Abstract
Background/Objectives:
There is convincing evidence that a high dietary fiber intake may lower the risk of coronary heart disease. However, the role of fiber in the prevention of stroke is unclear. We examined the associations of dietary fiber and fiber-rich food intake with risk of stroke within the Alpha-tocopherol, Beta-carotene Cancer Prevention Study.
Subjects/Methods:
Between 1985 and 1988, 26 556 Finnish male smokers aged 50–69 years, who had no history of stroke, completed a dietary questionnaire. During a mean follow-up of 13.6 years, 2702 cerebral infarctions, 383 intracerebral hemorrhages and 196 subarachnoid hemorrhages were ascertained.
Results:
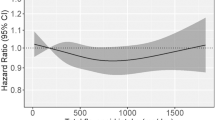
After adjustment for cardiovascular risk factors and folate and magnesium intakes, there was no significant association between intake of total fiber, water-soluble fiber, water-insoluble fiber, or fiber derived from fruit or cereal sources and risk of any stroke subtype. Vegetable fiber intake, as well as the consumption of fruit, vegetables and cereals, was inversely associated with the risk of cerebral infarction; the multivariate relative risks for the highest quintile of intake as compared with the lowest were 0.86 (95% confidence interval (CI): 0.76–0.99) for vegetable fiber, 0.82 (95% CI: 0.73–0.93) for fruit, 0.75 (95% CI: 0.66–0.85) for vegetables and 0.87 (95% CI: 0.74–1.03) for cereals. Vegetable consumption was inversely associated with risk of subarachnoid hemorrhage (relative risk for highest versus lowest quintile: 0.62; 95% CI: 0.40–0.98), and cereal consumption was inversely associated with risk of intracerebral hemorrhage (relative risk: 0.64; 95% CI: 0.41–1.01).
Conclusions:
These findings suggest a beneficial effect of the consumption of fruits, vegetables and cereals on stroke risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM et al. (1997). A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 336, 1117–1124.
Ascherio A, Rimm EB, Hernan MA, Giovannucci EL, Kawachi I, Stampfer MJ et al. (1998). Intake of potassium, magnesium, calcium, and fiber and risk of stroke among US men. Circulation 98, 1198–1204.
ATBC Cancer Prevention Study Group (1994). The alpha-tocopherol, beta-carotene lung cancer prevention study: design, methods, participant characteristics, and compliance. Ann Epidemiol 4, 1–10.
Brown L, Rosner B, Willett WW, Sacks FM (1999). Cholesterol-lowering effects of dietary fiber: a meta-analysis. Am J Clin Nutr 69, 30–42.
Chandalia M, Garg A, Lutjohann D, von Bergmann K, Grundy SM, Brinkley LJ (2000). Beneficial effects of high dietary fiber intake in patients with type 2 diabetes mellitus. N Engl J Med 342, 1392–1398.
Cox DR (1972). Regression models and life tables (with discussion). J R Stat Soc (B) 34, 187–220.
Hallfrisch J, Scholfield DJ, Behall KM (1995). Diets containing soluble oat extracts improve glucose and insulin responses of moderately hypercholesterolemic men and women. Am J Clin Nutr 61, 379–384.
He FJ, Nowson CA, MacGregor GA (2006). Fruit and vegetable consumption and stroke. Meta-analysis of cohort studies. Lancet 367, 320–326.
Heart Protection Study Collaborative Group (2002a). MRC/BHF Heart Protection Study of antioxidant vitamin supplementation in 20 536 high-risk individuals: a randomised placebo-controlled trial. Lancet 360, 23–33.
Hirvonen T, Virtamo J, Korhonen P, Albanes D, Pietinen P (2000). Intake of flavonoids, carotenoids, vitamins C and E, and risk of stroke in male smokers. Stroke 31, 2301–2306.
Homocysteine Studies Collaboration (2002b). Homocysteine and risk of ischemic heart disease and stroke: a meta-analysis. JAMA 288, 2015–2022.
King DE, Egan BM, Woolson RF, Mainous III AG, Al-Solaiman Y, Jesri A (2007). Effect of high-fiber diet vs a fiber-supplemented diet on C-reactive protein level. Arch Intern Med 167, 502–506.
Krupski WC (1991). The peripheral vascular consequences of smoking. Ann Vasc Surg 5, 291–304.
Larsson SC, Männistö S, Virtanen MJ, Kontto J, Albanes D, Virtamo J (2008a). Folate, vitamin B6, vitamin B12, and methionine intakes and risk of stroke subtypes in male smokers. Am J Epidemiol 167, 954–961.
Larsson SC, Virtanen MJ, Mars M, Männistö S, Pietinen P, Albanes D et al. (2008b). Magnesium, calcium, potassium, and sodium intakes and risk of stroke in male smokers. Arch Intern Med 168, 459–465.
Leppälä JM, Virtamo J, Fogelholm R, Albanes D, Taylor PR, Heinonen OP (2000). Vitamin E and beta carotene supplementation in high risk for stroke. a subgroup analysis of the alpha-tocopherol, beta-carotene cancer prevention study. Arch Neurol 57, 1503–1509.
Leppälä JM, Virtamo J, Heinonen OP (1999). Validation of stroke diagnosis in the National Hospital Discharge Register and the Register of Causes of Death in Finland. Eur J Epidemiol 15, 155–160.
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R (2002). Age-specific relevance of usual blood pressure to vascular mortality. a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360, 1903–1913.
Mozaffarian D, Kumanyika SK, Lemaitre RN, Olson JL, Burke GL, Siscovick DS (2003). Cereal, fruit, and vegetable fiber intake and the risk of cardiovascular disease in elderly individuals. JAMA 289, 1659–1666.
Oh K, Hu FB, Cho E, Rexrode KM, Stampfer MJ, Manson JE et al. (2005). Carbohydrate intake, glycemic index, glycemic load, and dietary fiber in relation to risk of stroke in women. Am J Epidemiol 161, 161–169.
Omvik P (1996). How smoking affects blood pressure. Blood Press 5, 71–77.
Pereira MA, O'Reilly E, Augustsson K, Fraser GE, Goldbourt U, Heitmann BL et al. (2004). Dietary fiber and risk of coronary heart disease. a pooled analysis of cohort studies. Arch Intern Med 164, 370–376.
Pietinen P, Hartman AM, Haapa E, Räsänen L, Haapakoski J, Palmgren J et al. (1988). Reproducibility and validity of dietary assessment instruments. I. A self-administered food use questionnaire with a portion size picture booklet. Am J Epidemiol 128, 655–666.
Pietinen P, Rimm EB, Korhonen P, Hartman AM, Willett WC, Albanes D et al. (1996). Intake of dietary fiber and risk of coronary heart disease in a cohort of Finnish men. The alpha-tocopherol, beta-carotene cancer prevention study. Circulation 94, 2720–2727.
Selhub J (1999). Homocysteine metabolism. Annu Rev Nutr 19, 217–246.
Slavin JL, Martini MC, Jacobs Jr DR, Marquart L (1999). Plausible mechanisms for the protectiveness of whole grains. Am J Clin Nutr 70, 459S–463S.
Varo P, Laine R, Veijalainen K, Espo A, Wetterhoff A, Koivistoinen P (1984a). Dietary fiber and available carbohydrates in Finnish vegetables and fruits. J Agric Sci Finl 56, 49–59.
Varo P, Laine R, Veijalainen K, Pero K, Koivistoinen P (1984b). Dietary fiber and available carbohydrates in Finnish cereal products. J Agric Sci Finl 56, 39–48.
Walker AE, Robins M, Weinfeld FD (1981). The National Survey of Stroke. Clinical findings. Stroke 12, I13–I44.
Weickert MO, Mohlig M, Schofl C, Arafat AM, Otto B, Viehoff H et al. (2006). Cereal fiber improves whole-body insulin sensitivity in overweight and obese women. Diabetes Care 29, 775–780.
Whelton SP, Hyre AD, Pedersen B, Yi Y, Whelton PK, He J (2005). Effect of dietary fiber intake on blood pressure. a meta-analysis of randomized, controlled clinical trials. J Hypertens 23, 475–481.
Willett W, Stampfer MJ (1986). Total energy intake. implications for epidemiologic analyses. Am J Epidemiol 124, 17–27.
Acknowledgements
This ATBC Study was supported by Public Health Service contracts N01-CN-45165, N01-RC-45035 and N01-RC-37004 from the US National Cancer Institute, National Institutes of Health, Department of Health and Human Services, Bethesda, MD. Dr Larsson's postdoctoral research at the National Public Health Institute in Helsinki, Finland, was supported by a grant from the Swedish Council for Working Life and Social Research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Larsson, S., Männistö, S., Virtanen, M. et al. Dietary fiber and fiber-rich food intake in relation to risk of stroke in male smokers. Eur J Clin Nutr 63, 1016–1024 (2009). https://doi.org/10.1038/ejcn.2009.16
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2009.16
Keywords
This article is cited by
-
Health effects associated with vegetable consumption: a Burden of Proof study
Nature Medicine (2022)
-
Dietary fibre intake and risk of ischaemic and haemorrhagic stroke in the UK Women’s Cohort Study
European Journal of Clinical Nutrition (2015)
-
Dietary Fiber Intake and Risk of Stroke
Current Nutrition Reports (2014)
-
Dietary fiber intake and stroke risk: a meta-analysis of prospective cohort studies
European Journal of Clinical Nutrition (2013)
-
Impact of nutritional status and dietary quality on stroke: do we need specific recommendations?
European Journal of Clinical Nutrition (2013)