Japan faces a perfect storm: falling birth rates, an ageing population and a stagnant economy – a harbinger of what the rest of the developed world will confront. But those challenges are the catalyst for a determined push to extend working lives and outflank chronic disease, and nanomedicine is central to the effort.
© GiroScience / Alamy Stock Photo
“The challenges facing Japan now will, before long, be problems facing the world,” says Professor Kazunori Kataoka, director-general of the Innovation Center of NanoMedicine (iCONM) and considered a leader of the field. “If Japan is to become a role model in how to deal with a declining birth rate and ageing population, we need a stream of innovations in nanomedicine.”
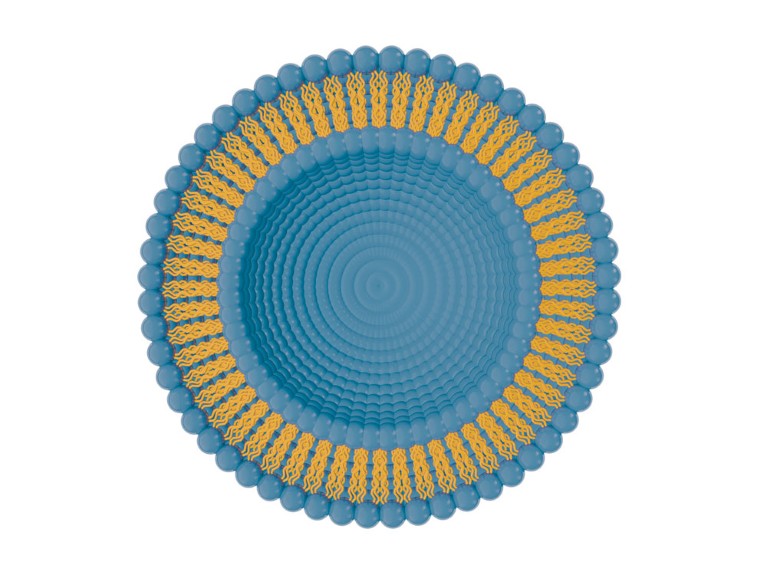
Kataoka is a pioneer — the man who in the 1980s developed the polymer micelle nanocarriers now providing unprecedented precision in the targeted delivery of drugs and genes in the body, especially for anti-cancer drugs that are poorly soluble in water. Ranging from 10 to 100 nanometres and encased in a hydrophilic shells of polyethylene glycol, micelles survive intact for long periods in the blood and reliably accumulate in tumour tissues. Many cancer treatments using them are on the verge of clinical adoption.
“The Japanese have definitely been at the top ranks of research in nanomedicine,” says Professor Cyrille Boyer, co-director of the Australian Centre for Nanomedicine at the University of New South Wales. “They’re famous for their work on polymer micelles, which is an extremely promising area, particularly in cancer treatment.”
Cancer is the second leading cause of death globally, but in Japan it has been number one since 1981. This is partly due to the country’s ageing demographic: most cancer deaths occur in those over 50. Cancer is also expensive to treat, requiring pathology, medical imaging, hospital stays, and often radiation, surgery and home care. Then there’s the hefty price tag of drugs; some, like Opdivo (created by Japan’s Ono Pharmaceutical to treat lung cancer) cost US$22,100 a month. Hence, Japan, which has one of the world’s most efficient national health systems, faces ballooning healthcare costs; US$367 billion in 2015, up 26% in a decade.
The continued ageing of Japanese society will only compound the situation: while 27.3% of Japan’s 127 million people are aged 65 or older, it’s forecast to be closer to 40% by 2065. Even excluding cancer, an older population costs more to keep healthy: already, 38% (or US$139 billion) of the country’s medical expenditure is directed at those 75 or older. This is expected to reach 42%, or US$175 billion, by 2020.
These factors make cancer the target of so much of Japan’s nanomedicine. Many of the treatments under development rely on another Japanese discovery: the enhanced permeability and retention (EPR) effect, in which molecules of certain sizes tend to accumulate more in tumour tissue compared to normal tissue. First described in 1986 by Dr Yasuhiro Matsumura of the National Cancer Center Hospital East and colleagues, it has given rise to a whole new class of cancer-selective drug delivery methods.
EPR has made experimental treatments, such as those involving polymer micelles, much more effective. And while work remains to be done to improve efficacy, especially in understanding tumour vasculature and dynamics, it’s clear EPR is making a major contribution, says Kataoka.
Another Japanese contribution to nanomedicine has been the discovery of green fluorescent protein (GFP) by organic chemist, Dr Osamu Shimomura, which earned him the 2008 Nobel Prize in Chemistry. GFP is an essential tool in nanomedicine, with applications in intracellular thermal sensing and imaging, protein fusions and as transcriptional reporters. It has, in effect, allowed living cells to be used as experimental platforms for nanomedicine research.
While research in nanocarriers is a hot area of global research — not just with polymer micelles, but also various organic/inorganic nanoparticles — Kataoka believes polymer micelles have extraordinary potential.
“I used to think of them as pizza deliverers,” he said. “Then we realized they can respond to cellular microenvironments and change structure. Now I think we can make micelles more like a chef, who can go to your house with nothing, and make pizza. Or anything else.”
Research has established that even small changes in size and shape can dramatically affect the properties of nanoparticles, so precision synthesis is essential to achieve the tightly focused distribution necessary for targeted therapy. In this, Kataoka believes Japan has a major advantage, thanks to its status as a US$300 billion behemoth in chemicals industry.
“Nanomedicine is based on polymer chemistry, where Japan has a big advantage,” he said. “It requires precision polymerization, and we have lot of experience and have made a lot of progress in this field.”


 Focal Point on Nanomedicine in Japan
Focal Point on Nanomedicine in Japan