Abstract
Background/Objectives:
High-fat (HF) diets of 2 weeks have been shown to accelerate gastric emptying (GE). To date, no studies have shown any alteration in GE following shorter HF diets. The aim of this study was to assess if an HF, high-energy diet of 3 days can adapt gastrointestinal (GI) transit, blood lipids and satiety.
Subjects/Methods:
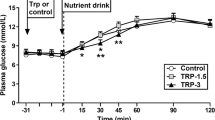
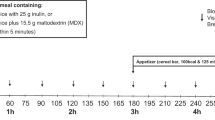
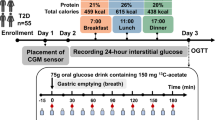
Eleven male volunteers participated in a study consisting of three, 3-day interventions each separated by a test day. During the first intervention, volunteers recorded their diet. In the second and third interventions, volunteers repeated their food diary plus either a low-fat yogurt or HF yogurt supplement in randomized order. Test days involved measurement of GE using the 13C octanoic-acid breath-test, mouth-to-caecum transit time (MCTT) using the inulin H2 breath test and satiety using visual analogue scales. Blood samples for measurement of lipaemia were taken using a venous cannula.
Results:
MCTT was different between the three test days (P=0.038), with the shortest MCTT following the HF intervention. GE was shortest following the HF intervention. There were no differences in satiety between the interventions. The HF intervention reduced triglycerides, total cholesterol and low-density lipoprotein cholesterol, and increased high-density lipoprotein cholesterol.
Conclusion:
This study shows that changes in GI transit owing to an HF diet can occur in a time period as short as 3 days.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Bond Jr JH, Levitt MD, Prentiss R (1975). Investigation of small bowel transit time in man utilizing pulmonary hydrogen (H2) measurements. J Lab Clin Med 85, 546–555.
Boyd KA, O’Donovan DG, Doran S, Wishart J, Chapman IM, Horowitz M et al. (2003). High-fat diet effects on gut motility, hormone, and appetite responses to duodenal lipid in healthy men. Am J Physiol Gastrointest Liver Physiol 284, G188–G196.
Brown NJ, Rumsey RD, Read NW (1994). Gastrointestinal adaptation to enhanced small intestinal lipid exposure. Gut 35, 1409–1412.
Burns RN, Moniri NH (2010). Agonism with the omega-3 fatty acids alpha-linolenic acid and docosahexaenoic acid mediates phosphorylation of both the short and long isoforms of the human GPR120 receptor. Biochem Biophys Res Commun 396, 1030–1035.
Cardoso-Junior A, Coelho LG, Savassi-Rocha PR, Vignolo MC, Abrantes MM, de Almeida AM et al. (2007). Gastric emptying of solids and semi-solids in morbidly obese and non-obese subjects: an assessment using the 13C-octanoic acid and 13C-acetic acid breath tests. Obes Surg 17, 236–241.
Castiglione KE, Read NW, French SJ (2002). Adaptation to high-fat diet accelerates emptying of fat but not carbohydrate test meals in humans. Am J Physiol Regul Integr Comp Physiol 282, R366–R371.
Cecil JE, Francis J, Read NW (1999). Comparison of the effects of a high-fat and high-carbohydrate soup delivered orally and intragastrically on gastric emptying, appetite, and eating behaviour. Physiol Behav 67, 299–306.
Clegg M, McClean C, Davison GW, Murphy MH, Trinick T, Duly E et al. (2007). Exercise and postprandial lipaemia: effects on peripheral vascular function, oxidative stress and gastrointestinal transit. Lipids Health Dis 6, 30.
Clegg M, Shafat A (2009). Conference on “Multidisciplinary approaches to nutritional problems” Postgraduate Symposium. The role of fat in gastric emptying and satiety: acute and chronic effects. Proc Nutr Soc 68, 89–97.
Clegg M, Shafat A (2010a). Energy and macronutrient composition of breakfast affect gastric emptying of lunch and subsequent food intake, satiety and satiation. Appetite 54, 517–523.
Clegg M, Shafat A (2010b). Gastric emptying and orocaecal transit time of meals containing lactulose or inulin in men. Br J Nutr 104, 554–559.
Cummins DG, Marion JE, Craigmiles JP, Burns RE (1967). Oil content, fatty acid composition, and other agronomic characteristics of sunflower introductions. J Am Oil Chem Soc 44, 581–582.
Cunningham KM, Daly J, Horowitz M, Read NW (1991). Gastrointestinal adaptation to diets of differing fat composition in human volunteers. Gut 32, 483–486.
Darwiche G, Ostman EM, Liljeberg HG, Kallinen N, Bjorgell O, Bjorck IM et al. (2001). Measurements of the gastric emptying rate by use of ultrasonography: studies in humans using bread with added sodium propionate. Am J Clin Nutr 74, 254–258.
Engelstoft MS, Egerod KL, Holst B, Schwartz TW (2008). A gut feeling for obesity: 7TM sensors on enteroendocrine cells. Cell Metab 8, 447–449.
French SJ, Murray B, Rumsey RD, Fadzlin R, Read NW (1995). Adaptation to high-fat diets: effects on eating behaviour and plasma cholecystokinin. Br J Nutr 73, 179–189.
Friedewald WT, Levy RI, Fredrickson DS (1972). Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18, 499–502.
Geboes KP, Luypaerts A, Rutgeerts P, Verbeke K (2003). Inulin is an ideal substrate for a hydrogen breath test to measure the orocaecal transit time. Aliment Pharmacol Ther 18, 721–729.
Geliebter A (1988). Gastric distension and gastric capacity in relation to food intake in humans. Physiol Behav 44, 665–668.
Ghoos YF, Maes BD, Geypens BJ, Mys G, Hiele MI, Rutgeerts PJ et al. (1993). Measurement of gastric emptying rate of solids by means of a carbon-labeled octanoic acid breath test. Gastroenterology 104, 1640–1647.
Harris WS (2008). Linoleic acid and coronary heart disease. Prostaglandins Leukot Essent Fatty Acids 79, 169–171.
Haycock GB, Schwartz GJ, Wisotsky DH (1978). Geometric method for measuring body surface area: a height–weight formula validated in infants, children, and adults. J Pediatr 93, 62–66.
Hill JO, Peters JC (1998). Environmental contributions to the obesity epidemic. Science 280, 1371–1374.
James WP (2008). The epidemiology of obesity: the size of the problem. J Intern Med 263, 336–352.
Liddle RA, Rushakoff RJ, Morita ET, Beccaria L, Carter JD, Goldfine ID (1988). Physiological role for cholecystokinin in reducing postprandial hyperglycemia in humans. J Clin Invest 81, 1675–1681.
Little TJ, Horowitz M, Feinle-Bisset C (2007). Modulation by high-fat diets of gastrointestinal function and hormones associated with the regulation of energy intake: implications for the pathophysiology of obesity. Am J Clin Nutr 86, 531–541.
Maljaars J, Romeyn EA, Haddeman E, Peters HP, Masclee AA (2009). Effect of fat saturation on satiety, hormone release, and food intake. Am J Clin Nutr 89, 1019–1024.
Maljaars PW, Peters HP, Mela DJ, Masclee AA (2008). Ileal brake: a sensible food target for appetite control. A review. Physiol Behav 95, 271–281.
Mensink RP, Zock PL, Kester AD, Katan MB (2003). Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr 77, 1146–1155.
Moore K, Zhang Q, Murgolo N, Hosted T, Duffy R (2009). Cloning, expression, and pharmacological characterization of the GPR120 free fatty acid receptor from cynomolgus monkey: comparison with human GPR120 splice variants. Comp Biochem Physiol B 154, 419–426.
Niness KR (1999). Inulin and oligofructose: what are they? J Nutr 129, 1402S–1406S.
Park MI, Camilleri M, O’Connor H, Oenning L, Burton D, Stephens D et al. (2007). Effect of different macronutrients in excess on gastric sensory and motor functions and appetite in normal-weight, overweight, and obese humans. Am J Clin Nutr 85, 411–418.
Ridker PM (2008). Fasting versus nonfasting triglycerides and the prediction of cardiovascular risk: do we need to revisit the oral triglyceride tolerance test? Clin Chem 54, 11–13.
Robertson MD, Jackson KG, Fielding BA, Morgan LM, Williams CM, Frayn KN (2002). Acute ingestion of a meal rich in n-3 polyunsaturated fatty acids results in rapid gastric emptying in humans. Am J Clin Nutr 76, 232–238.
Rolls BJ (2000). The role of energy density in the overconsumption of fat. J Nutr 130, 268S–271S.
Schommartz B, Ziegler D, Schadewaldt P (1998). Significance of diagnostic parameters in [13C]octanoic acid gastric emptying breath tests. Isotopes Environ Health Stud 34, 135–143.
Shahidullah M, Kennedy TL, Parks TG (1975). The vagus, the duodenal brake, and gastric emptying. Gut 16, 331–336.
Tanaka T, Katsuma S, Adachi T, Koshimizu TA, Hirasawa A, Tsujimoto G (2008). Free fatty acids induce cholecystokinin secretion through GPR120. Naunyn Schmiedebergs Arch Pharmacol 377, 523–527.
Temelkova-Kurktschiev TS, Koehler C, Henkel E, Leonhardt W, Fuecker K, Hanefeld M (2000). Postchallenge plasma glucose and glycemic spikes are more strongly associated with atherosclerosis than fasting glucose or HbA1c level. Diabetes Care 23, 1830–1834.
Acknowledgements
We gratefully acknowledge the Irish Research Council for Science, Engineering and Technology (IRCSET) for their support of this project. Inulin was donated by Orafti, Belgium.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Clegg, M., McKenna, P., McClean, C. et al. Gastrointestinal transit, post-prandial lipaemia and satiety following 3 days high-fat diet in men. Eur J Clin Nutr 65, 240–246 (2011). https://doi.org/10.1038/ejcn.2010.235
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2010.235
Keywords
This article is cited by
-
Prevalence, overlap, and risk factors for Rome IV functional gastrointestinal disorders among college students in northern India
Indian Journal of Gastroenterology (2021)
-
Short-term low carbohydrate/high-fat diet intake increases postprandial plasma glucose and glucagon-like peptide-1 levels during an oral glucose tolerance test in healthy men
European Journal of Clinical Nutrition (2012)
-
Does domperidone, a D2-antagonist alter gastric emptying rates and appetite sensations in healthy adults with high-fat meal? A block-randomised, single-blind placebo-controlled study
Irish Journal of Medical Science (2012)
-
Effect of cinnamon on gastric emptying, arterial stiffness, postprandial lipemia, glycemia, and appetite responses to high-fat breakfast
Cardiovascular Diabetology (2011)