
The association between dietary fiber and digestive function has been known for many centuries. The Ancient Greeks reportedly understood that fibrous grains could help alleviate constipation. During the 1970’s Denis Burkitt1 linked fiber (or lack of fiber in Western diets) to broader aspects of health, including obesity, diabetes, cardiovascular disease (CVD), colon cancer and diverticulosis, in his ‘Dietary Fiber Hypothesis’. Proposing fiber as a key factor underlying these conditions was at that time hugely controversial, and stimulated much debate and research, which subsequently supported these associations. We have long known that fiber promotes regularity via stool bulking, due in part to fiber fueling microbial growth, contributing to increased mass. The gut microbiota paradigm fosters a new ‘Dietary Fiber Hypothesis’. While research continues to unravel its complexities, we already have sufficient understanding to reinvigorate the message to ‘eat more fiber’, and in particular to ‘eat more grain fiber’.
More than 100 years ago, W.K. Kellogg founded the company through his belief in nutrition and dedication to well-being. Motivated by a passion for people, quality and innovation, he created the first ever breakfast cereal, based on his understanding of the nutritional benefits of consuming fiber rich cereal grains. More than a century later, this legacy continues to inspire the Kellogg Company; by responding to consumer preferences and using evidence-based science as our guide, we continue on our journey to deliver nutrition through plant based foods. We actively support research to understand how our food and our company can contribute to health and wellness - sponsoring systematic literature reviews, in vitro and intervention studies to explore the effects of dietary manipulations, and epidemiological research to understand food intake behaviors and drivers for dietary change.
Developments in increasingly efficient high-throughput profiling provide sophisticated insight into the complexity of the gut microbial community. Modulating the gut microbiota is emerging as a plausible approach for promoting health, and targeting disease prevention and treatment.2 Changes in dietary macronutrients, including carbohydrate, fat and protein lead to measurable, rapid, person-specific shifts in the human gut microbiota. However, the sheer complexity of the gut microbiota community and wide array of influencing factors, mean that personalizing nutrition interventions to optimize gut microbiota still has challenges to overcome3. While we await research developments, we can already start to address one important question – if fiber intake is increased, will this affect the gut microbiota?
When translating research into practice, it is customary to carry out a systematic review: a methodology which summarizes results from available clinical studies. Systematic reviews of fiber-microbiota interventions have largely focused on isolated prebiotic fiber consumed as supplements4,5, or on prebiotic fiber efficacy for specific conditions, e.g. Irritable Bowel Syndrome (IBS)6. No systematic reviews had assessed whether consuming grain fiber from everyday foods such as breakfast cereals or breads – had any measurable effects on the gut microbiota in healthy individuals. Having identified this evidence gap, Kellogg provided a grant to independent dietitian and researcher Angie Jefferson, who collaborated with Dr. Katie Adolphus (at the time employed by Kellogg but now a Research Fellow at Leeds University, UK) to conduct a systematic review of this topic using PRISMA methodology.
The authors were particularly interested in wheat as it is an important contributor to fiber intakes in many Western societies. Authoritative recognition of wheat bran for digestive health benefits exists in the European Union (EFSA 2010 j.efsa.2010.1817), Canada (Health Canada), USA (US FDA Laxative Monograph), and Australia (Food Standards Australia New Zealand 2014). Wheat fiber is also the most studied cereal grain fiber in relation to its impact on regularity7, so understanding its effects on gut microbiota composition and function in healthy adults was a subsidiary aim of this review. The resulting paper can be freely accessed on-line8, and is outlined below.
Studies published between 1998-2018 were identified in the PubMed and Cochrane electronic databases. Relevant search terms included “microbiota,” or “prebiotic” in combination with “grain fiber or fiber”, “digestive health,” “wheat,” “oat,” etc. Eligible studies included: healthy adults (>18 years); at least one intact cereal grain fiber; and measurement of fecal microbiota related outcomes e.g. change in species abundance, diversity, and microbial metabolic indicators, e.g. short chain fatty acids (SCFA). As every individual has a unique microbiota, many trials utilized a cross-over design where individuals acted as their own control. 226 publications were identified, and 40 included into the final review.
Study outcomes are summarized in Table 1. Findings from a total of 1,308 participants, spanning 1 meal to 1 year were included. Wheat was the most commonly utilized fiber, provided as foods (e.g. wholewheat breads, wholegrain or bran cereals or pasta) in 27 of 40 studies. 9 studied wholegrain intake (predominantly wheat); 8 explored wheat fiber or bran; and a further 9 provided wheat bran derived arabinoxylan-oligosaccharides (AXOS). 5 studies reported on rye fiber. While the prebiotic effect of isolated beta-glucans on the gut microbiota has been studied extensively, only 2 studies were identified examining the effects of intact oat fiber on the gut microbiota. Barley, rice and maize accounted for the remaining 8 studies.
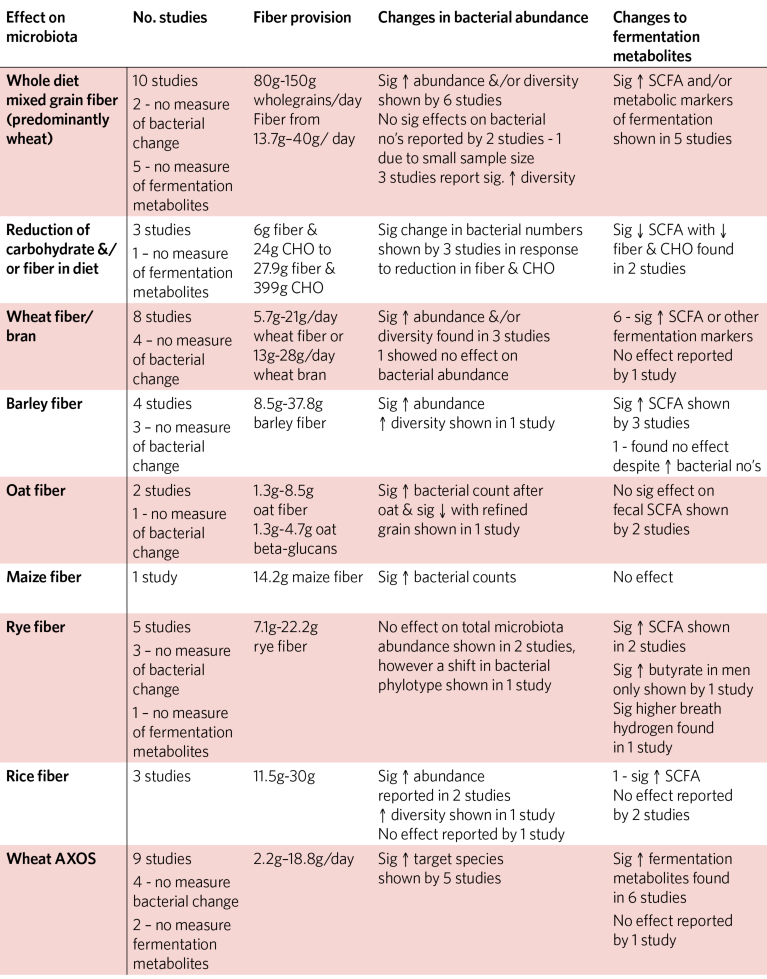
Table 1: Summary of Short-Term Effects of Fiber Manipulation on Gut Microbiota of Healthy Adults
When translating research into practice an important question is how much fiber was provided, and could this be consumed in a normal daily diet? Overall, reported fiber interventions ranged from 5.7g–40g/d. Four studies utilized a single daily serve of wheat bran fiber (5.7g-33g) at breakfast and all of these demonstrated significant prebiotic effect, measurable within 3 weeks and after 1 year.
Review results suggest that as little as 5.7g/d wheat fiber is sufficient to significantly modulate the gut microbiota, a finding in line with that of So et al who suggested that <5g fiber may be sufficient to stimulate bacterial growth5. Other cereal grains also appeared to stimulate gut microbiota at relatively low levels, with as little as 10 g barley fiber and 7g rye fiber providing measurable significant effect. Breakfast can provide a significant contribution to the daily fiber intakes of western populations9 and is an occasion where a switch to higher fiber foods can be easily achieved. A simple dietary modification to consume a daily bowl of a high fiber breakfast within a mixed habitual diet was shown to have a positive impact on the gut microbiota for healthy adults. Whether delivering a single bolus of fiber has different stimulatory effects on the gut microbiota compared to delivery of a steady stream of fiber throughout the day is a potential area for future research. Differences in inter-individual microbiota response were highlighted by three studies within this review. Individuals most responsive to cereal grain fiber had the lowest starting levels of the target bacteria, with variations in response as high as 10-fold. The authors propose that individuals likely to benefit most from an increase in cereal grain fiber intake are those who habitually consume low fiber foods.
Fiber is the primary fuel source for human gut microbiota. Sonnenburg et al therefore proposed that microbial accessibility of fiber is a key characteristic, coining the term Microbiota-Accessible Carbohydrates (MAC), and in Western diets where MAC consumption is low, Microbiota Insufficiency Syndrome (MIS)10. This systematic review provides reassurance that cereal grain fibers indeed provide MACs, and that reintroducing cereal grain fiber into habitual diets appears to have rapid, significant effect on both activity of the gut microbiota and diversity, increasing not only bacterial types able to utilize complex fiber structures, but also other bacterial species as a result of cross feeding relationships.
‘Eat more fiber-rich cereals’ appears to be a simple message, but fiber intakes remain woefully low across the globe, and intake behaviors are difficult to shift. Kellogg sponsored research in the USA and Australia has examined sources and intakes of fiber in children and adults. In the USA, across the 10-year period studied, mean fiber intake was 13.2 g/d for children 4-18yrs. and 16.1 g/d for adults 19-50yrs9. Across that period, even with consumer guidance and communications on the benefits of fiber, intakes increased on average by only about 1g. In Australia, fiber intakes are higher at 18.2 g/d in children and 20.7 g/d in adults, but still fall short, with only 42% of children and 28% of adults meeting recommendations11.
Increasing fiber intakes has potential additional benefits for healthcare savings. Kellogg funding has enabled modelling assessments to estimate potential savings in the USA, Canada, Australia, UK, Ireland and Spain – with startling results. In Europe, increasing daily fiber intake by 3-11 g/d could enable savings for constipation treatment by £127 million (UK), €9 million (Ireland), and €121 million (Spain)12. Looking beyond digestive health, if just 15% of Canadians consumed their recommended fiber intake, annual health care cost savings could amount to CAD$108 million and CAD$194million for costs associated with Type 2 diabetes and CVD respectively13. In Australia, if all adults consumed the recommended daily fiber intake, and both health care costs and productivity losses are considered, savings could rise to AUD$3 billion14. This however pales into insignificance compared to the potential $21.9 billion saving which could be achieved if all US adults increased fiber intake by 15g per day – equivalent to that contained in a bowl of All Bran® cereal plus 2 slices of wholegrain bread15.
Fiber is no longer the inert substance once thought, and it is increasingly apparent that consumption of a diverse range of plant foods to deliver a range of different fiber types is most likely the best way to support a symbiotic gut microbiota. Challenges remain in helping populations across the globe achieve adequate dietary fiber intakes for optimal health. Kellogg is committed not only to providing fiber, but also to continuing collaboration with academia, industry and regulators, and with local communities, to continue to work towards a shared goal of an adequate fiber intake for all. Good nutrition and simple grains have lain at the heart of the Kellogg Company since its inception. Innovation in digestive wellness is woven through the story of Kellogg foods from the very beginning with Bran Flakes® launched in 1915, followed by All-Bran® one year later. To this day these foods remain a lynch pin in Kellogg’s fiber-rich offering. Kellogg’s plant-based foods are offered in more than 180 countries.

