In 2016, Chiba University and the University of California San Diego (UCSD) launched a US$2 million partnership focusing on the development of vaccines to prevent infectious diseases, allergies and cancers.
The joint initiative builds on more than a decade of successful collaboration between Chiba University and the La Jolla Institute for Allergy and Immunology, located in UCSD’s Science Research Park. Toshinori Nakayama, professor and dean of the Graduate School of Medicine at Chiba University, says that with the School of Medicine’s more than 100 years of history and progress in the field of immunology, the time is ripe to work on the intersection between mucosal immunology and vaccines.
“The mucosal barrier is the body’s first line of defence against external pathogens, and also where allergic reactions occur,” he says. “We’re now bringing all of our data, knowledge and insights together to accelerate the development of preventive medicines and innovative therapeutics.”
He highlights MucoRice-CTB — a new form of cholera vaccine developed by Hiroshi Kiyono and his team, a core member of the Chiba University-UCSD Center for Mucosal Immunology, Allergy and Vaccine (cMAV) — as a shining example of what can be achieved.
“MucoRice has several advantages over existing vaccines: more stability at room temperature, lower risks of contamination and higher effectiveness,” says Nakayama. “We believe this technology will be used for other types of vaccines against emerging and re-emerging diseases as well as other diseases including allergy and cancer.”
An asthmatic lung examined by electron microscopy.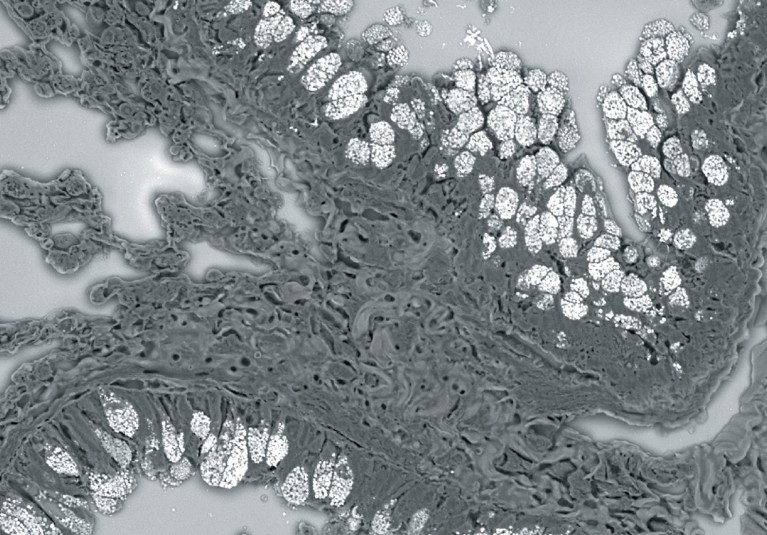
Improving human health
Chiba University researchers are also working to uncover the mechanisms underlying allergic inflammations, and have established treatments such as sublingual immunotherapy for Japanese cedar pollinosis — hay fever caused by pollen released by the endemic tree species Cryptomeria japonica that afflicts millions of people every year.
Drawing on more than 20 years of research on T cell biology, Motoko Kimura at Chiba University’s Department of Immunology is now investigating the immunoregulatory role of the molecule CD69. An anti-CD69 antibody was found to help prevent inflammatory responses related, for example, to asthma, colitis, and arthritis in mouse studies.
“By collaborating with pharmaceutical venture companies, we have established humanized anti-CD69 as well as anti-CD69 ligand (Myl9) antibodies, which we believe will be useful for the treatment of intractable inflammatory diseases,” she says.
Kimura’s research has also identified CD69 as a target for cancer immunotherapy. “Currently, powerful anti-tumour drugs — so-called immune checkpoint inhibitors — are only effective for about 20% of patients, and are not applicable to patients suffering from autoimmune diseases,” she says. “We hope that anti-CD69 antibody treatment could offer new hope to these patients.”
A micrograph showing induced bronchus-associated lymphoid tissue (iBALT) in the lung.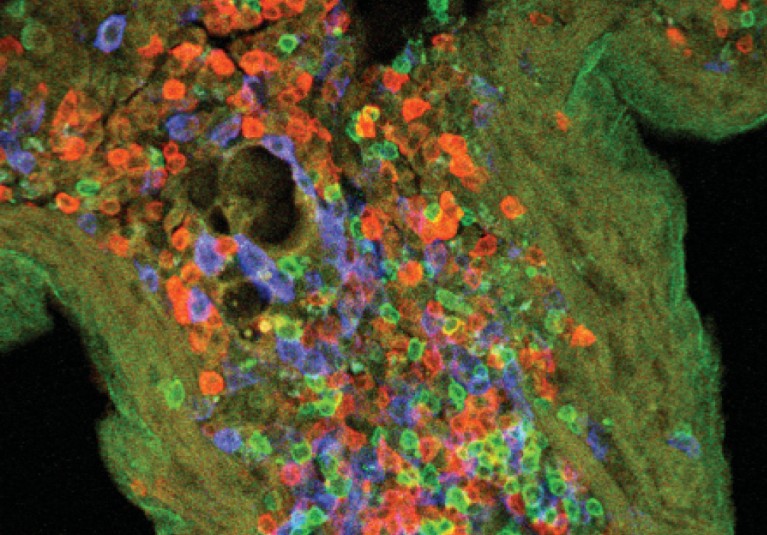
Looking ahead
Nakayama says there are plans to expand the immunology initiative globally, with activities extending to the rest of Asia and Europe. He encourages those who are interested in contributing to the advancement of next-generation vaccines to attend the 4th cMAV Symposium, which will be held at UCSD from 13–15 February 2019.


 Focal Point on Vaccine Research in Asia
Focal Point on Vaccine Research in Asia