- OUTLOOK
How to improve the diagnosis of prostate cancer
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Rent or buy this article
Prices vary by article type
from$1.95
to$39.95
Prices may be subject to local taxes which are calculated during checkout
Nature 609, S36-S37 (2022)
doi: https://doi.org/10.1038/d41586-022-02858-7
This article is part of Nature Outlook: Prostate cancer, an editorially independent supplement produced with the financial support of third parties. About this content.
References
Ilic, D. et al. BMJ 362, k3519 (2018).
Panigrahi, G. K. et al. Cancer Med. 8, 1110–1123 (2019).
Fredsøe, J. et al. Diagnostics 10, 188 (2020).
Borkowetz, A. et al. Diagnostics 10, 578 (2020).
De Visschere, P. J. L. et al. Eur. Urol. Oncol. 2, 47–76 (2019).

 Researchers take on the challenge of prostate cancer
Researchers take on the challenge of prostate cancer
 Prostate cancer: highlights from research
Prostate cancer: highlights from research
 A better way to biopsy in prostate cancer
A better way to biopsy in prostate cancer
 Metastatic prostate cancer: seeking a fresh chance of recovery
Metastatic prostate cancer: seeking a fresh chance of recovery
 The destructive power of PROTACs could tackle prostate cancer
The destructive power of PROTACs could tackle prostate cancer
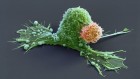
 Could immunotherapy finally break through in prostate cancer?
Could immunotherapy finally break through in prostate cancer?
 Treat the mind, not just the body for prostate cancer
Treat the mind, not just the body for prostate cancer
 Does prostate-cancer treatment place a strain on the heart?
Does prostate-cancer treatment place a strain on the heart?
 Let’s talk about sex: tailoring prostate-cancer care for LGBT+ people
Let’s talk about sex: tailoring prostate-cancer care for LGBT+ people
 Racism and prostate cancer: a multilayered issue
Racism and prostate cancer: a multilayered issue