Abstract
Background/objectives:
Epidemiological evidence is suggestive, but inconclusive, for an association between consumption of red and processed meat and risk of stroke. We aimed to assess this association by conducting a meta-analysis of prospective cohort studies.
Subjects/methods:
We performed a literature search on PubMed database through June 2012 to indentify prospective cohort studies of red and processed meat intake in relation to risk of stroke. Reference lists of the retrieved articles were also reviewed. Both fixed-effects and random-effects model were assumed to compute the summary risk estimates.
Results:
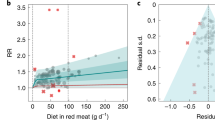
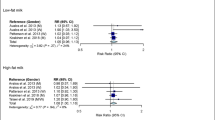
Five large independent prospective cohort studies were identified. These studies contained a total of 2 39 251 subjects and 9593 stroke events. Comparing the highest category of consumption with lowest category, the pooled relative risks (RRs) of total stroke were 1.15 (95% confidence interval (CI), 1.05–1.25) for total meat (red and processed meat combined) (n=4), 1.09 (95% CI, 1.01–1.18) for red meat (n=5) and 1.14 (95% CI, 1.05–1.25) for processed meat (n=5); the corresponding RRs of ischemic stroke (highest vs lowest quintile) were 1.15 (95% CI, 1.04–1.28), 1.13(95% CI, 1.01–1.25) and 1.19 (95% CI, 1.08–1.31). Consumption of red and/or processed meat was not associated with hemorrhagic stroke. In the dose–response analysis, the risk of stroke increased significantly by 10% and 13% for each 100 g per day increment in total and red meat consumption, respectively, and by 11% for each 50 g per day increment in processed meat consumption.
Conclusion:
Findings from this meta-analysis indicate that consumption of red and/or processed meat increase risk of stroke, in particular, ischemic stroke.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Murray CJ, Lopez AD . Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet 1997; 349: 1269–1276.
Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G et al. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation 2010; 121: e46–e215.
Di Carlo A . Human and economic burden of stroke. Age Ageing 2009; 38: 4–5.
Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Stampfer MJ et al. Red meat consumption and mortality: results from 2 prospective cohort studies. Arch Intern Med 2012; 172: 555–563.
Sinha R, Cross AJ, Graubard BI, Leitzmann MF, Schatzkin A . Meat intake and mortality: a prospective study of over half a million people. Arch Intern Med 2009; 169: 562–571.
Micha R, Wallace SK, Mozaffarian D . Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation 2010; 121: 2271–2283.
Bernstein AM, Pan A, Rexrode KM, Stampfer M, Hu FB, Mozaffarian D et al. Dietary protein sources and the risk of stroke in men and women. Stroke 2012; 43: 637–644.
Larsson SC, Virtamo J, Wolk A . Red meat consumption and risk of stroke in Swedish men. Am J Clin Nutr 2011; 94: 417–421.
Larsson SC, Virtamo J, Wolk A . Red meat consumption and risk of stroke in Swedish women. Stroke 2011; 42: 324–329.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000; 283: 2008–2012.
DerSimonian R, Laird N . Meta-analysis in clinical trials. Control Clin Trials 1986; 7: 177–188.
Greenland S, Longnecker MP . Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 1992; 135: 1301–1309.
Higgins JP, Thompson SG . Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21: 1539–1558.
Egger M, Davey Smith G, Schneider M, Minder C . Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315: 629–634.
Begg CB, Mazumdar M . Operating characteristics of a rank correlation test for publication bias. Biometrics 1994; 50: 1088–1101.
Kinjo Y, Beral V, Akiba S, Key T, Mizuno S, Appleby P et al. Possible protective effect of milk, meat and fish for cerebrovascular disease mortality in Japan. J Epidemiol 1999; 9: 268–274.
Qiu D, Mei J, Tanihata T, Kawaminami K, Minowa M . A cohort study on cerebrovascular disease in middle-aged and elderly population in rural areas in Jiangxi Province, China. J Epidemiol 2003; 13: 149–156.
Nagao M, Iso H, Yamagishi K, Date C, Tamakoshi A . Meat consumption in relation to mortality from cardiovascular disease among Japanese men and women. Eur J Clin Nutr 2012; 66: 687–693.
Fung TT, Stampfer MJ, Manson JE, Rexrode KM, Willett WC, Hu FB . Prospective study of major dietary patterns and stroke risk in women. Stroke 2004; 35: 2014–2019.
He K, Merchant A, Rimm EB, Rosner BA, Stampfer MJ, Willett WC et al. Dietary fat intake and risk of stroke in male US healthcare professionals: 14 year prospective cohort study. BMJ 2003; 327: 777–782.
Sauvaget C, Nagano J, Allen N, Grant EJ, Beral V . Intake of animal products and stroke mortality in the Hiroshima/Nagasaki Life Span Study. Int J Epidemiol 2003; 32: 536–543.
Zhang WJ, Wei H, Frei B . The iron chelator, desferrioxamine, reduces inflammation and atherosclerotic lesion development in experimental mice. Exp Biol Med (Maywood) 2010; 235: 633–641.
Kiechl S, Willeit J, Egger G, Poewe W, Oberhollenzer F . Body iron stores and the risk of carotid atherosclerosis: prospective results from the Bruneck study. Circulation 1997; 96: 3300–3307.
Jiang R, Manson JE, Meigs JB, Ma J, Rifai N, Hu FB . Body iron stores in relation to risk of type 2 diabetes in apparently healthy women. JAMA 2004; 291: 711–717.
Ascherio A, Willett WC, Rimm EB, Giovannucci EL, Stampfer MJ . Dietary iron intake and risk of coronary disease among men. Circulation 1994; 89: 969–974.
Steffen LM, Kroenke CH, Yu X, Pereira MA, Slattery ML, Van Horn L et al. Associations of plant food, dairy product, and meat intakes with 15-y incidence of elevated blood pressure in young black and white adults: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Am J Clin Nutr 2005; 82: 1169–1177. quiz 1363-1364.
Wang L, Manson JE, Buring JE, Sesso HD . Meat intake and the risk of hypertension in middle-aged and older women. J Hypertens 2008; 26: 215–222.
Kokubo Y, Kamide K, Okamura T, Watanabe M, Higashiyama A, Kawanishi K et al. Impact of high-normal blood pressure on the risk of cardiovascular disease in a Japanese urban cohort: the Suita study. Hypertension 2008; 52: 652–659.
Kanbay M, Chen Y, Solak Y, Sanders PW . Mechanisms and consequences of salt sensitivity and dietary salt intake. Curr Opin Nephrol Hypertens 2011; 20: 37–43.
Strazzullo P, D'Elia L, Kandala NB, Cappuccio FP . Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ 2009; 339: b4567.
He FJ, MacGregor GA . Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst Rev 2004 CD004937.
He FJ, Nowson CA, Lucas M, MacGregor GA . Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: meta-analysis of cohort studies. J Hum Hypertens 2007; 21: 717–728.
Carter P, Gray LJ, Troughton J, Khunti K, Davies MJ . Fruit and vegetable intake and incidence of type 2 diabetes mellitus: systematic review and meta-analysis. BMJ 2010; 341: c4229.
Soerjomataram I, Oomen D, Lemmens V, Oenema A, Benetou V, Trichopoulou A et al. Increased consumption of fruit and vegetables and future cancer incidence in selected European countries. Eur J Cancer 2010; 46: 2563–2580.
Acknowledgements
This study was funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Chen, GC., Lv, DB., Pang, Z. et al. Red and processed meat consumption and risk of stroke: a meta-analysis of prospective cohort studies. Eur J Clin Nutr 67, 91–95 (2013). https://doi.org/10.1038/ejcn.2012.180
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2012.180
Keywords
This article is cited by
-
Role of diet in stroke incidence: an umbrella review of meta-analyses of prospective observational studies
BMC Medicine (2022)
-
Health effects associated with consumption of unprocessed red meat: a Burden of Proof study
Nature Medicine (2022)
-
Meat consumption and risk of 25 common conditions: outcome-wide analyses in 475,000 men and women in the UK Biobank study
BMC Medicine (2021)
-
Relationship between sensory liking for fat, sweet or salt and cardiometabolic diseases: mediating effects of diet and weight status
European Journal of Nutrition (2020)
-
Association between intake of red and processed meat and the risk of heart failure: a meta-analysis
BMC Public Health (2019)