Credit: Bettmann / Getty Images
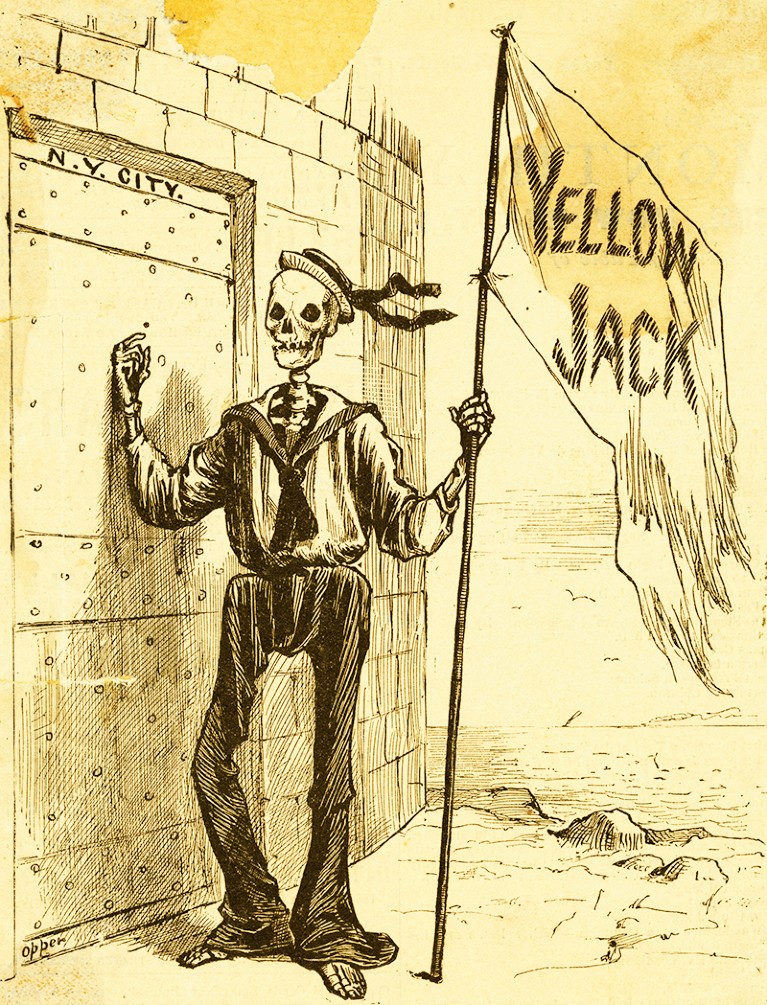
By the end of the 19th century, the feared yellow fever (often known as ‘yellow jack’ owing to the yellow quarantine flag on infected ships) had reached South America, the USA and Europe. Caused by a zoonotic flavivirus spread by an infected female mosquito, mostly Aedes aegypti, the slave trade and global markets had helped to spread the disease around the world. Yellow fever is now endemic in large parts of sub-Saharan Africa and tropical South America, with the vast majority of cases occurring on the African subcontinent.
Yellow fever symptoms include chills, nausea, loss of appetite, headaches and muscle pain. In most people, these symptoms improve in around 5 days; however, for around 15% of cases, the fever returns with abdominal pain, jaundice and liver damage. Up to half of these individuals with severe disease will die.
Unsuccessful attempts to create a vaccine for yellow fever — including vaccines against a spirochaete or other bacteria — date back to the late 19th and early 20th centuries, before the causative agent of yellow fever had been identified. This is where South African virologist Max Theiler enters the story. Theiler started his work on yellow fever at the Harvard University School of Tropical Medicine in the USA. He and his colleagues confirmed that the disease was viral, and by 1928 they had shown that the same virus was responsible for both the African and South American pools of disease.
Researchers at the Rockefeller Foundation in the USA isolated the causative virus from the blood of a Ghanaian man called Asibi, and a team from the Institut Pasteur in Dakar, Senegal isolated the ‘French strain’ of the virus from a Lebanese man, Francoise Mayali. Once in the lab, these researchers found that serum from patients with yellow fever protected monkeys from infection but that killed virus was not effective at inducing immunity.
In 1930, Theiler moved to the Rockefeller Foundation in New York, where he worked to reduce the pathogenicity of the virus so that it could be used as a vaccine that triggered immunity but did not cause systemic damage. He showed that repeated passage in mouse brain cultures reduced the effect of the virus on most organs, but potentially increased its impact on the central nervous system, which could cause encephalitis. In 1931, after around 100 passages in mouse brain, the Rockefeller Institute tested a modified French strain as a vaccine, in combination with immune serum from recovered patients to reduce the risk of encephalitis. But the risk of neurotoxicity was still there and the large quantities of serum that were required made it hard to scale up its use. So, another approach was needed.
In a sequence of three publications in the Journal of Experimental Medicine in 1937, Max Theiler and Hugh Smith described the development of a live attenuated yellow fever vaccine strain using tissue from embryonated chicken eggs. The researchers focused on the Asibi strain, from which strain 17D was isolated after 176 passages initially in mouse embryonic tissue and monkey serum, and later in minced whole chick embryo, then in chick embryo from which the brain and spinal cord had been removed. 17D had lost neurotropism, viscerotropism and mosquito competence, but it still had the potential to trigger an immune response.
Ernest Goodpasture, a US pathologist and medic, should be given due credit for paving the way for this stage of the research. Working in the early 1930s, he and his fellow researchers were the first to reproducibly grow pure viruses in culture by infecting fertilized chicken eggs. Prior to this, viruses could only be studied in costly animal models or in tissue cultures that were prone to contamination by bacteria because antibiotics were not yet available.
The next step for Theiler and his team was to see whether a 17D vaccine prepared from infected whole chick embryos was safe and effective for human use without the addition of human serum, the bottleneck for Theiler’s previous vaccine. In a study in rhesus monkeys, the vaccine triggered antibodies in all monkeys by 14 days and immunity to infection after a week. There were few adverse effects in the monkeys, so the researchers vaccinated four people who were already immune and eight people with no immunity. All developed antibody responses, and adverse effects were limited to mild fever, headache and backache. The positive results of this preliminary trial led to further larger studies.
The 17D vaccine received licensing approval in 1938, with more than 850 million doses having been distributed since. The vaccine is well tolerated, up to 100% effective and affordable, and it can provide lifelong protection with a single vaccination. Serious side effects are rare. In 1951, Theiler was awarded the Nobel Prize in Physiology or Medicine for “discoveries concerning yellow fever and how to combat it”, the first and only time that the prize has been awarded for a vaccine.

 Nature Milestones in Vaccines: Interactive Timeline
Nature Milestones in Vaccines: Interactive Timeline
 The adaptation of unmodified strains of yellow fever virus to cultivation in vitro. (Smith, H. H. & Theiler, M., 1937)
The adaptation of unmodified strains of yellow fever virus to cultivation in vitro. (Smith, H. H. & Theiler, M., 1937)