Abstract
Background/objectives:
Evidence from prospective studies is consistent in showing an inverse association between dietary fibre intake and risk of ischaemic heart disease (IHD), but whether dietary fibre from various food sources differ in their effect on IHD risk is less clear. The objective of this study was to assess the associations of total and food sources of dietary fibre with IHD mortality in the European Prospective Investigation into Cancer and Nutrition-Heart study.
Subjects/methods:
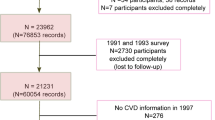
Participants were 306 331 men and women from eight European countries. Dietary fibre intake was assessed using centre or country-specific diet questionnaires and calibrated using a 24-h diet recall.
Results:
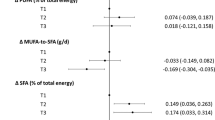
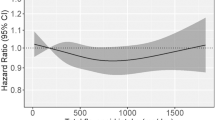
After an average follow-up of 11.5 years, there were 2381 IHD deaths among participants without cardiovascular disease at baseline. The calibrated intake of dietary fibre was inversely related with IHD mortality; each 10 g/day was associated with a 15% lower risk (relative risk (RR) 0.85; 95% confidence interval (CI): 0.73–0.99, P=0.031). There was no difference in the associations of the individual food sources of dietary fibre with the risk of IHD mortality; RR for each 5 g/day higher cereal fibre intake was 0.91 (CI: 0.82–1.01), RR for each 2.5 g/day fruit fibre intake was 0.94 (CI: 0.88–1.01) and RR for each 2.5 g/day vegetable fibre intake was 0.90 (95% CI: 0.76–1.07).
Conclusion:
A higher consumption of dietary fibre is associated with a lower risk of fatal IHD with no clear difference in the association with IHD for fibre from cereals, fruits or vegetables.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Trowell H . Ischemic heart disease and dietary fiber. Am J Clin Nutr 1972; 25: 926–932.
Burkitt DP, Walker ARP, Painter NS . Dietary fiber and disease. JAMA 1974; 229: 1068–1074.
Mente A, De Koning L, Shannon HS, Anand SS . A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med 2009; 169: 659–669.
Pereira MA, O'Reilly E, Augustsson K, Fraser GE, Goldbourt U, Heitmann BL et al. Dietary fiber and risk of coronary heart disease: a pooled analysis of cohort studies. Arch Intern Med 2004; 164: 370–376.
Eshak ES, Iso H, Date C, Kikuchi S, Watanabe Y, Wada Y et al. Dietary fiber intake is associated with reduced risk of mortality from cardiovascular disease among Japanese men and women. J Nutr 2010; 140: 1445–1453.
Mozaffarian D, Kumanyika SK, Lemaitre RN, Olson JL, Burke GL, Siscovick DS . Cereal, fruit, and vegetable fiber intake and the risk of cardiovascular disease in elderly individuals. JAMA 2003; 289: 1659–1666.
Streppel MT, Ocké MC, Boshuizen HC, Kok FJ, Kromhout D . Dietary fiber intake in relation to coronary heart disease and all-cause mortality over 40 y: The Zutphen Study. Am J Clin Nutr 2008; 88: 1119–1125.
Brown L, Rosner B, Willett WW, Sacks FM . Cholesterol-lowering effects of dietary fiber: A meta-analysis. Am J Clin Nutr 1999; 69: 30–42.
Riboli E, Hunt KJ, Slimani N, Ferrari P, Norat T, Fahey M et al. European Prospective Investigation into Cancer and Nutrition (EPIC): study populations and data collection. Public Health Nutr 2002; 5: 1113–1124.
Danesh J, Saracci R, Berglund G, Feskens E, Overvad K, Panico S et al. EPIC-Heart: The cardiovascular component of a prospective study of nutritional, lifestyle and biological factors in 520 000 middle-aged participants from 10 European countries. Eur J Epidemiol 2007; 22: 129–141.
Crowe FL, Roddam AW, Key TJ, Appleby PN, Overvad K, Jakobsen MU et al. Fruit and vegetable intake and mortality from ischaemic heart disease: results from the European Prospective Investigation into Cancer and Nutrition (EPIC)-Heart study. Eur Heart J 2011; 32: 1235–1243.
Bingham SA, Gill C, Welch A, Cassidy A, Runswick SA, Oakes S et al. Validation of dietary assessment methods in the UK arm of EPIC using weighed records, and 24-h urinary nitrogen and potassium and serum vitamin C and carotenoids as biomarkers. Int J Epidemiol 1997; 26: S137–S151.
Bohlscheid-Thomas S, Hoting I, Boeing H, Wahrendorf J . Reproducibility and relative validity of energy and macronutrient intake of a food frequency questionnaire developed for the German part of the EPIC project. Int J Epidemiol 1997; 26: S71–S81.
Katsouyanni K, Rimm EB, Gnardellis C, Trichopoulos D, Polychronopoulos E, Trichopoulou A . Reproducibility and relative validity of an extensive semi-quantitative food frequency questionnaire using dietary records and biochemical markers among Greek schoolteachers. Int J Epidemiol 1997; 26: S118–S127.
Ocké MC, Bueno-De-Mesquita HB, Pols MA, Smit HA, Van Staveren WA, Kromhout D . The Dutch EPIC Food Frequency Questionnaire. II. Relative validity and reproducibility for nutrients. Int J Epidemiol 1997; 26: S49–S58.
Pisani P, Faggiano F, Krogh V, Palli D, Vineis P, Berrino F . Relative validity and reproducibility of a food frequency dietary questionnaire for use in the Italian EPIC centres. Int J Epidemiol 1997; 26: S152–S160.
Riboli E, Elmståhl S, Saracci R, Gullberg B, Lindgärde F . The Malmo Food Study: Validity of two dietary assessment methods for measuring nutrient intake. Int J Epidemiol 1997; 26: S161–S173.
Slimani N, Ferrari P, Ocké M, Welch A, Boeing H, Van Liere M et al. Standardization of the 24-h diet recall calibration method used in the European Prospective Investigation into Cancer and Nutrition (EPIC): general concepts and preliminary results. Eur J Clin Nutr 2000; 54: 900–917.
Slimani N, Kaaks R, Ferrari P, Casagrande C, Clavel-Chapelon F, Lotze G et al. European Prospective Investigation into Cancer and Nutrition (EPIC) calibration study: rationale, design and population characteristics. Public Health Nutr 2002; 5: 1125–1145.
Slimani N, Deharveng G, Unwin I, Southgate DAT, Vignat J, Skeie G et al. The EPIC nutrient database project (ENDB): A first attempt to standardize nutrient databases across the 10 European countries participating in the EPIC study. Eur J Clin Nutr 2007; 61: 1037–1056.
Ferrari P, Day NE, Boshuizen HC, Roddam A, Hoffmann K, Thiebaut A et al. The evaluation of the diet/disease relation in the EPIC study: considerations for the calibration and the disease models. Int J Epidemiol 2008; 37: 368–378.
Bazzano LA, He J, Ogden LG, Loria CM, Whelton PK . Dietary fiber intake and reduced risk of coronary heart disease in US men and women: The National Health and Nutrition Examination Survey I Epidemiologic Follow-up Study. Arch Intern Med 2003; 163: 1897–1904.
Burr ML, Fehily AM, Gilbert JF, Rogers S, Holliday RM, Sweetnam PM et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet 1989; 2: 757–761.
Ness AR, Hughes J, Elwood PC, Whitley E, Smith GD, Burr ML . The long-term effect of dietary advice in men with coronary disease: follow-up of the diet and reinfarction trial (DART). Eur J Clin Nutr 2002; 56: 512–518.
Howard BV, Van Horn L, Hsia J, Manson JE, Stefanick ML, Wassertheil-Smoller S et al. Low-fat dietary pattern and risk of cardiovascular disease: The Women's Health Initiative randomized controlled dietary modification trial. JAMA 2006; 295: 655–666.
Streppel MT, Arends LR, Van't Veer P, Grobbee DE, Geleijnse JM . Dietary fiber and blood pressure: A meta-analysis of randomized placebo-controlled trials. Arch Intern Med 2005; 165: 150–156.
Whelton SP, Hyre AD, Pedersen B, Yi Y, Whelton PK, He J . Effect of dietary fiber intake on blood pressure: a meta-analysis of randomized, controlled clinical trials. J Hypertens 2005; 23: 475–481.
Andersson A, Tengblad S, Karlström B, Kamal-Eldin A, Landberg R, Basu S et al. Whole-grain foods do not affect insulin sensitivity or markers of lipid peroxidation and inflammation in healthy, moderately overweight subjects. J Nutr 2007; 137: 1401–1407.
Olendzki BC, Ma Y, Schneider KL, Merriam P, Culver AL, Ockene IS et al. A simple dietary message to improve dietary quality: Results from a pilot investigation. Nutrition 2009; 25: 736–744.
Thompson WG, Holdman NR, Janzow DJ, Slezuk JM, Morris KL, Zemel MB . Effect of energy-reduced diets high in dairy products and fiber on weight loss in obese adults. Obes Res 2005; 13: 1344–1353.
Weickert MO, Roden M, Isken F, Hoffmann D, Nowotny P, Osterhoff M et al. Effects of supplemented isoenergetic diets differing in cereal fiber and protein content on insulin sensitivity in overweight humans. Am J Clin Nutr 2011; 94: 459–471.
Acknowledgements
The coordination of EPIC is financially supported by the European Commission (DG-SANCO) and the International Agency for Research on Cancer. The national cohorts are supported by Danish Cancer Society (Denmark); Federal Ministry of Education and Research (Germany); Hellenic Health Foundation, the Stavros Niarchos Foundation and the Hellenic Ministry of Health (Greece); Italian Association for Research on Cancer (AIRC) and National Research Council (Italy); Dutch Ministry of Public Health, Welfare and Sports (VWS), Netherlands Cancer Registry (NKR), LK Research Funds, Dutch Prevention Funds, Dutch ZON (Zorg Onderzoek Nederland), World Cancer Research Fund (WCRF), Statistics Netherlands (the Netherlands); Health Research Fund (FIS), Regional Governments of Andalucia, Asturias, Basque Country, Murcia and Navarra, RTICC (Red temática de investigación cooperativa en Cáncer) and CIBERESP (caber de salud Pública y Epidemiología); Swedish Cancer Society, Swedish Research Council, Regional Government of Skåne and Västerbotten and Swedish Heart Lung Foundation (Sweden); Cancer Research UK and the Medical Research Council (United Kingdom).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Crowe, F., Key, T., Appleby, P. et al. Dietary fibre intake and ischaemic heart disease mortality: the European Prospective Investigation into Cancer and Nutrition-Heart study. Eur J Clin Nutr 66, 950–956 (2012). https://doi.org/10.1038/ejcn.2012.51
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2012.51
Keywords
This article is cited by
-
Incremental monounsaturated to saturated fat ratio and fibre consumption is associated with a reduction in a composite score of modifiable cardiovascular risk factors: Prospective results from the Moli-sani study
European Journal of Clinical Nutrition (2022)
-
Burden and trend of ischemic heart disease and colorectal cancer attributable to a diet low in fiber in China, 1990–2017: findings from the Global Burden of Disease Study 2017
European Journal of Nutrition (2021)
-
The gastro-intestinal tract as the major site of biological action of dietary melanoidins
Amino Acids (2015)
-
Dietary intake of patients with angiographically defined coronary artery disease and that of healthy controls in Iran
European Journal of Clinical Nutrition (2014)
-
Dietary fibre and cardiovascular disease mortality in the UK Women’s Cohort Study
European Journal of Epidemiology (2013)