Abstract
Background/Objectives:
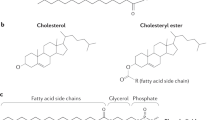
The fatty acid pattern of membrane phospholipids is suggested to affect membrane fluidity and epithelial barrier function as a result of membrane fatty acid unsaturation. The incorporation of n-3 polyunsaturated fatty acids (PUFAs) into membrane phospholipids may diminish inflammatory potential in patients with gastrointestinal diseases. The aim of this study was to improve the fatty acid profile of erythrocyte membrane phospholipids after oral supplementation of specific fatty acids in patients with maldigestion and/or malabsorption.
Subjects/Methods:
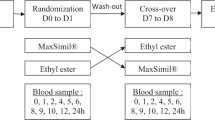
We conducted a randomized, double-blind, controlled trial. A total of 48 patients with gastrointestinal diseases received either fat-soluble vitamins A,D,E,K (ADEK) or ADEK plus fatty acids α-linolenic acid (ALA), docosahexaenoic acid (DHA) and medium-chain triglycerides (FA-ADEK) for 12 weeks. The fatty acid profile of erythrocyte membrane phospholipids, dietary intake, plasma antioxidant vitamins and serum γ-glutamyl transferase (GGT) were evaluated at baseline, 8 and 12 weeks after supplementation.
Results:
Supplementation with FA-ADEK increased ALA, DHA and eicosapentaenoic acid (EPA) concentrations of erythrocyte membrane phospholipids by 0.040, 1.419 and 0.159%, respectively, compared with ADEK supplementation (−0.007, 0.151 and 0.002%, respectively) after 12 weeks (all P⩽0.001). Serum GGT activity decreased in patients receiving FA-ADEK compared with those receiving ADEK with a significant difference after 8 weeks.
Conclusions:
The significant change in erythrocyte membrane fatty acid pattern demonstrates the incorporation of orally administered n-3 PUFA in patients with maldigestion and malabsorption. The increase in ALA and DHA, as well as the conversion of ALA to EPA is attributed to the supplementation of sufficient amounts of ALA and DHA, respectively. Serum GGT activity decreased in response to decreased oxidative stress.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
André P, Balkau B, Born C, Charles MA, Eschwège E, D.E.S.I.R. study group (2006). Three-year increase of gamma-glutamyltransferase level and development of type 2 diabetes in middle-aged men and women: the D.E.S.I.R. cohort. Diabetologia 49, 2599–2603.
Barceló-Coblijn G, Murphy EJ, Othman R, Moghadasian MH, Kashour T, Friel JK (2008). Flaxseed oil and fish-oil capsule consumption alters human red blood cell n-3 fatty acid composition: a multiple-dosing trial comparing 2 sources of n-3 fatty acid. Am J Clin Nutr 88, 801–809.
Belluzzi A, Brignola C, Campieri M, Pera A, Boschi S, Miglioli M (1996). Effect of an enteric-coated fish-oil preparation on relapses in Crohn's disease. N Engl J Med 334, 1557–1560.
Biesalski HK, Böhles H, Esterbauer H, Fürst P, Gey F, Hundsdörfer G et al. (1997). Antioxidant vitamins in prevention. Clin Nutr 16, 151–155.
Calder PC (2008). Polyunsaturated fatty acids, inflammatory processes and inflammatory bowel diseases. Mol Nutr Food Res 52, 885–897.
Cao J, Schwichtenberg KA, Hanson NQ, Tsai MY (2006). Incorporation and clearance of omega-3 fatty acids in erythrocyte membranes and plasma phospholipids. Clin Chem 52, 2265–2272.
Carroccio A, Verghi F, Santini B, Lucidi V, Iacono G, Cavataio F et al. (2001). Diagnostic accuracy of fecal elastase 1 assay in patients with pancreatic maldigestion or intestinal malabsorption. Dig Dis Sci 46, 1335–1342.
Christophe A, Matthijs F (1967). New method for the determination of the fatty acid pattern of serum lipid classes. Clin Chim Acta 16, 39–43.
Das UN (2006). Essential fatty acids: biochemistry, physiology and pathology. Biotechnol J 1, 420–439.
DeMeo MT, Mutlu EA, Keshavarzian A, Tobin MC (2002). Intestinal permeation and gastrointestinal disease. J Clin Gastroenterol 34, 385–396.
De Vizia B, Raia V, Spano C, Pavlidis C, Coruzzo A, Alessio M (2003). Effect of an 8-month treatment with ω-3 fatty acids (eicosapentaenoic and docosahexaenoic) in patients with cystic fibrosis. J Parenter Enteral Nutr 27, 52–57.
D’Odorico A, Bortolan S, Cardin R, D’Inca R, Martines D, Ferronato A et al. (2001). Reduced plasma antioxidant concentrations and increased oxidative DNA damage in inflammatory bowel disease. Scand J Gastroenterol 36, 1289–1294.
Ehrhardt J (2002). Labormethoden und Normalwerte für fett- und wasserlösliche Vitamine (Laboratory methods and normal values for fat- and water-soluble vitamins). Vitamine, Spurenelemente und Mineralstoffe. Prävention und Therapie mit Mikronährstoffen (Vitamins, trace elements and minerals. Prevention and therapy with micronutrients), In: (eds). KH Biesalski, J Köhrle, K Schümann, Georg Thieme Verlag: Stuttgart, 676–682.
Emdin M, Pompella A, Paolicchi A (2005). Gamma-glutamyltransferase, atherosclerosis, and cardiovascular disease. Triggering oxidative stress within the plaque. Circulation 112, 2078–2080.
Folch J, Lees M, Stanley GHS (1957). A simple method for the isolation and purification of total lipids from animal tissues. J Biol Chem 226, 497–509.
Guebre-Egziabher F, Rabasa-Lhoret R, Bonnet F, Bastard JP, Desage M, Skilton MR et al. (2008). Nutritional intervention to reduce the n-6/n-3 fatty acid ratio increases adiponectin concentration and fatty acid oxidation in healthy subjects. Eur J Clin Nutr 62, 1287–1293.
Harats D, Dabach Y, Hollander G, Ben-Naim M, Schwartz R, Berry EM et al. (1991). Fish oil ingestion in smokers and nonsmokers enhances peroxidation of plasma lipoproteins. Atherosclerosis 90, 127–139.
Harris WS, Mozaffarian D, Rimm E, Kris-Etherton P, Rudel LL, Appel LJ et al. (2009). Omega-6 fatty acids and risk for cardiovascular disease. A science advisory from the American Heart Association Nutrition Subcommittee of the Council on Nutrition, Physical Activity, and Metabolism; Council on Cardiovascular Nursing; and Council on Epidemiology and Prevention. Circulation 119, 902–907.
Higdon JV, Liu J, Du SH, Morrow JD, Ames BN, Wander RC (2000). Supplementation of postmenopausal women with fish oil rich in eicosapentaenoic acid and docosahexaenoic acid is not associated with greater in vivo lipid peroxidation compared with oils rich in oleate and linoleate as assessed by plasma malondialdehyde and F2-isoprostanes. Am J Clin Nutr 72, 714–722.
Hillier K, Jewell R, Dorrell L, Smith CL (1991). Incorporation of fatty acids from fish oil and olive oil into colonic mucosal lipids and effects upon eicosanoid synthesis in inflammatory bowel disease. Gut 32, 1151–1155.
Hull J, Vervaart P, Grimwood K, Phelan P (1997). Pulmonary oxidative stress response in young children with cystic fibrosis. Thorax 52, 557–560.
Hussein N, Ah-Sing E, Wilkinson P, Leach C, Griffin BA, Millward DJ (2005). Long-chain conversion of (13C)linoleic acid and α-linolenic acid in response to marked changes in their dietary intake in men. J Lipid Res 46, 269–280.
Koutroubakis IE, Malliaraki N, Dimoulios PD, Karmiris K, Castanas E, Kouroumalis EA (2004). Decreased total and corrected antioxidant capacity in patients with inflammatory bowel disease. Dig Dis Sci 49, 1433–1437.
Kruidenier L, Kuiper I, Lamers CBHW, Verspaget HW (2003). Intestinal oxidative damage in inflammatory bowel disease: semi-quantification, localization, and association with mucosal antioxidants. J Pathol 201, 28–36.
Lee DS, Evans JC, Robins SJ, Wilson PW, Albano I, Fox CS et al. (2007). Gamma glutamyl transferase and metabolic syndrome, cardiovascular disease, and mortality risk: the Framingham Heart Study. Arterioscler Thromb Vasc Biol 27, 127–133.
Liou YA, King DJ, Zibrik D, Innis SM (2007). Decreasing linoleic acid with constant α-linolenic acid in dietary fats increases (n-3) eicosapentaenoic acid in plasma phospholipids in healthy men. J Nutr 137, 945–952.
Ma TY (1997). Intestinal epithelial barrier dysfunction in Crohn's disease. Proc Soc Exp Biol Med 214, 318–327.
Mann STW, Stracke H, Lange U, Klör HU, Teichmann J (2003). Vitamin D3 in patients with various grades of chronic pancreatitis, according to morphological and functional criteria of the pancreas. Dig Dis Sci 48, 533–538.
Meisinger C, Döring A, Schneider A, Löwel H, for the KORA Study Group (2006). Serum γ-glutamyltransferase is a predictor of incident coronary events in apparently healthy men from the general population. Atherosclerosis 189, 297–302.
Meister D, Ghosh S (2005). Effect of fish oil enriched enteral diet on inflammatory bowel disease tissues in organ culture: differential effects on ulcerative colitis and Crohn's disease. World J Gastroenterol 11, 7466–7472.
Mills SC, Windsor AC, Knight SC (2005). The potential interactions between polyunsaturated fatty acids and colonic inflammatory processes. Clin Exp Immunol 142, 216–228.
Mori TA (2004). Effect of fish and fish oil-derived omega-3 fatty acids on lipid oxidation. Redox Rep 9, 193–197.
Morrow JD, Chen Y, Brame CJ, Yang J, Sanchez SC, Xu J et al. (1999). The isoprostanes: unique prostaglandin-like products of free-radical-initiated lipid peroxidation. Drug Metab Rev 31, 117–139.
Nielsen AA, Jörgensen LGM, Nielsen JN, Eivindson M, Grönbaek H, Vind I et al. (2005). Omega-3 fatty acids inhibit an increase of proinflammatory cytokines in patients with active Crohn's disease compared with omega-6 fatty acids. Aliment Pharmacol Ther 22, 1121–1128.
Peretti N, Roy CC, Drouin E, Seidman E, Brochu P, Casimir G et al. (2006). Abnormal intracellular lipid processing contributes to fat malabsorption in cystic fibrosis patients. Am J Physiol Gastrointest Liver Physiol 290, G609–G615.
Periago JL, Suarez MD, Pita ML (1990). Effect of dietary olive oil, corn oil and medium-chain triglycerides on the lipid composition of rat red blood cell membranes. J Nutr 120, 986–994.
Rantala AO, Lilja M, Kauma H, Savolainen MJ, Reunanen A, Kesäniemi YA (2000). Gamma-glutamyl transpeptidase and the metabolic syndrome. J Intern Med 248, 230–238.
Romano C, Cucchiara S, Barabino A, Annese V, Sferlazzas C (2005). Usefulness of ω-3 fatty acid supplementation in addition to mesalazine in maintaining remission in pediatric Crohn's disease: a double-blind, randomized, placebo-controlled study. World J Gastroenterol 11, 7118–7121.
Sabanayagam C, Shankar A, Li JL, Pollard C, Ducatman A (2009). Serum gamma-glutamyl transferase level and diabetes mellitus among US adults. Eur J Epidemiol 24, 369–373.
Saito M, Kubo K (2003). Relationship between tissue lipid peroxidation and peroxidizability index after α-linolenic, eicosapentaenoic, or docosahexaenoic acid intake in rats. Br J Nutr 89, 19–28.
Shankar A, Li J, Klein BEK, Nieto FJ, Klein R (2008). Serum gamma-glutamyltransferase level and peripheral arterial disease. Atherosclerosis 199, 102–109.
Trebble TM, Arden NK, Wootton SA, Calder PC, Mullee MA, Fine DR et al. (2004). Fish oil and antioxidants alter the composition and function of circulating mononuclear cells in Crohn disease. Am J Clin Nutr 80, 1137–1144.
Vuilleumier JP, Keller HE, Gysel D, Hunziker F (1983). Clinical chemical methods for the routine assessment of the vitamin status in human populations. Part I: the fat-soluble vitamins A and E, and beta-carotene. Int J Vitam Nutr Res 53, 265–272.
Whitfield JB (2001). Gamma glutamyl transferase. Crit Rev Clin Lab Sci 38, 263–355.
Whiting CV, Bland PW, Tarlton JF (2005). Dietary n-3 polyunsaturated fatty acids reduce disease and colonic proinflammatory cytokines in a mouse model of colitis. Inflamm Bowel Dis 11, 340–349.
Zhao S, Jia L, Gao P, Li Q, Lu X, Li J et al. (2008). Study on the effect of eicosapentaenoic acid on phospholipids composition in membrane microdomains of tight junctions of epithelial cells by liquid chromatography/electrospray mass spectrometry. J Pharm Biomed Anal 47, 343–350.
Acknowledgements
CM coordinated the study and acted as an expert on fatty acid metabolism; RS conducted the study; RS and CM constituted the writing group and prepared this paper; BA and PS set up and performed the laboratory method of analysis of erythrocyte membrane fatty acids, plasma fat-soluble vitamins and 8-isoprostanes; BT was responsible for patient inclusion; BJ contributed to the collection of dietary and biochemical data; and NB conducted the statistical analysis. This study was supported in part by a research grant from Meduna Ltd, Isernhagen, Germany. Professor Metzner was a consultant for Meduna Ltd, Isernhagen, Germany. All authors contributed to the final version of the paper and gave their approval to publish the final version.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Siener, R., Alteheld, B., Terjung, B. et al. Change in the fatty acid pattern of erythrocyte membrane phospholipids after oral supplementation of specific fatty acids in patients with gastrointestinal diseases. Eur J Clin Nutr 64, 410–418 (2010). https://doi.org/10.1038/ejcn.2009.151
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2009.151
Keywords
This article is cited by
-
Effects of Cold Pressed Chia Seed Oil Intake on Hematological and Biochemical Biomarkers in Both Normal and Hypercholesterolemic Rabbits
Plant Foods for Human Nutrition (2023)
-
Increased intestinal permeability exacerbates sepsis through reduced hepatic SCD-1 activity and dysregulated iron recycling
Nature Communications (2020)
-
Ameliorative effect of flaxseed oil against thiacloprid-induced toxicity in rats: hematological, biochemical, and histopathological study
Environmental Science and Pollution Research (2016)
-
Consumption of Dietary n‐3 Fatty Acids Decreases Fat Deposition and Adipocyte Size, but Increases Oxidative Susceptibility in Broiler Chickens
Lipids (2013)
-
Effects of flaxseed oil on anti-oxidative system and membrane deformation of human peripheral blood erythrocytes in high glucose level
Lipids in Health and Disease (2012)