Illustration of antibodies (red and blue) responding to an infection with the new coronavirus SARS-CoV-2 (purple). Credit: KTSDESIGN/SPL/ GETTY IMAGES
This spring, as the coronavirus outbreak killed thousands in Italy, Stefano Casola decided he could no longer sit at home. Trained as a medical doctor, Casola left clinical work more than 20 years ago to research the molecular basis of lymphoma—a type of blood cancer. In March, as a country-wide lockdown shut down his laboratory at Istituto FIRC di Oncologia Molecolare in Milan, Casola scrambled to find a way to contribute to the fight against the pandemic. “I told myself, let’s leave the lymphoma projects aside for the moment and use everything we know in the lab to help,” he recalls.
Casola is one of dozens of scientists in Italy who have reconfigured their labs to tackle the pandemic. In a country hurt by cuts to basic science spending, a flurry of funding to support COVID-19 research pushed many researchers to refocus expertise, protocols and equipment on diagnostic and therapeutic solutions. And as the Italian government imposes new restrictions amid a second virus surge, researchers hope that working on a coronavirus-related study will help them to keep their labs open.
“In March, April and May, many researchers tried to pivot towards SARS-CoV-2, partly because it was the only way to be able to work,” says Matteo Iannacone, an immunologist at Ospedale San Raffaele in Milan who is developing new mouse models of the disease. “Now, the gap has widened between those who have produced results and those who haven’t, so many went back to what they were doing before,” he says. But, he adds, research funders set the agenda. “If there’s a lot of coronavirus-related funding, labs will try to get it.”
Open questions
Italy was the European country hit hardest at the start of the pandemic. In April, the Italian Ministry of Health earmarked €7 million to support research aimed at containing the spread of the virus and understanding the disease. Some regional governments also announced funding for coronavirus-related research. Lombardy, Italy’s worst-hit region in the first wave of COVID-19, invested €4 million, and more came from universities and charitable organizations.
At that time, there were many open questions about how immunity to SARS-CoV-2 develops and whether people who had recovered were protected against reinfection, Casola says. For years, his group has studied how lymphomas arise from alterations in the DNA of immune cells that fight off infections. He decided to use his team’s expertise to set up a test that can identify antibodies against the virus in a drop of blood. By identifying more subtypes of the longer-lived antibodies that linger in the body for months or years, he says, the test would be better suited than existing ones to tell whether someone has acquired long-term immunity. The test has not yet been approved for use in hospitals and doctor’s offices, but Casola’s team used it to track the immune response of a group of health-care workers in Brescia who have recovered from the illness months ago. So far, all have shown a robust immune response which suggests a lasting protection, Casola says.
The researchers are also sieving the blood from the same individuals, looking for the antibody that’s best at sticking to the protein used by the virus to enter cells. A few antibodies-based treatments are already authorized for use, or in clinical trials, but more will be required even if there is a vaccine, to treat patients with a compromised immune system, or who do not respond to it.
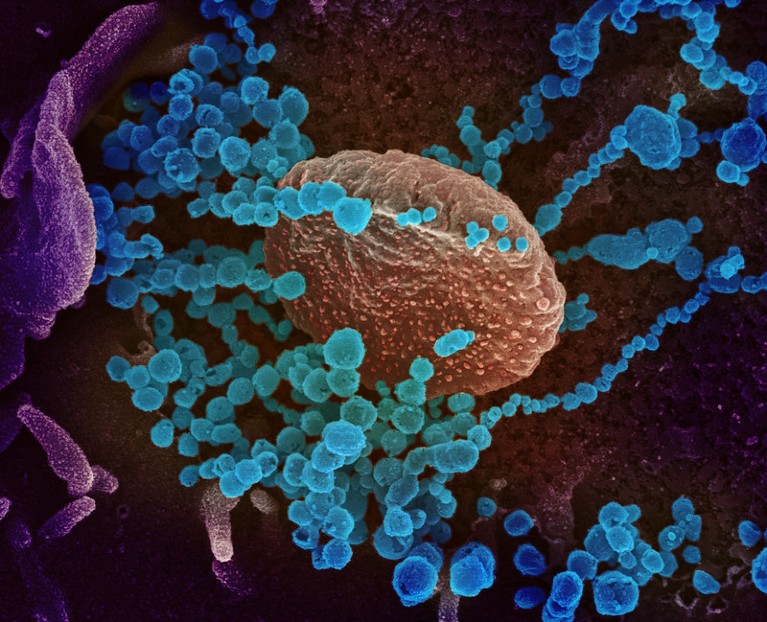
Scanning electron microscope image of SARS-CoV-2 (round blue objects) emerging from the surface of cells cultured in the lab. Credit: NIAID-RML
Other researchers used the lockdown to develop COVID-19 projects. Pediatrician Carla Colombo, at the Policlinico di Milano, usually studies cystic fibrosis, a genetic disease that causes persistent lung infections. After the pandemic struck, she reached out to researchers across Italy to develop a project that will track the outcome of COVID-19 in different groups of people, including those with cystic fibrosis or with other respiratory conditions. The study, which has been awarded nearly €800,000 in funding from the Ministry of Health, will also analyse which proteins are expressed in lung cells from COVID-19 patients, with the aim of identifying biomarkers for severe disease and therapeutic targets.
Even if in the next weeks the Italian government shuts down universities and labs to halt a second wave of coronavirus, Colombo’s study will probably be considered essential. “Sadly”, there won’t be a shortage of coronavirus-positive samples either, Colombo says. “We hoped the second wave wouldn’t be so big.”
Joining forces
According to Barbara Montanini, a molecular biologist at the Università di Parma, perhaps the only benefit of the pandemic is that it has encouraged scientists to collaborate. A few years ago, Montanini and her collaborators developed a screening platform to look for molecules that block the interaction between two proteins. They used it to identify compounds that could interfere with bacterial growth and be used as antibiotics. Now, she’s joined forces with other researchers to repurpose the platform to find molecules that could prevent coronavirus proteins from binding to receptors on human cells. If safe and effective, the drug could be produced in large scale, freeze-dried and administered in the form of an oral spray. In September, the study was awarded a €47,000 grant from the Università di Parma, but the researchers had already gotten to work. “We were so passionate that we had started investing money from unallocated funds,” Montanini says.
Others invested their own lab funds in COVID-19 studies. Structural biologist, Federico Forneris of the Università di Pavia, who ordinarily studies how collagen production contributes to cancer metastasis, used money from previous grants to produce large quantities of key SARS-CoV-2 proteins as well as the human protein that provides the entry point for the virus. The proteins have been used by other research groups to develop an antibody test for the coronavirus and to investigate how its ability to bind to human receptors has changed over time. The test is now awaiting authorization from the Ministry of Health to make it available for public use.
Forneris notes that working on COVID-19 gave his team a competitive edge. When the lab shut down in March, the researchers had to stop all the cell cultures used to make proteins—one of the lab’s biggest assets. But in mid-May, they were allowed back in the lab to work on the COVID-19 studies, and could restart the cultures. “This saved us time in all the other projects,” Forneris says. What’s more, coronavirus proteins are in such high demand that Forneris is now considering a spin-off for producing them on industrial scale.
Vaccines are not the end of the story
Nearly 10 months into the pandemic, huge progress has been made in diagnostic, therapeutic and vaccine approaches, but little is known about why some people fare much worse than others if infected. “Without an animal model, we’ll never know,” says Iannacone, who usually focuses on how the immune system evolved to respond to pathogens. Mice don't get sick from the virus. Scientists have genetically modified them with the human version of the receptor, but that is not enough to cause the most severe symptoms seen in humans. Hoping to obtain a model that better reproduces COVID-19, Iannacone and his team have engineered mice in various ways, including modifying their receptor.

A better mouse model of COVID-19 would allow to study why some patients have worse symptoms than others. Credit: dra_schwartz/ E+/ Getty Images
In order to work safely with coronavirus-infected mice, Iannacone’s lab had to buy new equipment and create dedicated rooms in the animal facility. “Thanks to donations from Italian entrepreneurs, we could make it happen,” he says. He worries that the funding spree will not last. If an effective vaccine is rolled out soon, governments and funders may consider the problem solved and cut investments in basic research. That could be dangerous, he says. “This pandemic is so dire because the necessary basic research work on coronaviruses had not been done.”
While Iannacone plans to continue working on COVID-19 even after the outbreak, others look forward to going back full-time to their pre-pandemic research. “I’ve entered the COVID field to help in a difficult time,” Casola says. “I’ll get out of it when I have made my contribution.”
