the ND trial (P=0.024). In addition, increase in GLP-1 levels was significantly higher in the LC/HFD trial than in the ND trial (P=0.025). The first-phase insulin secretion indexes were significantly lower in the LC/HFD trial than in the ND trial (P<0.041).
Conclusions:
These results demonstrate that even short-term LC/HFD increased postprandial plasma glucose and GLP-1 levels in healthy young men. A decrease in first-phase insulin secretion may partially contribute to the short-term LC/HFD-induced increase in postprandial plasma glucose levels.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
DECODE group. Glucose tolerance and mortality: comparison of WHO and American Diabetes Association diagnostic criteria. The DECODE study group. European Diabetes Epidemiology Group. Diabetes Epidemiology: Collaborative analysis Of Diagnostic criteria in Europe. Lancet 1999; 354: 617–621.
DECODE group. Glucose tolerance and cardiovascular mortality: comparison of fasting and 2-hour diagnostic criteria. Arch Intern Med 2001; 161: 397–405.
Nakagami T . Hyperglycaemia and mortality from all causes and from cardiovascular disease in five populations of Asian origin. Diabetologia 2004; 47: 385–394.
Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M . Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trial. Lancet 2002; 359: 2072–2077.
Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M . Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA 2003; 290: 486–494.
Kawamori R, Tajima N, Iwamoto Y, Kashiwagi A, Shimamoto K, Kaku K . Voglibose for prevention of type 2 diabetes mellitus: a randomised, double-blind trial in Japanese individuals with impaired glucose tolerance. Lancet 2009; 373: 1607–1614.
Kawano H, Motoyama T, Hirashima O, Hirai N, Miyao Y, Sakamoto T et al. Hyperglycemia rapidly suppresses flow-mediated endothelium-dependent vasodilation of brachial artery. J Am Coll Cardiol 1999; 34: 146–154.
Esposito K, Nappo F, Marfella R, Giugliano G, Giugliano F, Ciotola M et al. Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress. Circulation 2002; 106: 2067–2072.
Sakamoto T, Ogawa H, Kawano H, Hirai N, Miyamoto S, Takazoe K et al. Rapid change of platelet aggregability in acute hyperglycemia. Detection by a novel laser-light scattering method. Thromb Haemost 2000; 83: 475–479.
Bisschop PH, de Metz J, Ackermans MT, Endert E, Pijl H, Kuipers F et al. Dietary fat content alters insulin-mediated glucose metabolism in healthy men. Am J Clin Nutr 2001; 73: 554–559.
Chokkalingam K, Jewell K, Norton L, Littlewood J, van Loon LJ, Mansell P et al. High-fat/low-carbohydrate diet reduces insulin-stimulated carbohydrate oxidation but stimulates nonoxidative glucose disposal in humans: an important role for skeletal muscle pyruvate dehydrogenase kinase 4. J Clin Endocrinol Metab 2007; 92: 284–292.
Cooper JA, Watras AC, Shriver T, Adams AK, Schoeller DA . Influence of dietary fatty acid composition and exercise on changes in fat oxidation from a high-fat diet. J Appl Physiol 2010; 109: 1011–1018.
Hansen KC, Zhang Z, Gomez T, Adams AK, Schoeller DA . Exercise increases the proportion of fat utilization during short-term consumption of a high-fat diet. Am J Clin Nutr 2007; 85: 109–116.
Harber MP, Schenk S, Barkan AL, Horowitz JF . Alterations in carbohydrate metabolism in response to short-term dietary carbohydrate restriction. Am J Physiol Endocrinol Metab 2005; 289: E306–E312.
Peters SJ, Harris RA, Wu P, Pehleman TL, Heigenhauser GJ, Spriet LL . Human skeletal muscle PDH kinase activity and isoform expression during a 3-day high-fat/low-carbohydrate diet. Am J Physiol Endocrinol Metab 2001; 281: E1151–E1158.
Schrauwen P, van Marken Lichtenbelt WD, Westerterp KR . Changes in fat oxidation in response to a high-fat diet. Am J Clin Nutr 1997; 66: 276–282.
Brons C, Jensen CB, Storgaard H, Hiscock NJ, White A, Appel JS et al. Impact of short-term high-fat feeding on glucose and insulin metabolism in young healthy men. J Physiol 2009; 587: 2387–2397.
Bachmann OP, Dahl DB, Brechtel K, Machann J, Haap M, Maier T et al. Effects of intravenous and dietary lipid challenge on intramyocellular lipid content and the relation with insulin sensitivity in humans. Diabetes 2001; 50: 2579–2584.
Stettler R, Ith M, Acheson KJ, Decombaz J, Boesch C, Tappy L et al. Interaction between dietary lipids and physical inactivity on insulin sensitivity and on intramyocellular lipids in healthy men. Diabetes Care 2005; 28: 1404–1409.
Johnson NA, Stannard SR, Rowlands DS, Chapman PG, Thompson CH, O'Connor H et al. Effect of short-term starvation versus high-fat diet on intramyocellular triglyceride accumulation and insulin resistance in physically fit men. Exp Physiol 2006; 91: 693–703.
Drucker DJ, Nauck MA . The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet 2006; 368: 1696–1705.
Hirmsworth HP . The dietetic factor determining the glucose tolerance and sensitivity to insulin of healthy men. Clin Sci 1935; 2: 67–94.
Anderson JW, Herman RH . Effects of carbohydrate restriction on glucose tolerance of normal men and reactive hypoglycemic patients. Am J Clin Nutr 1975; 28: 748–755.
Sparti A, Decombaz J . Effect of diet on glucose tolerance 36 h after glycogen-depleting exercise. Eur J Clin Nutr 1992; 46: 377–385.
Pehleman TL, Peters SJ, Heigenhauser GJ, Spriet LL . Enzymatic regulation of glucose disposal in human skeletal muscle after a high-fat, low-carbohydrate diet. J Appl Physiol 2005; 98: 100–107.
Ministry of Health Labour Welfare of Japan. Dietary reference intakes for Japanese, 2010. Daiichi Shuppan: Tokyo, Japan, 2010; in Japanese.
Friedewald WT, Levy RI, Fredrickson DS . Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972; 18: 499–502.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Mari A, Pacini G, Murphy E, Ludvik B, Nolan JJ . A model-based method for assessing insulin sensitivity from the oral glucose tolerance test. Diabetes Care 2001; 24: 539–548.
Stumvoll M, Mitrakou A, Pimenta W, Jenssen T, Yki-Jarvinen H, Van Haeften T et al. Use of the oral glucose tolerance test to assess insulin release and insulin sensitivity. Diabetes Care 2000; 23: 295–301.
Cohen J . Statistical Power Analysis for the Behavioral Sciences. 2nd edn. Routledge Academic: UK, 1988.
Ferrannini E, Bjorkman O, Reichard GA, DeFronzo RA . The disposal of an oral glucose load in healthy subjects. A quantitative study. Diabetes 1985; 34: 580–588.
Swinburn BA, Boyce VL, Bergman RN, Howard BV, Bogardus C . Deterioration in carbohydrate metabolism and lipoprotein changes induced by modern, high fat diet in Pima Indians and Caucasians. J Clin Endocrinol Metab 1991; 73: 156–165.
Oprescu AI, Bikopoulos G, Naassan A, Allister EM, Tang C, Park E et al. Free fatty acid-induced reduction in glucose-stimulated insulin secretion: evidence for a role of oxidative stress in vitro and in vivo. Diabetes 2007; 56: 2927–2937.
Chaikomin R, Doran S, Jones KL, Feinle-Bisset C, O'Donovan D, Rayner CK et al. Initially more rapid small intestinal glucose delivery increases plasma insulin, GIP, and GLP-1 but does not improve overall glycemia in healthy subjects. Am J Physiol Endocrinol Metab 2005; 289: E504–E507.
Clegg ME, McKenna P, McClean C, Davison GW, Trinick T, Duly E et al. Gastrointestinal transit, post-prandial lipaemia and satiety following 3 days high-fat diet in men. Eur J Clin Nutr 2011; 65: 240–246.
Schrauwen P, Wagenmakers AJ, van Marken Lichtenbelt WD, Saris WH, Westerterp KR et al. Increase in fat oxidation on a high-fat diet is accompanied by an increase in triglyceride-derived fatty acid oxidation. Diabetes 2000; 49: 640–646.
Kiens B, Essen-Gustavsson B, Gad P, Lithell H . Lipoprotein lipase activity and intramuscular triglyceride stores after long-term high-fat and high-carbohydrate diets in physically trained men. Clin Physiol 1987; 7: 1–9.
Acknowledgements
This work was supported in part by a Grant-in-Aid for the Young Scientists (B) (22700703) and for the Global COE program ‘Sport Sciences for the promotion of Active Life’ (2010–2011) awarded by Ministry of Education, Culture, Sports Science and Technology of Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Numao, S., Kawano, H., Endo, N. et al. Short-term low carbohydrate/high-fat diet intake increases postprandial plasma glucose and glucagon-like peptide-1 levels during an oral glucose tolerance test in healthy men. Eur J Clin Nutr 66, 926–931 (2012). https://doi.org/10.1038/ejcn.2012.58
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2012.58
Keywords
This article is cited by
-
Modeling of postprandial glycemic response by consecutive reaction kinetics model for precise glycemic control
International Journal of Diabetes in Developing Countries (2023)
-
Pleurotus tuber-regium inclusion in diet ameliorates dyslipidaemia in obese-type 2 diabetic rats
Clinical Phytoscience (2021)
-
The effect of a low-carbohydrate high-fat diet and ethnicity on daily glucose profile in type 2 diabetes determined by continuous glucose monitoring
European Journal of Nutrition (2020)
-
Resistant maltodextrin or fructooligosaccharides promotes GLP-1 production in male rats fed a high-fat and high-sucrose diet, and partially reduces energy intake and adiposity
European Journal of Nutrition (2018)
-
A low-carbohydrate high-fat diet increases weight gain and does not improve glucose tolerance, insulin secretion or β-cell mass in NZO mice
Nutrition & Diabetes (2016)