A researcher sees a patient’s most painful and intimate moments when developing new treatments for cancer. Working assiduously to improve those treatments, some progress is made. Occasionally, there are miracles.
That’s what happened at Tokyo Women’s Medical University in 2015. While conducting safety trials of experimental ultrasound therapy on a 12-year-old dog with a terminal-stage chondrosarcoma — its weakened pelvic bone so swollen the animal couldn’t stand — they were amazed to see the dog walking again shortly after a single treatment.
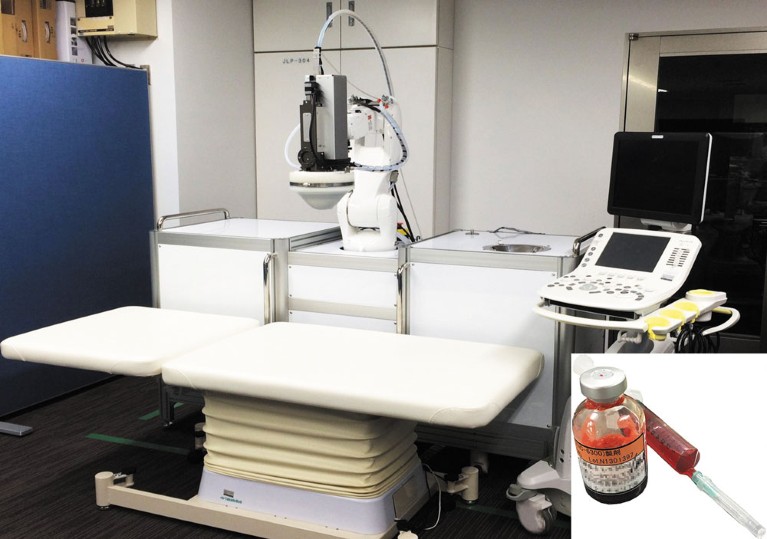
A high-intensity focused ultrasound system, sponsored by Japan Science and Technology Agency; [Inset] a vial of nanocarriers
“It was a completely unexpected result — we were just testing for safety,” says Professor Yoshihiro Muragaki of the university’s Faculty of Advanced Techno-Surgery. “The improvement was very dramatic. The dog couldn’t walk when he arrived. But after a week, he was walking again and could even run steadily on all four legs. CT scans showed the tumour had been reduced by 15%.”
With the animal stable two months after treatment, a second round of sonodynamic therapy was performed, resulting in even more improvement: the dog could excrete again naturally. Follow-up scans four months later showed only a minimal increase in tumour volume.
“This dog survived for more than two years after two treatments,” adds Muragaki. “In human terms, that’s an extra 10 years of survival from terminal bone cancer.”
Another three dogs with inoperable tumours underwent sonodynamic therapy; one had bone cancer, one liver cancer and one prostate cancer and a metastatic lung tumour. All improved after treatment, and in the last dog, the calcified mass inside the prostate tumour disappeared within 49 days and no lung tumour could be detected with radiographic imaging. None of the animals suffered adverse effects during irradiation and no abnormalities were detected in haematological or biochemical tests.
The canine trials were exciting because cancers in dogs are very similar to human cancers — at times, functionally identical. And sonodynamic therapy had already succeeded in in vivo trials on mouse models of colon and pancreatic cancer.
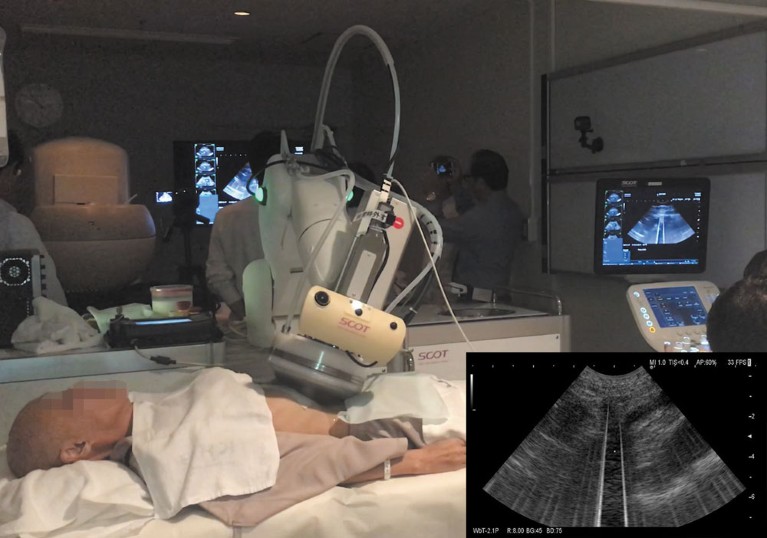
The first in-human trial of sonodynamic therapy for unresectable pancreatic cancer at Tokyo Medical University
Muragaki began exploring high-intensity focused ultrasound (HIFU), along with drugs that help destroy solid tumours, in 2007. His team developed a system consisting of a diagnostic ultrasound probe tailored to locate and tag tumours, coupled with a precision robot HIFU transducer, and specialized software that controls the robot and helps it navigate based on an MRI map of the tumour and live data from the ultrasound probe.
The HIFU transducer itself is novel: a flexible robot arm with six axes of movement, developed by Tohoku University, which fires beams in a specialized pattern called trigger pulses. The pulses activate polymer nanocarriers, or micelles, injected intravenously the day before, which then disgorge their embedded anti-cancer agents, epirubicin or doxorubicin.
“We don’t know the exact mechanism that leads to this dramatic effectiveness,” says Muragaki. “It may be that the focused ultrasound helped the drug work better by destroying the tumour. Or active oxygen was generated by sonodynamic therapy. Or perhaps the ultrasound destroyed the micelle capsule and boosted delivery of the anti-cancer agent in the cancer cell. Or it could be all three.”
Human trials are underway, and early results are encouraging. Researchers believe the potential for sonodynamic therapy, especially in late-stage pancreatic cancer, is extremely attractive: it’s minimally invasive, has few side effects, and requires just half to one-sixth the dose of drug-laden micelles used in chemotherapy, says Muragaki: “There’s no anaesthesia, the patient lays down on a bed, and it takes around 20 or 30 minutes.”
If successful, Muragaki is keen to deploy the treatment in the faculty’s premier project: the Smart Cyber Operating Theater (or SCOT®), which he also leads. Established in 2000 as the Intelligent Operating Theater — an initiative to boost interoperability between the multitude of stand-alone medical devices in modern surgery — it has since spawned into a fully networked, robot-assisted surgical theatre with real-time monitoring and display of a patient’s condition during surgery.

The TWMU team in the Hyper Smart Cyber Operating Theater ® sponsored by Japan Agency for Medical Research and Development
Its latest incarnation, HyperSCOT®, looks like a scene from Star Trek: a room filled with networked equipment spiralling toward a central operating table, encircled by large high-resolution screens. A video feed of the operation is surrounded by live data from various instruments on a single screen, and the physician occupies a ‘surgeon’s cockpit’ — a robot that supports their arms and wrists, making hands steadier and arms tire less easily.
Surgeries continued even as the SCOT® concept evolved: some 1,900 operations were completed (mostly on brain tumours in the precursor theatre to SCOT®), and the results were better than those from conventional theatres. In a study of 525 glioma operations in the theatre, the 5-year survival rate for grade II tumours was 93%, compared to an average of 75% in Japan. In fact, progression-free survival time for grade-II gliomas treated in the precursor theatre was 7.5 years, unmatched by any other hospital.
The surgery department of Tokyo Women’s Medical University Hospital has 296 types of medical devices. The goal is to network all of them into the HyperSCOT®, says Muragaki: “We want to turn the operating theatre into a single medical device.”



 Focal Point on Nanomedicine in Japan
Focal Point on Nanomedicine in Japan