Abstract
Background:
The anthropometric measurement of mid-arm muscular area (MAMA) involves overestimation because of various assumptions, this overestimation being progressive with increasing adiposity. However, the effects of muscle atrophy and variation of the subcutaneous fat thickness have remained uncertain.
Objectives:
The validity of MAMA estimated by anthropometry was examined by comparing with MAMA measured by computed tomography (CT) in a nonobese population. The effects of muscle atrophy and variation of the subcutaneous fat thickness on the validity of MAMA were examined by new indices.
Subjects/Methods:
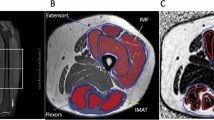
The relative MAMA was compared between the anthropometric and CT methods in 45 patients. New indices were introduced for assessing muscle deformity (muscle deformity index, MDI) and subcutaneous fat variation (SFVI). The effects of MDI, SFVI and age on the difference of MAMA between the anthropometric and CT methods were investigated.
Results:
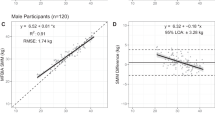
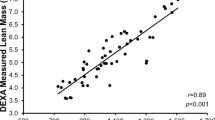
MDIs were positively correlated with age in males (r=0.47, P<0.05) and females (r=0.66, P<0.001). SFVI was positively correlated with age only in females (r=0.54, P<0.01). Even in these patients, the relative MAMA estimated by anthropometry was significantly associated with that measured by CT (r=0.85, P<0.0001 in males and r=0.90, P<0.0001 in females). A Bland–Altman plot indicated that the difference between both methods was relatively small, although increased adiposity might be a source of overestimation for anthropometric MAMA measurement.
Conclusions:
MAMA estimated by anthropometry was a reliable indicator of muscle mass in patients with muscle atrophy and varying thickness of subcutaneous fat in lean patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Baumgartner RN, Rhyne RL, Troup C, Wayne S, Garry PJ (1992). Appendicular skeletal muscle areas assessed by magnetic resonance imaging in older persons. J Gerontol 47, M67–M72.
Burr ML, Phillips KM (1984). Anthropometric norms in the elderly. Br J Nutr 51, 165–169.
Eng CM, Abrams GD, Smallwood LR, Lieber RL, Ward SR (2007). Muscle geometry affects accuracy of forearm volume determination by magnetic resonance imaging (MRI). J Biomech 40, 3261–3266.
Eveleth PB, Andres R, Chumlea WC, Eiben O, Ge K, Harris T et al. (1998). Uses and interpretation of anthropometry in the elderly for the assessment of physical status. Report to the Nutrition Unit of the World Health Organization: Expert Subcommittee on the Use and Interpretation of Anthropometry in the Elderly. J Nutr Health Aging 2, 5–17.
Forbes GB, Brown MR, Griffiths HJ (1988). Arm muscle plus bone area: anthropometry and CAT scan compared. Am J Clin Nutr 47, 929–931.
Friedman PJ, Campbell AJ, Caradoc-Davies TH (1985). Prospective trial of a new diagnostic criterion for severe wasting malnutrition in the elderly. Age Ageing 14, 149–154.
Frisancho AR (1990). Anthropometric Standards for the Assessment of Growth and Nutritional Status. University of Michigan Press: Ann Arbor.
Heymsfield SB, Gallagher D, Visser M, Nuñez C, Wang ZM (1995). Measurement of skeletal muscle: laboratory and epidemiological methods. J Gerontol A Biol Sci Med Sci 50A, 23–29.
Heymsfield SB, McManus C, Smith J, Stevens V, Nixon DW (1982). Anthropometric measurement of muscle mass: revised equations for calculating bone-free arm muscle area. Am J Clin Nutr 36, 680–690.
Heymsfield SB, Olafson RP, Kutner MH, Nixon DW (1979). A radiographic method of quantifying protein-calorie undernutrition. Am J Clin Nutr 32, 693–702.
Jackiw R (1972). Introducing scale symmetry. Physics Today 25, 23–27.
Japanese Anthropometric Reference Data: JARD 2001 (2002). Jpn J Nutr Assess 19 (suppl). (in Japanese).
Lee SY, Gallagher D (2008). Assessment methods in human body composition. Curr Opin Clin Nutr Metab Care 11, 566–572.
Papathakis PC, Rollins NC, Brown KH, Bennish ML, Van Loan MD (2005). Comparison of isotope dilution with bioimpedance spectroscopy and anthropometry for assessment of body composition in asymptomatic HIV-infected and HIV-uninfected breastfeeding mothers. Am J Clin Nutr 82, 538–546.
Acknowledgements
This study was supported by a grant from the COE (Center of Excellence) Program in the 21st Century at the University of Shizuoka.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix A
Appendix A
MDI defined by a simple model calculation
The progression of muscle deformity can be regarded by a simple approximation from a circle to an ellipse. In this simple geometrical model, a candidate for the deformity index is

where a is the shorter radius and b is the longer radius of the ellipsec.
Parameter r, however, is rather difficult to calculate because the center of the irregularly shaped arm muscle cannot be easily found. We thus introduce MDI in this study as

where MAMC is the mid-arm muscular circumference and MAMA is the mid-arm muscular area.
The validity of this equation can be easily demonstrated. In equations (1) and (2), the quantities of both r and MDI should be independent of the scaling of the body size, so a scale transformation or Weyl transformation (Jackiw, 1972) is performed.



where ew is the scale factor (a positive number; w=0 is the identical transformation).
MDI is expressed as,



where L (a, b) is the circumference of an ellipse, E (k2) is the complete elliptical integral of the second kind and S (a, b) is the area of an ellipse. MDI depends only on scale invariant parameter r=b/a, hence manifesting their scale invariance.
MDI shows a positive association with r in the range of 1⩽r⩽5.
Rights and permissions
About this article
Cite this article
Saito, R., Ohkawa, S., Ichinose, S. et al. Validity of mid-arm muscular area measured by anthropometry in nonobese patients with increased muscle atrophy and variation of subcutaneous fat thickness. Eur J Clin Nutr 64, 899–904 (2010). https://doi.org/10.1038/ejcn.2010.87
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2010.87
Keywords
This article is cited by
-
The feasibility and acceptability of a home-based, virtual exercise intervention for older patients with hepatocellular carcinoma: protocol for a non-randomised feasibility study (TELEX-Liver Cancer)
Pilot and Feasibility Studies (2022)
-
How reliably can ultrasound help determine muscle and adipose tissue thickness in clinical settings? An assessment of intra- and inter-examiner reliability in the USVALID study
European Journal of Clinical Nutrition (2022)
-
Utility of the simplified measurements of muscle mass in patients with gastrointestinal and chronic liver diseases
Scientific Reports (2020)
-
Mid-arm muscle area and anthropometry predict low birth weight and poor pregnancy outcomes in Tanzanian women with HIV
BMC Pregnancy and Childbirth (2018)