Abstract
Objective:
To compare childhood obesity prevalence in England and the United States using different criteria.
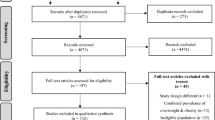
Subjects/Methods:
Participants included 2- to 17-year olds in the Health Survey for England (HSE, n=33 563) and the US National Health and Nutrition Examination Survey (NHANES, n=14 540) 1999 through 2006. Mean body mass index (BMI) and prevalence of obesity were compared using the UK 1990, US 2000 Centers for Disease Control and International Obesity Task Force (IOTF) criteria.
Results:
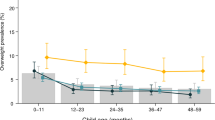
English children at ages 2–5 years had a higher mean BMI than US children (mean difference (English minus US)=0.41 kg/m2, 95% confidence intervals (CI) 0.31–0.52). At age ⩾8 years, mean BMI was lower in England (for ages 8–11 years, mean difference=−1.00 kg/m2, 95% CI −1.26 to −0.75; for ages 12–17 years, mean difference=−1.37 kg/m2, 95% CI −1.59 to −1.14). The IOTF criteria produced the lowest estimates of obesity prevalence. The 2000 Centre for Disease Control and Prevention (CDC) criteria produced the highest estimates in younger children and the UK 1990 criteria produced the highest in adolescents. Children aged 2–5 years in England had higher prevalence of obesity than those in the United States when using the 2000 CDC and UK 1990 criteria. US adolescents had the highest prevalence of obesity by age group using each of the three criteria.
Conclusion:
The 2000 CDC and UK 1990 criteria give a higher prevalence of obesity in England than in the United States at ages 2–5 years; however, at age ⩾8 years, the reverse is true. Estimates of childhood obesity prevalence rely on the criteria used, which has implications for surveillance and clinical practice.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000). Establishing a standard definition for child overweight and obesity worldwide: international survey (see comment). BMJ 320, 1240–1243.
Cole TJ, Freeman JV, Preece MA (1995). Body mass index reference curves for the UK, 1990. Arch Dis Child 73, 25–29.
Euling SY, Selevan SG, Pescovitz OH, Skakkebaek NE (2008). Role of environmental factors in the timing of puberty. Pediatrics 121 (Supplement_3), S167–S171.
Kuczmarski RL, Ogden CL, Guo SS (2002). 2000 CDC Growth Charts for the United States: Methods and Development. Vital Health Stat 11(246). National Center for Health Statistics.
Must A, Dallal GE, Dietz WH (1991a). Reference data for obesity: 85th and 95th percentiles of body mass index (wg/ht2)—a correction. Am J Clin Nutr 54, 773.
Must A, Dallal GE, Dietz WH (1991b). Reference data for obesity: 85th and 95th percentiles of body mass index (wg/ht2) and triceps skinfold thickness. Am J Clin Nutr 53, 839–846.
National Center for Health Statistics (2006). Centers for Disease Control and Prevention Analytic And Reporting Guidelines. The National Health and Nutrition Examination Survey (NHANES). National Center for Health Statistics Centers for Disease Control and Prevention: Hyattsville, Maryland.
Ogden CL, Carroll MD, Flegal KM, Ogden CL, Carroll MD, Flegal KM (2008). High body mass index for age among US children and adolescents, 2003–2006 (see comment). JAMA 299, 2401–2405.
Reilly JJ, Dorosty AR, Emmett PM, The ALSPAC Study Team (2000). Identification of the obese child: adequacy of the body mass index for clinical practice and epidemiology. Int J Obes 24, 1623–1627.
Reilly JJ, Kelly J, Wilson DC (2010). Accuracy of simple clinical and epidemiological definitions of childhood obesity: systematic review and evidence appraisal. Obes Rev 11, 645–655.
Sproston K, Mindell J (2006). Health Survey for England 2004, vol. 2. Methodology and Documentation. The Information Centre: London.
Sproston K, Primatesta P (2003). Health Survey for England 2002: vol 3: Methodology and Documentation. The Stationary Office: London.
Sproston K, Primatesta P (2004). Health Survey for England 2003, vol. 3. Methodology and Documentation. The Stationery Office: London.
The Information Centre (2008). Health survey for England 2007 latest trends. http://www.ic.nhs.uk/webfiles/publications/HSE07/Health%20Survey%20for%20England%202007%20Latest%20Trends.pdf. 16-4-2009. Ref Type: Electronic Citation.
Wang Y (2004). Epidemiology of childhood obesity—methodological aspects and guidelines: what is new? Int J Obes Relat Metab Disord 28 (S3), S21–S28.
Wang Y, Lobstein T (2006). Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes 1, 11–25.
Wang Y, Wang JQ (2002). A comparison of international references for the assessment of child and adolescent overweight and obesity in different populations. Eu J Clin Nutr 56, 973–982.
Wyshak G, Frisch RE (1982). Evidence for a secular trend in age of menarche. N Engl J Med 306, 1033–1035.
Zimmermann MB, Gubeli C, Puntener C, Molinari L (2004). Detection of overweight and obesity in a national sample of 6–12-y-old Swiss children: accuracy and validity of reference values for body mass index from the US Centers for Disease Control and Prevention and the International Obesity Task Force. Am J Clin Nutr 79, 838–843.
Acknowledgements
No funding was received for the design and conduct of the study; for collection, management, analysis and interpretation of the data; and for preparation, review or approval of the manuscript. No specific funding was received for the work. IAL is funded by NIHR, the UK National Institute for Health Research, as part of PenCLAHRC, the Peninsula Collaboration for Leadership in Applied Health Research and Care. RRK is supported by the South West Public Health Training Scheme. DAL is funded by the Higher Education Funding Council for England. DAL has grants from the UK Medical Research Council, the Wellcome Trust and the British Heart Foundation, although this work was not directly funded by any of these. RJ is funded from a Career Development Fellowship supported by the National Institute for Health Research. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on European Journal of Clinical Nutrition website
Supplementary information
Rights and permissions
About this article
Cite this article
Lang, I., Kipping, R., Jago, R. et al. Variation in childhood and adolescent obesity prevalence defined by international and country-specific criteria in England and the United States. Eur J Clin Nutr 65, 143–150 (2011). https://doi.org/10.1038/ejcn.2010.260
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2010.260
Keywords
This article is cited by
-
Gender and Ethnic Differences in the Association Between Obesity and Depression Among Black Adolescents
Journal of Racial and Ethnic Health Disparities (2015)