The Strategic Advisory Group of Experts on Immunization (SAGE) — a team of around 15 public-health physicians, epidemiologists and other specialists — has been making recommendations to the World Health Organization (WHO) about who should receive what vaccines since 1999.
But in early 2020, the group faced its most daunting challenge yet. As the world reeled from overwhelmed health systems, lockdowns and closed schools and businesses, SAGE had to advise the WHO on how its 194 member states should deploy what would initially be a limited supply of COVID-19 vaccines.
Until this point, SAGE had based its recommendations almost exclusively on scientific evidence — immunological and epidemiological data, the results of clinical trials and so on. But with SARS-CoV-2 presenting a more serious threat to global health and stability than any other pathogen in SAGE’s two decades of existence, the advisory body was facing choices more consequential and morally fraught than any it had faced before.
For perhaps the first time in SAGE’s history, ethicists were included in its call for nominees for a working group on vaccines (along with specialists in vaccinology, infectious disease, epidemiology, modelling and public health). What’s more, the working group’s first task was to come up with an ethical framework that would inform and justify subsequent recommendations about which groups around the world should be the first to receive COVID-19 vaccines. Although ethicists had previously been involved in SAGE’s deliberations, ethics was given a much more central role in its work.
We were asked to develop this ethical framework as members of a subgroup of SAGE’s Working Group on COVID-19 Vaccines. The 15 of us in the subgroup had less than 10 weeks to develop a document that we knew might help to determine who in the world would get a potentially life-saving vaccine. What happened in the countless hours we spent annotating shared documents, in video meetings and on phone calls across disparate time zones holds lessons for those trying to better prepare the world for a future pandemic.
Moral goal
Ethical frameworks — a set of moral principles, values or rules — are routinely developed in science, medicine and health policy to guide research and practice, and to make it easier for stakeholders to identify interventions or areas of research that are ethically problematic. In 2017, for instance, the US National Academy of Sciences, Engineering, and Medicine co-produced a report that included seven “general principles for the governance of human genome editing”1.
We drew on this tradition of ethical frameworks to develop a values framework for the allocation and prioritization of COVID-19 vaccination.
In this document, we first articulated the overarching moral goal of the global deployment of COVID-19 vaccines: “to contribute significantly to the equitable protection and promotion of human well-being among all people of the world”. We then laid out six principles to guide the allocation of COVID-19 vaccines within and between countries in the face of limited supply. For each principle, we specified two to three objectives: goals specific to a pandemic. As an example, “protect the continuing functioning of essential services, including health services” was one of three objectives tied to the principle of human well-being.
Finally, alongside the principles and objectives, we flagged various ‘priority-use groups’ to consider for early access to vaccination, from health-care workers and people with co-morbidities to low-income migrant workers and refugees.
Developing this ethical framework was challenging. Members of our subgroup alone represented 11 countries. And although there was no acrimony during the many weeks of discussions, everyone brought a different perspective. Those who had experience in treating children, for example, were especially concerned that we should consider the potential impact of the pandemic on under-18s.

In late 2020, data indicated that elderly people had a much greater risk of dying from COVID-19 than did younger people.Credit: Craig F. Walker/The Boston Globe/Getty
After our subgroup had agreed on a draft framework, it had to be endorsed by the full working group, by the equally culturally and nationally diverse members of the entire SAGE advisory body, as well as by the leadership of the WHO, including director-general Tedros Adhanom Ghebreyesus. The process involved ten meetings of our subgroup and around ten meetings of the working group, deliberations by the entire SAGE team (some of which were open to external observers, such as regional specialists and representatives of non-governmental organizations) and vetting by the WHO’s Working Group on Ethics and COVID-19. (The WHO established a separate Working Group on Ethics and COVID-19 in March 2020 to provide ethical guidance on fast-moving developments during the pandemic, such as mandatory public-health measures and digital vaccine passports.)
Two years of COVID-19 in Africa: lessons for the world
Every word was scrutinized. In the over-arching goal and in one of the six principles, for example, we agreed to refer to ‘human well-being’, not ‘human health’. We were all aware that a focus on well-being would be a departure for SAGE — even for public-health policy in general, which leans heavily on evidence related to people’s health. We chose this wording because, added to the deaths and sickness caused by infection with SARS-CoV-2 were lockdowns, school closures, the need to keep family members separated and other knock-on effects of the pandemic that were upending all aspects of human life.
Likewise, we agreed to specify that minimizing the disruption of education and socio-emotional development in school-aged children was a way to achieve the objective of reducing societal and economic disruption (in turn tied to the principle of human well-being). We hoped that calling out children would encourage SAGE and world leaders taking heed of the WHO’s recommendations to keep considering how vaccines could support children’s lives — even if vaccines that could be administered directly to children were not yet available.
Another source of intense discussion was the principle of reciprocity. A key concern was that the term reciprocity might be exploited so that anyone who had made a contribution to advance the health of others in the pandemic (drug-company scientists or executives, say) could gain priority access to COVID-19 vaccines. By crafting the objective tied to this principle as protecting “those who bear significant additional risks and burdens of COVID-19 to safeguard the welfare of others, including health and other essential workers”, we narrowed down what was meant by the term.
Life or death
Laying out an ethical framework was the first step in a two-part process used by SAGE to develop guidance on which groups to prioritize for COVID-19 vaccination.
In the framework, we had flagged 27 priority groups. We identified another 11 groups in subsequent discussions. The next step was to rank these 38 groups.
To defensibly recommend that homeless people should be vaccinated before vaccine-production workers, say, our subgroup had to integrate the framework’s principles and objectives with whatever evidence was available on specific vaccine products, the probable availability of vaccines and so on.
COVID research: a year of scientific milestones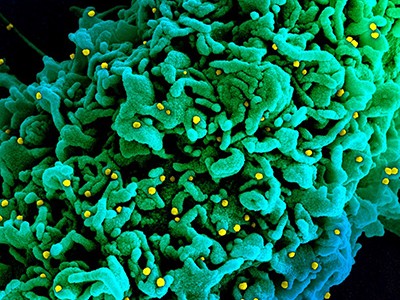
To help with this, we used a modified ‘Delphi method’. After assessing the best available scientific evidence, members independently ranked the priority groups in two rounds. After each round, every member received an anonymized summary of the group’s ratings along with the reasons why those ratings had been selected. They then ranked the groups again in light of the shared information.
The sense of intensity and urgency was perhaps greatest at this point. It was not lost on any of us that — assuming vaccines would protect people from severe disease and death — we were making recommendations that could affect who would live and who would die.
After 11 or so meetings and the use of vetting and input-generation strategies similar to those we had used for the ethical framework, the result was the WHO SAGE Roadmap for Prioritizing Uses of COVID-19 Vaccines in the Context of Limited Supply. This was published on 20 October 2020, before any vaccines were available for emergency use.
The purpose of the road map was to provide governments with ethics-informed, evidence-based recommendations, given the data available at the time. It laid out who to prioritize for COVID-19 vaccination under high, medium or low rates of transmission, and in situations in which vaccine supply constraints meant that only 1–10%, 11–20% or 21–50% of the population could be covered.

Teachers were prioritized to reflect their importance in advancing children’s well-being.Credit: Donwilson Odhiambo/SOPA Images/LightRocket/Getty
More than two years into the pandemic, it’s easy to forget that in late 2020, ideas differed about who should get a COVID-19 vaccine first. For example, that September, a group of prominent scholars proposed that vaccines be administered so as to reduce ‘standard expected years of life lost’2. This would have moved younger adults up the priority list. Likewise, that December, the US Centers for Disease Control and Prevention (CDC) recommended that essential workers be vaccinated before some older adults, in part to try to narrow the disparities in cases and deaths between different socio-economic and ethnic groups across the country3.
The data available at the time included findings that those older than 65 were at least 90 times more likely to die or become seriously ill from COVID-19 than were those aged 18–29. People older than 85 were 630 times more likely to die or become seriously ill. After assessing these data, we decided that the most ethically defensible way to deploy limited supplies of vaccines was to prioritize the direct reduction of death and severe disease. Without evidence on how vaccination might reduce transmission, prioritizing the reduction of death and severe disease also seemed to offer the best way out of lockdowns and other restrictive pandemic policies that were undermining human well-being. (In the values framework and road map documents, we deferred to countries to define ‘older’ and ‘younger’ adults according to age-based risk for their demographic situations, which we knew varied with country and region.)
In the road map, we assigned each priority group to one of three ‘stages’. We assigned health-care workers who were at high to very high risk of acquiring and transmitting infection to the highest priority ranking, for example, in all three epidemiological scenarios and under the different vaccine-supply conditions. This was because of their importance to the continuing functioning of health systems (human well-being) and because of their role in safeguarding the well-being of others (reciprocity). Likewise, teachers and other school staff were assigned to be offered vaccines once availability exceeded 10–20% of a country’s population, because of their importance in advancing the well-being of children.
Priority decisions
So, how valuable was SAGE’s approach?
Although limited in scope, brief surveys administered by the WHO to regional and national vaccine advisory bodies suggest that SAGE’s approach was helpful to many countries when it came to defining — and justifying — their prioritization strategies. (The WHO familiarized national immunization technical advisory groups with the values framework and road map through a series of regional webinars.) Most countries, across the income spectrum, did end up prioritizing initial groups for vaccination in line with SAGE’s recommendations — with health-care workers and ‘older adults’ being first in line. And nearly two years on, SAGE’s ethics- and evidence-centred approach is still shaping policy around the prioritization of COVID-19 vaccination, even in a very different landscape.
The WHO released a major revision of the road map on 21 January 2022. And our work, and that of the other members of SAGE’s working group (and subgroups) on COVID-19 vaccines, is ongoing. In advising on appropriate booster-dose schedules, for example, or the use of COVID-19 vaccines in children and adolescents, we continue to rely on the values framework and road map to orient — and justify — our thinking.
Important to note is that even though global equity features prominently in the values framework, it was not in SAGE’s scope to provide guidance on the allocation of COVID-19 vaccines across countries. It was the mandate of COVAX — a multi-partner initiative in which the WHO was one partner — to work towards global equitable access to COVID-19 vaccines. The greatest failing in the world’s handling of the pandemic — the lack of global equity in the first 20 months in terms of access to medical supplies and vaccines, as well as in the capacity to get doses into arms — needs to be addressed at a more foundational level. The establishment of a pandemic treaty could help to shift norms, for example.
Africa: tackle HIV and COVID-19 together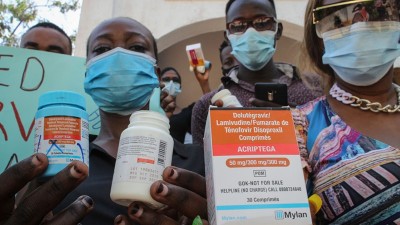
Looking back, we think four features of our effort to integrate ethics into evidence-based recommendations for vaccination were especially valuable.
First, the ethical framework was developed by the people who would go on to deploy it to draft recommendations about which groups to prioritize. This meant that everyone involved had invested in the foundational work, and had a sense of ownership of it. Outside specialists could have been commissioned to do at least the initial drafting of the framework. Doing everything in-house legitimized the central role of ethics in our analysis, and increased people’s comfort levels around ethics reasoning — a new experience for some members of SAGE’s working group and subgroup.
Second, all members of SAGE’s subgroup had some experience in working across disciplines. Two members had expertise in vaccine ethics, even though their primary expertise was in public health or clinical sciences. One of us, whose main expertise was in ethics, had a background in public health and vaccine policy.
Third, continually pressure-testing our ethical reasoning against the best available evidence made our recommendations more credible and defensible. For example, our initial assessment of high mortality in older adults was based on early data from high-income countries only. We continued to critically re-examine this assumption as data emerged from lower-income countries.
Last, we were lucky in the mix of people we had. More didactic or difficult personalities in our group could have stalled our efforts.
There are also aspects of the process that could be improved.
In the first iteration of the road map, we aimed for a level of ethical precision that turned out to be impractical. For instance, we put health-care workers at high to very high risk of infection in a separate category from other health-care workers. But overly complicated or prescriptive prioritization schema are difficult to implement. In fact, some countries, such as the United Kingdom, prioritized vaccination of people who were not health-care workers mainly on the basis of age. To provide an approach that could be more easily implemented at the national level, the 2022 updated road map includes fewer priority groups and describes them more simply.
Also, we were as consultative as feasible given the time constraints. But more time would have allowed for more in-depth feedback from regional and national vaccine policy bodies. It would also have allowed for the inclusion of an even greater diversity of stakeholders, and could have enabled us to tackle more issues — such as the challenges around people’s acceptance of vaccines. It is likely that some attempts to develop within-country vaccine-allocation ethics frameworks (with an overlapping timeline) also faced limitations in securing in-depth feedback because of time constraints.
To better prepare for the next major outbreak, we urge a broad range of stakeholders, from public-policy leaders to researchers to advocates for diverse groups, to engage now in the ethics of vaccine policy — be it in globally or nationally convened committees, conferences, journals or the media.
Ethics and evidence
Many challenging policy decisions around the use of COVID-19 vaccines remain. What part should booster doses or variant-specific vaccines play as the pandemic continues? How should questions around value for money affect the expansion of COVID-19 vaccination in low- and middle-income settings with many competing health needs and more constraints on public financing?
As crucial as scientific data are to addressing these issues, embedded in them are questions about values. Policymakers cannot make decisions about what should be done in these scenarios on the basis of science alone. When policymakers do not acknowledge that ethical reasoning is being used in combination with scientific evidence, the result is often a disconnect between the science and the policy — which can in turn undermine public trust.
The SAGE approach — still very much in development — offers one model for how to integrate ethics with evidence.


 Two years of COVID-19 in Africa: lessons for the world
Two years of COVID-19 in Africa: lessons for the world
 Africa: tackle HIV and COVID-19 together
Africa: tackle HIV and COVID-19 together
 COVID research: a year of scientific milestones
COVID research: a year of scientific milestones






