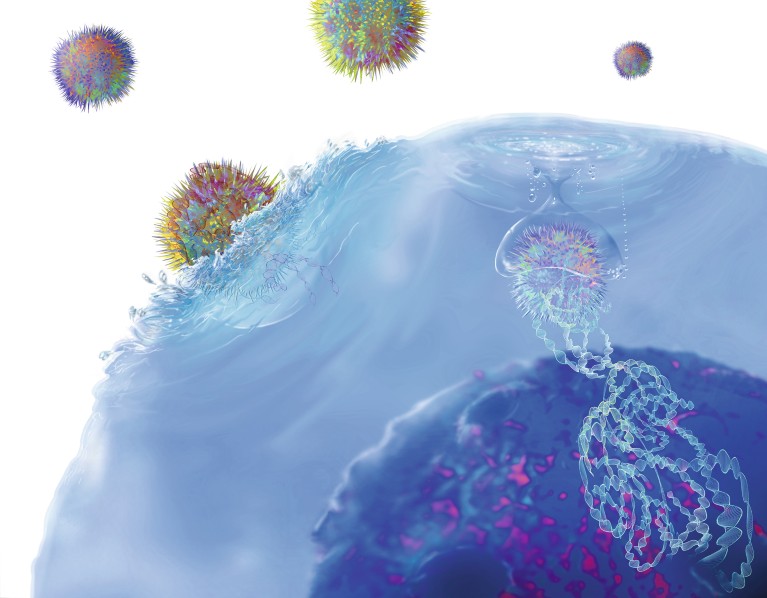
Viruses modify T cell DNA to produce chimeric antigen receptor (CAR) proteins.
Even as our understanding of the immune systems grows, one thing remains constant: T cells have a fundamental role in many diseases and their treatments.
In fact, Michael Vincent, Pfizer’s chief scientific officer, inflammation & immunology, calls T cells the generals of the immune system. “Everything else is carried out as effector functions of this system,” he says, “but there’s always a T cell at the helm, directing the activity.” Three areas, in particular, are major priorities for T-cell therapy: inflammation, cancer and infectious diseases.
Unravelling inflammation
The range of inflammatory diseases that can potentially benefit from T-cell therapies is “almost unlimited,” says Vincent. “For any disease where inflammation is causing bodily harm, that’s a potential area where modulating T-cell targets could be beneficial.”
For many autoimmune diseases, “The underlying issue is that the body’s ability to discriminate what it should and shouldn’t attack has been subverted,” says Vincent. “That recognition process is fundamentally what the T cell does.” Pfizer is working on treatments that directly target the cause of autoimmune diseases by modifying T cells or their actions.
T cells often play an initiating role in inflammation. In psoriasis, for example, dendritic cells cause specific T cells to release cytokines that cause inflammation of the skin. Many existing psoriasis therapies target key cytokines that drive the characteristic skin changes, but Pfizer wants to understand why T cells are reacting this way to begin with, so its scientists can design therapies that move up the chain to address the T cells that release them.
Understanding and attacking cancer
Pfizer is also keen to understand the T-cell subsets that are most likely to contribute to anti-tumour immunity that directs the T cells to attack specific features of cancer cells. “Much of our focus is on killer T cells, which are activated and recruited into a tumour,” says Robert Rickert, chief scientific officer, cancer immunology discovery at Pfizer.
Some of the key advances in treating cancer are focused on targeting treatments to the tumour. Rickert describes bispecific antibodies, which bind both a T cell and a tumour cell, bringing the immune effector directly to the cancer cell. Future treatments could potentially help T cells recognize peptide neoantigens that are only presented by cancer cells, allowing T cells to kill them and avoid healthy cells.
Other options include CAR-T therapies, which add a chimeric antigen receptor (CAR) to a patient’s T cells to help them attack the cancer.
Vaccines against infectious diseases
Vaccines aim to stimulate a protective immune response. Traditional vaccines include a weakened or inactivated virus. They are manufactured in big batches then purified. For SARS-CoV-2, the virus behind COVID-19, Pfizer and BioNTech developed a vaccine with mRNA technology. Scientists synthesize the genetic code for the viral antigen, and can quickly and stably package it, typically in lipid nanoparticles. A vaccinated individual’s cellular machinery then reads the mRNA to make the specific antigen, which stimulates protective B and T cells.
“With mRNA technology, you generate the antibodies that can neutralize the pathogen,” says Annaliesa Anderson, senior vice president and chief scientific officer of Pfizer’s vaccine research and development. “But you’re also doing some T-cell imprinting that provides a memory.”
mRNA technology could also improve the T-cell response to potential vaccines for other infectious diseases. For example, Pfizer is developing an influenza vaccine candidate to potentially defend against four strains. “While our mRNA vaccine candidate is currently in a Phase 3 study, in early clinical studies, the vaccine seemed to be activating more T cells and stimulating better T-cell responses than the current flu vaccine we used in our studies,” Anderson says.
Added intelligence
Learning more about the role of the immune system in various diseases requires collecting data on wide range of T cells. Such work creates large datasets that can only be explored with artificial intelligence (AI). “A lot of the computational and machine-learning tasks allow us to take advantage of those molecular data to develop greater insights into disease and our clinical treatments,” Vincent says.
To learn even more, Pfizer partnered with Israel-based CytoReason, which creates AI-based algorithms. These tools may help identify which pathways and cells are active at the site of disease in many autoimmune conditions. “We can combine this with other information to make a kind of ‘Google map’ for a disease that shows the state of the immune system and the pathways that are up- and downregulated,” Vincent says.
Pfizer thinks that future vaccines and treatments will make even better use of T cells. “We’ve always known that T cells are important,” Anderson says, “but as we gain a deeper understanding of how they work, we’ll hopefully be able to activate the right T cells at the right time to provide the desired benefit for patients.”


