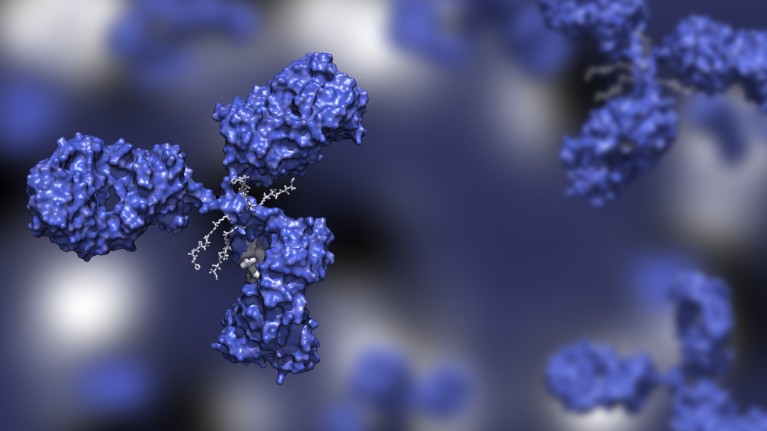
Antibody-drug conjugates are hybrid constructs comprising three main components: the antibody backbone, the cytotoxic payload and the linker that binds them.Credit: Huen Structure Bio/Shutterstock.com.
Antibody–drug conjugates (ADCs) are among the fastest growing therapeutic modalities in modern cancer drug research and development. These medicines combine the tumour-targeting properties of antibodies with the cytotoxic potency of chemotherapeutics, enabling destructive compounds to be smuggled past healthy tissues to hit their targets. Although the history of ADC development spans decades, recent clinical successes — along with advances in antibody engineering, chemical synthesis and cancer biology — have brought a renaissance in ADC research.
“With this new wave of investment, I have no doubt we’ll see more ADCs approved across a broader set of cancers,” says Scott Peterson, head of ADC discovery and cancer immunology at Pfizer.
Traditional ADCs are engineered with a DNA-damaging or microtubule-targeting agent tethered to a monoclonal antibody. Once bound to the antibody’s target, the complex is internalized by the cell and the cytotoxic payload is released. This mechanism has already proven effective in several solid tumours and blood cancers. ADCs have received FDA approval for 20 indications and more than 100 others are in development (Tsuchikama, K. et al. Nature Rev. Clin. Oncol. 21, 203–223; 2024).
Like other therapeutics, ADCs are limited by off-tumour toxicities, resistance and challenging pharmacokinetics (Gogia, P. et al. Cancers https://doi.org/mqcc; 2023). To overcome these hurdles, researchers are exploring next-generation ADC designs incorporating novel payloads, modified antibody backbones and new drug linker-release mechanisms. This is a multifaceted process, says Peterson, “with many moving parts that each require exploration and optimization”.
Designing a new generation
ADCs consist of three modifiable primary components: the antibody backbone, the cytotoxic payload and the linker that joins the two.
The drug linker is typically created as a peptide or carbohydrate that is cleaved inside the tumour cell after internalization to release the payload. These payloads may diffuse beyond the targeted cell to destroy adjacent tumour cells. Though this may impact neighbouring tissue, it can spread therapeutic effects to malignant cells that lack the targeted antigen.
ADCs can incorporate multiple linkers to increase the concentration of delivered cytotoxin. However, there’s a limit. “Conjugating too many payloads can be counterproductive,” explains Peterson. “They can cause the ADCs to aggregate and have a shorter half-life. You can’t just pile linkers on — there’s always a trade-off.”
Peterson’s team at Pfizer is exploring next generation ADC designs, with several programmes in clinical development. These include programmes that employ a novel topoisomerase 1 (TOPO1) inhibitor payload, including Pfizer’s TOPO1-ADC, which targets CEACAM5, and 35C, a next-generation CD30-targeted ADC. The company is also pursuing ADCs with next-generation auristatin payloads that could improve tolerability.
Pfizer has programmes in discovery and pre clinical stages that employ payloads with distinct mechanisms of action, from immune agonist payloads to protein degrader payloads and novel cytotoxic payloads.
“I’m particularly enthusiastic about our TOPO1 ADC drug linker, which complements our vedotin ADC technology, and for new payload mechanisms of action such as protein degraders,” says Peterson. Protein degraders are a molecular class designed to transport a target protein to, and activate, native protein degradation machinery. This opens the door to targets that have been difficult to reach with small molecules.
“There’s huge promise in the future of ADCs,” says Peterson. “The investment we've seen will drive innovation, and the more we do, the better it’ll get for cancer patients. That's why we're in this: to do best by the patients.”


