Abstract
Background/Objectives:
We have shown earlier that consumption of moderate amount of oats improve intakes of vitamin B1, fiber, magnesium and iron in celiac patients using gluten-free diet (GFD). The objective of this study was to clarify the effect of high amount of both kilned and unkilned oats on food and nutrient intakes in celiac patients in remission. Kilning as an industrial heating process is performed to preserve the main properties of oats and to lengthen its useableness. Kilning may, however, change the protein structure of oats and therefore influence on the intake of nutrients.
Subjects/Methods:
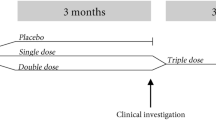
The study group consisted of 13 men and 18 women with celiac disease in remission. The patients who were earlier using moderate amount of oats as part of their GFD were randomized to consume kilned or unkilned oats. After 6 months, the patients changed the treatment groups. The goal of daily intake of oats was 100 g. Food records and frequency questionnaire were used to follow nutrient intakes.
Results:
Type of oats did not affect the amount of oats used. In the group using kilned oats, the intake of vitamin B1 and magnesium and in the group of unkilned oats that of magnesium and zinc increased significantly during the first 6 months (P⩽0.05).
Conclusions:
Large amounts of oats, both kilned and unkilned in GFD, can increase intakes of nutrients in celiac patients in remission. Oats improve the nutritional value of GFD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Arentz–Hansen H, Fleckenstein B, Molberg Ø, Scott H, Koning F, Jung G et al. (2004). The molecular basis for oat intolerance in patients with celiac disease. Plots Med 1, e1.
Björkman A, Mobacken H, Kastrup W, Anderson H (1985). Changes in food consumption and its nutritional quality when on a gluten- free diet for dermatitis herpetiformis. Hum Nutr Appl Nutr 39A, 124–129.
Ciclitira PJ, Ellis HJ, Lundin KE (2005). Gluten -free diet—what is toxic? Best Pract Res Clin Gastroenterol 19, 359–371.
Collins B, Bell P, Thomson J, Fee D, Wilson E, Love A (1986). Dietary history and nutritional state in treated coeliac patients. J R Soc Med 79, 206–209.
Ganssmann W, Vorwerek K (1995). Oat milling processing and storage. In: Welch R (ed). The Oat Crop: Production and Utilization. Chapman & Hall: London. pp 369–408.
Hakala-Lahtinen P, Puumalainen R, Metsäranta L (1981). Celiakipatienters konsumtion av livsmedel, samt deras näringsintag och matutgifter (in Swedish with English summary). Näringsforskning 25, 104–107.
Hardman C, Garioch J, Leonard J, Thomas H, Walker M, Lortan J et al. (1997). Absence of toxicity of oats in patients with dermatitis herpetiformis. N Engl J Med 337, 1884–1887.
Hartman A, Brown C, Palmgren J, Pietinen P, Verkasalo M, Myer D et al. (1990). Variability in nutrient and food intakes among older middle-aged men. Implications for design of epidemiologic and validations studies using food recording. Am J Epidemiol 132, 999–1012.
Hernando A, Mujico J, Mena M, Lombardia M, Mendez E (2008). Measurement of wheat gluten and barley hordeins in contaminated oats from Europe, the United States and Canada by Sandwich R5 Elisa. Eur J Gastroenterol Hepatol 20, 545–554.
Hoffenberg E, Haas J, Drescher A, Barnhurst R, Osberg T, Bao F et al. (2000). A trial of oats in children with newly diagnosed celiac disease. J Pediatr 137, 361–366.
Högberg L, Laurin P, Fälth-Magnusson K, Grant C, Grodzinsky E, Jansson G et al. (2004). Oats to children with newly diagnosed coeliac disease: a randomised double blind study. Gut 53, 649–654.
Janatuinen E, Kemppainen T, Julkunen R, Kosma V-M, Mäki M, Heikkinen M et al. (2002). No harm from five year ingestion of oats in coeliac disease. Gut 50, 332–335.
Janatuinen E, Kemppainen T, Pikkarainen P, Holm K, Kosma V-M, Uusitupa M et al. (2000). Lack of cellular and humoral immunological responses to oats in adults with coeliac disease. Gut 46, 327–331.
Janatuinen E, Pikkarainen P, Kemppainen T, Kosma V-M, Järvinen R, Uusitupa M et al. (1995). A comparison of diets with or without oats in adults with celiac disease. N Engl J Med 333, 1033–1037.
Kemppainen T (1997). Oat meal as a component of a gluten-free diet, nutrient intakes, nutritional status and osteopenia in coeliac patients. Kuopio University Publications, Medical Sciences 118.
Kemppainen T, Kosma V-M, Janatuinen E, Julkunen R, Pikkarainen P, Uusitupa M (1998). Nutritional status of newly diagnosed celiac disease patients before and after the institution of a celiac disease-diet.-association with the grade of mucosa villous atrophy. Am J Clin Nutr 67, 482–487.
Kemppainen T, Heikkinen M, Ristikankare M, Kosma V-M, Julkunen R (2009). Effect of unkilned and large amounts of oats on nutritional state of celiac patients in remission. e-SPEN Eur e-J Clin Nutr Metabol 4, e30–e34.
Kemppainen T, Heikkinen M, Ristikankare M, Kosma V-M, Sontag-Strohm T, Brinck O et al. (2008). Unkilned and large amounts of oats in the coeliac disease diet : a randomized, controlled study. Scand J Gastroenterol 43, 1094–1101.
Kemppainen T, Uusitupa M, Janatuinen E, Järvinen R, Julkunen R, Pikkarainen P (1995). Intakes of nutrients and nutritional status in coeliac patients. Scand J Gastroenterol 30, 575–579.
Kinsey L, Burden ST, Bannerman E (2008). A dietary survey to determine if patients with coeliac disease are meeting current healthy eating quidelines and how their diet compares to that of the British general population. Eur J Clin Nutr 62, 1333–1342.
Lundin K, Nilsen E, Scott H, Løberg E, Gjøen A, Brattle J et al. (2003). Oats induced villous atrophy in coeliac disease. Gut 52, 1649–1652.
McFarlane X, Marsham J, Reeves D, Bhalla A, Robertson D (1995). Subclinical nutritional deficiency in treated celiac disease and nutritional content of the gluten free diet. J. Hum Nutr Dietet 8, 231–237.
Reunala T, Collin P, Holm K, Pikkarainen P, Miettinen A, Vuolteenaho N et al. (1998). Tolerance to oats in dermatitis herpetiformis. Gut 43, 490–493.
Roy-Choudhury F, Cooke WT, Banswell JG, Smith RJ (1966). Jejunal biopsy: criteria and significance. Scand J Gastroenterol 1, 57–74.
Siegel S, Gastellan Jr N (1988). Multiple comparisons between groups on conditions. In: Siegel S, Castellan N (eds). Nonparametric Statistics for the Behavioural Sciences. McGraw-Hill Book Company: New York. pp 180–181.
Srinivasan U, Leonard N, Jones E, Kasarda DD, Weir D, O’Farelly C et al. (1996). Absence of oats toxicity in adult coeliac disease. Br Med J 313, 1300–1301.
Størsrud S, Hulthen L, Lenner R (2003a). Beneficial effects of oats in the gluten-free diet of adults with special reference to nutrient status, symptoms and subjective experiences. Br J Nutr 90, 101–107.
Størstrud S, Olsson M, Arvidsson Lenner R, Nilsson L, Nilsson O, Kilander A (2003b). Adult coeliac patients do tolerate large amounts of oats. Eur J Clin Nutr 57, 163–169.
Thompson T, Dennis M, Higgins LA, Lee AR, Sharrett MK (2005). Gluten free diet survey: are Americans with coeliac disease consuming recommended amounts of fibre, iron, calcium and grain foods. J Hum Nutr Diet 18, 163–169.
Wahab P, Meijer J, Mulder C (2002). Histological follow-up of people with celiac disease on a gluten-free diet: slow and incomplete recovery. Am J Clin Pathol 118, 459–463.
Acknowledgements
This study was supported by the Finnish Cultural Foundation, Antti and Jenny Wihuri Foundation and EVO funding of Kuopio University Hospital. Melia OY, Raisio Group, Raisio, Finland, Farina Oy, Virtasalmi, Finland and Moilanen bakery, Moilas Oy, Naarajärvi, Finland (gluten-free bakery) contributed oats and oat products to the project. Department of Food Technology, University of Helsinki has investigated the purity of oats.
Author information
Authors and Affiliations
Corresponding author
Additional information
Contributors: Each author has participated sufficiently to take public responsibility for the work. TAK, RJJ, MKR, MTH and VMK carried out the study. TAK participated in the design of the study, performed the statistical analysis and drafted the paper. RJJ conceived the study, and participated in its design and coordination and helped to draft the paper. All authors have read and approved the final paper.
Rights and permissions
About this article
Cite this article
Kemppainen, T., Heikkinen, M., Ristikankare, M. et al. Nutrient intakes during diets including unkilned and large amounts of oats in celiac disease. Eur J Clin Nutr 64, 62–67 (2010). https://doi.org/10.1038/ejcn.2009.113
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2009.113
Keywords
This article is cited by
-
Detection of gluten content in both naturally and labelled gluten-free products available in Morocco
Journal of Consumer Protection and Food Safety (2022)
-
A Comprehensive Review of Celiac Disease/Gluten-Sensitive Enteropathies
Clinical Reviews in Allergy & Immunology (2019)
-
Effects of 3 g of soluble fiber from oats on lipid levels of Asian Indians - a randomized controlled, parallel arm study
Lipids in Health and Disease (2017)
-
Characterization of celiac disease related oat proteins: bases for the development of high quality oat varieties suitable for celiac patients
Scientific Reports (2017)
-
Celiac disease: a clinical review
Abdominal Radiology (2017)