A nurse tests a patient’s haemoglobin levels.Credit: Donwilson Odhiambo/SOPA Images/LightRocket via Getty
A one-year medical internship at Nyeri Provincial General Hospital in Kenya led me to think about oncology. I spent a lot of time learning about chemotherapies and monitoring cancers. I enjoyed seeing people get proper treatment, especially when it resulted in better outcomes and quality of life.
I had a good relationship with my father, and one other experience that made me consider oncology was when he died of colorectal carcinoma in 2012, after my internship was over. We had sought therapy, but it was too expensive, and the cancer spread quickly to the liver.
I wondered about the speed of this spread. This led to my interest in the biological mechanisms of the condition. A couple of years after my father died, my friends suggested I apply to do a master’s degree in clinical oncology at Muhimbili University of Health and Allied Sciences in Dar es Salaam, Tanzania.
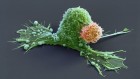
I am now at the Kenyatta University Teaching, Referral and Research Hospital in Nairobi. Working at a research hospital is very important to me. Research has helped us to accumulate extensive knowledge about the biological processes involved in cancer onset, growth and spread. Those discoveries have led to more-effective treatments and prevention strategies. Research in a hospital setting gives you more resources than elsewhere, and you see a lot of patients, which is good for sample sizes in studies.
In a typical week, I meet up with other oncologists and various specialists at least once, usually on Mondays. This team reviews people who are newly diagnosed with the disease. A junior doctor presents the clinical findings, diagnosis and plans for initial treatment suggested by an oncologist. Then a radiologist discusses things such as magnetic resonance imaging (MRI) scans, and pathologists present their findings. On Tuesdays, I usually meet up with the radiation physicist and come up with a plan for radiotherapy.
Hectic schedule
I see some patients on alternate Wednesdays and Thursdays, but Thursdays are my main clinic day — and they can be very hectic. This is when I meet with people newly diagnosed with cancer, and I write down and adjust chemotherapy plans. Thursdays are usually punctuated by phone calls or by questions from young doctors. This means that at the end of a long day, you might have seen just one or two patients. Their families also have a lot of questions, so I end up having long discussions with them: 1–2 hours, instead of the usual 30 minutes.
I’m not currently doing research in Kenya but I am working on several studies with scientists in Rwanda and Uganda. We have done a number of clinical trials involving, for example, people with ‘triple-negative’ breast cancer — in which the cancer cells lack receptors for oestrogen and progesterone and the protein HER2. Without these receptors, the cancer doesn’t respond in the typical way to medications and is harder to treat. We wanted to find out whether people with this cancer have other illnesses that could change the recommended course of treatment.
The better we understand cancer, the more progress we will make in dealing with its human and economic toll.

 Blood vessel growth in benign tumours can illuminate malignant ones
Blood vessel growth in benign tumours can illuminate malignant ones
 Using proteins to test for COVID antibodies
Using proteins to test for COVID antibodies
 Untangling the complex roots of cancer in Brazil
Untangling the complex roots of cancer in Brazil
 Why a private hospital in Mexico City embraces research
Why a private hospital in Mexico City embraces research
 Coordinating research at one of Latin America’s best hospitals
Coordinating research at one of Latin America’s best hospitals