Last September, more than 100 governments attending US President Joe Biden’s virtual Global COVID-19 Summit committed to vaccinating at least 70% of the population in every country by September 2022. Using national vaccination rates from mid-February, we estimate1 that nearly 100 countries will fall short of that objective.
Those missing the target include four out of five African nations, and most countries in Central America and the Middle East. In low-income nations, only one in ten people is fully vaccinated. Seventeen high-income nations, including Poland and Oman, are not on track to reach this goal either. At its current pace, Slovakia will not vaccinate 70% of its population until May 2026.
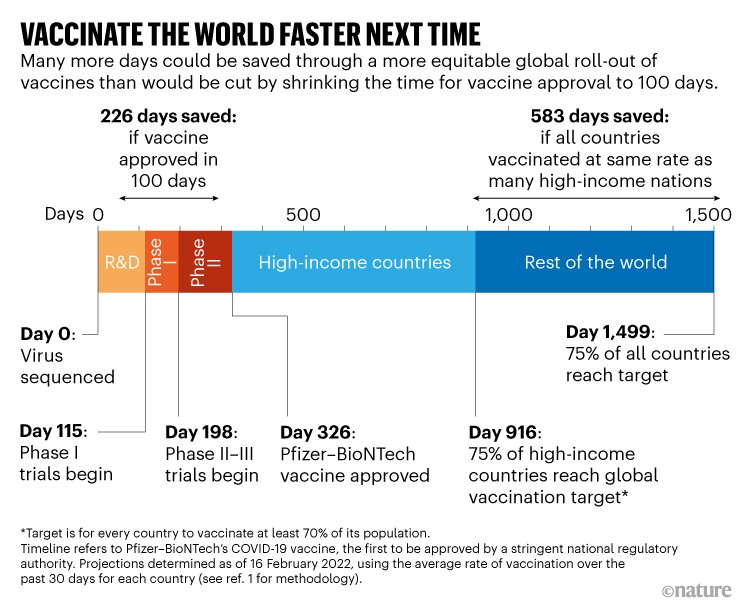
In fact, at current vaccination rates, it will take until 15 July for 75% of high-income nations to fully vaccinate 70% of their populations. That’s 590 days (more than 1.5 years) after the UK government first authorized a COVID-19 vaccine for general use (see ‘Vaccinate the world faster next time’). Getting this proportion of people fully vaccinated in three-quarters of all countries will take almost double that time — 1,173 days, or more than three years1.
These delays translate into millions of avoidable hospitalizations and deaths. They are mainly the result of inadequate global supplies of vaccine doses, and the challenges of planning, resourcing and implementing vast vaccination programmes in countries with already strained health systems.
Source: T. J. Bollyky et al.
The US White House is convening another global COVID-19 summit in the near future. To limit further surges in hospitalizations and deaths in the current pandemic — and to prepare better for a potentially even deadlier one — attendees and world leaders must establish long-lasting adult-immunization infrastructure and vaccine-manufacturing capacity in their own countries. They must prioritize vulnerable groups for COVID-19 vaccination. And they must take steps to stem the spread of misinformation and disinformation around vaccination.
For many low- and middle-income countries, all this can be achieved only with adequate support from wealthy nations.
The 100-day goal
Over the past six months, the United Kingdom2, the United States3 and the European Union (see go.nature.com/3jrxudk) have all launched various initiatives to boost vaccine production. These aim to reduce the research and development time needed to create vaccines against future pandemic threats to as little as 100 days from the publication of a virus’s genetic sequence. Researchers are already trying to develop prototype vaccines for known pathogens in viral families deemed most likely to cause the next pandemic.
Such initiatives are crucial in preparing for future pandemics. On 2 December 2020, the UK Medicines and Healthcare products Regulatory Agency became the first stringent regulator to authorize a COVID-19 vaccine, namely that made by Pfizer and BioNTech. Developing vaccines in 100 days would have produced a publicly accessible vaccine 226 days sooner — a period in which 1.4 million COVID-19 deaths were recorded.
Yet, having faster ways to develop vaccines will not help unless world leaders also undertake the measures necessary to achieve much faster rates of vaccination globally.
COVID-19: talk of ‘vaccine hesitancy’ lets governments off the hook
As of February, COVAX, the multilateral COVID-19 vaccine initiative, had distributed 1.3 billion doses of vaccines to 144 countries and territories. But three-quarters of those doses were distributed in the past four months, almost two years into the pandemic. Millions of vaccine doses, donated through COVAX and bilaterally, are going to waste because they are arriving in low- and middle-income countries too late for them to be used before they expire. The initial priority for COVAX was procuring and shipping vaccines, but many recipient governments lack resources to get the shots into arms. They do not have the workforce, information systems or cold-chain infrastructure and supply logistics to plan, finance and deploy massive and effective vaccination campaigns.
Forty-four of the African Union’s 55 member states don’t have enough fridges, freezers and other cold-storage infrastructure needed to distribute the Pfizer–BioNTech vaccine. This is according to a report last month by the Reuters news agency, which cited a January survey by the United Nations children’s charity UNICEF (see go.nature.com/3jpivpm). In fact, in February, the Africa Centres for Disease Control (Africa CDC) reportedly requested that vaccine donations be delayed or staggered because countries need more time and resources to deploy them. Meanwhile, COVAX has reportedly run out of money to help recipient countries with vaccine deployment, with no new funding sent since January4. Because of this and other challenges, 34% of the current supply of COVID-19 vaccines has yet to be administered across the African continent (see go.nature.com/3bgrhxy).
Such bottlenecks are compounded by a lack of consideration for the needs of low- and middle-income countries when it comes to vaccine authorization processes.
In wealthy nations, regulators such as the US Food and Drug Administration (FDA) and the European Union’s European Medicines Agency have been slow to authorize vaccines that would be easier to administer in low-infrastructure settings. The protein-based vaccine made by Novavax, for example, might not be needed in wealthier countries where governments have purchased more than enough doses of other vaccines for their population. But Novavax does not require such cold storage as the Pfizer–BioNTech shot, and could be valuable in Africa. Likewise, the lack of FDA approval for the vaccine developed by the University of Oxford, UK, and AstraZeneca has reportedly undermined the willingness of other nations to take donations of this vaccine.
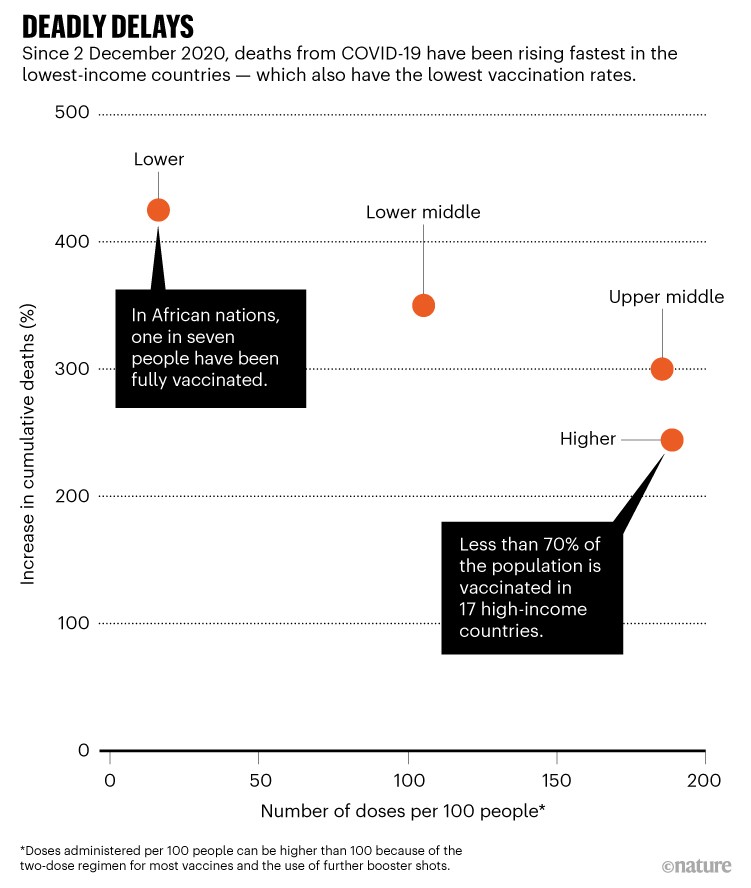
All these delays in vaccination have deadly consequences. In general, deaths from COVID-19 have been rising fastest in the countries and regions that have the lowest vaccination rates (see ‘Deadly delays’).
Source: Our World In Data
Four priorities
Addressing the outstanding gaps in global vaccination coverage will require major investments across four domains — especially in the world’s poorest regions.
Prioritizing vulnerable groups. That all nations have the same goal, of vaccinating 70% of their populations, remains important as a matter of global equity. But the public-health rationale behind this goal has shifted because stopping transmission of SARS-CoV-2 through a high vaccination rate alone is no longer feasible.
COVID-19 vaccines offer limited protection against infection by BA.1 and BA.2, the most common Omicron variants5. But vaccines still significantly reduce the probability that a person will be hospitalized or die as a result of infection. New York state reported that, in the latest Omicron wave, fully vaccinated individuals had a 90.1–95.9% lower chance of being hospitalized with COVID-19, compared with unvaccinated individuals (see go.nature.com/37tbshq).
Given this, prioritizing the most vulnerable groups for full vaccination is currently the best way to limit further waves of hospitalizations and deaths.
Indeed, the costs of not doing so were demonstrated by the recent surge in cases and deaths in Hong Kong. On average, 284 people were dying there each day between 6 and 13 March. That’s a death rate of 38 per million people per day — the highest recorded globally in the pandemic6.
Two years of COVID-19 in Africa: lessons for the world
Although 65% of the population was fully vaccinated by 9 February, when Hong Kong’s Omicron wave was escalating, only 33% of residents aged above 80 had received one dose — seemingly because of a mixture of complacency stemming from the region’s zero-COVID policy, and insufficient effort by public-health officials to reach nursing homes.
Worldwide, a focus on getting as many shots in arms as possible and boosting population vaccination coverage has tended to leave high-risk individuals unprotected. In low-resource settings, the limited human resources and lack of patient-information systems makes it even harder for health officials to identify and prioritize vulnerable and hard-to-reach individuals.
As we enter the third year of the pandemic, much more must be done in those settings to prioritize the most vulnerable — including health workers, those who are immunocompromised and older people, as well as disenfranchised populations.
To prioritize the vaccination of vulnerable groups, the World Health Organization (WHO), agencies such as UNICEF and the non-profit aid agency CARE, together with nations that provide aid, technical assistance and vaccines, could work with health officials in low- and middle-income countries. Over the past year, for example, the Ugandan government has worked with the US Centers for Disease Control and Prevention to establish centralized systems for tracking people by age and by medical and vaccination status, and to boost vaccine uptake in priority groups. This has been done in part through the use of clinics and infrastructure set up by the US President’s Emergency Plan for AIDS Relief. In Mali, for example, more than 800 health workers were recruited and trained in the past year to conduct community surveys, to improve understanding of local attitudes towards COVID-19 vaccines, and to identify community-specific barriers to vaccinating vulnerable groups.
To be most effective, however, partnerships with local leaders and communication campaigns must be established in advance of a crisis. Investments to help to address the COVID-19 pandemic should result in lasting infrastructure that can be used to address future global health threats.

A community leader and health-care workers talk to schoolchildren in a remote part of the Peruvian Amazon about COVID-19.Credit: Sebastian Castaneda/Reuters
Adult immunization infrastructure. The infrastructure needed for COVID-19 vaccination is different from that for immunizing newborns and children, which global health programmes have supported for decades. For the latter, health-care workers and immunization initiatives can largely focus on providing information and shots in schools and paediatric clinics, or as part of prenatal care programmes. But in the case of COVID-19 vaccines, all age groups (usually above the age of five) must be reached across vastly diverse settings.
As such, the COVID-19 pandemic offers a rare opportunity to build on existing health systems to improve adult immunization infrastructure across low-income settings.
More people, from medical students to pharmacists, could be trained and mobilized to help with community outreach and vaccine administration in local clinics. Mobile vaccination clinics could be set up to reach people where they live, work or socialize. In addition, community-specific education and messaging campaigns could be launched. In Zambia, for example, the US Agency for International Development (USAID) has supported health workers’ door-to-door community outreach and COVID-19 vaccination events at stadiums and hair salons.
How COVID vaccines shaped 2021 in eight powerful charts
Building lasting adult immunization programmes in poorer nations would help to support any future need to provide boosters against COVID-19 variants, as well as bolster the response to a future pandemic and potential vaccination campaigns against other diseases, such as yellow fever and tuberculosis. Brazil, which has otherwise struggled in its pandemic response, achieved high rates of COVID-19 vaccination because of its well-established national immunization programme for children and adults, which is embedded in the primary health-care system.
Yet, to achieve all this, the United States, along with other governments and donors, must provide poorer countries with more financial and other support.
Just $150 million of the $3.5 billion that COVAX received in 2020 was for vaccine delivery (see go.nature.com/36jytcu). And according to Seth Berkley, chief executive of Gavi, the Vaccine Alliance, the international funding for getting shots into arms has run out. Last month, the White House asked the US Congress for $5 billion to support global vaccination. This amount — which has yet to be provided — is roughly one-quarter of the $19.5 billion that USAID originally requested to accelerate the uptake of COVID-19 vaccines globally.
Vaccine misinformation and disinformation. Globally, governments have underestimated the extent to which rampant disinformation impedes vaccination campaigns.
Targeted approaches, such as those involving community leaders discussing the benefits and risks of COVID-19 vaccination, can help to improve uptake in groups that have historical distrust in government interventions. In the United States, community-based vaccination efforts within the Navajo Nation helped to vaccinate adults at a rate that exceeded the US national average as of April last year (see go.nature.com/3irgecf). But evidence-based approaches with much broader reach will be crucial — both to address this problem at scale in the COVID-19 pandemic, and to ensure that governments and health officials are better equipped to deal with misinformation and disinformation in a future pandemic.
Some governments, such as the United States, are better placed than others to combat vaccine misinformation and disinformation. A 2021 report by the non-profit Center for Countering Digital Hate (CCDH) determined that more than two-thirds of the COVID-19 misinformation and disinformation online could be attributed to 12 individuals on social media7. Noting insufficient action by social-media companies to remove these people from their platforms, the CCDH has called on the US government to overhaul Section 230 of the US Communications Decency Act of 1996. This protects social-media companies from liability stemming from harms caused by content posted by users.
Until social-media firms or the US government take action to address disinformation at its source, social media will need to be continually monitored for untruths about vaccines, and evidence-based counter-narratives developed. Countries might need to do this for themselves, but given the common sources of vaccine falsehoods, a global monitoring effort could help.

A person with COVID-19 is taken to a hospital in Hong Kong in February 2022 as the region deals with a severe wave of infections.Credit: Emmanuel Serna/SOPA Images/LightRocket/Getty
The WHO, which warned of the existence of an ‘infodemic’ around COVID-19 as early as February 2020, might be able to help monitor and respond to some of the COVID-19 vaccine misinformation and disinformation that continue to arise. For instance, it could disseminate counter-information — in ways that capture enough people’s attention — to essentially drown out the false claims. But the WHO will need extra financial and technical resources to better fulfil this role.
Global capacity should also be expanded to monitor vaccine- and disease-related misinformation and disinformation; to understand what makes certain information spread so widely; and to develop and disseminate effective evidence-based counter-narratives.
Before the broad authorization of COVID-19 vaccines, the CCDH monitored anti-vaccination groups online and identified the ‘playbook’ these groups were planning to use to undermine vaccination efforts8. Understanding the strategies of these groups is crucial to developing campaigns that debunk false information.
Regional vaccine manufacturing. Wealthy nations should provide greater financial and technical support to create vaccine-manufacturing hubs in underserved regions, to ensure earlier and more equitable global access to vaccines in future pandemics.
There have been welcome steps in this direction in Africa. The continent is the world’s most underserved, importing 99% of the vaccines its populations use (see go.nature.com/36wcbre). Unsurprisingly, it also has the lowest COVID-19 vaccination rate in the world: just one in seven people there is fully vaccinated (see go.nature.com/38kusu4).
But in April 2021, Africa CDC launched Partnerships for African Vaccine Manufacturing (see go.nature.com/3wg2ysd). This framework aims to attract international investment, promote technology transfer, support local R&D and improve regional regulatory capacity. The aim is that, by 2040, 60% of all vaccines used on the continent will be produced there.
In recent months, the US International Development Finance Corporation (a development finance institution), the African Development Bank and the European Commission have promised financial support for vaccine manufacturing in Africa.
Let Africa into the market for COVID-19 diagnostics
What’s more, in November 2020 the US-based company Johnson & Johnson signed a deal for ‘fill-and-finish’ manufacturing of its viral-vector COVID-19 vaccine in South Africa (in which vials are filled with vaccine and packaged for distribution). Pfizer and BioNTech signed an agreement in July 2021 to do the same for their vaccine. And in October 2021, the US-based biotechnology company Moderna announced plans to build a production facility for 500 million annual doses of messenger RNA (mRNA) vaccines in Africa, which it later indicated will be located in Kenya.
In addition to this, over the past year, the governments of around ten African nations — including Algeria, Egypt, Rwanda, Côte d’Ivoire, Ghana and Nigeria — have either signed agreements to engage in manufacturing COVID-19 mRNA vaccines, or formally expressed an interest in doing so.
An emerging risk is that vaccine manufacturing efforts in Africa will become too heavily focused on a single platform — mRNA technology. The only approved mRNA vaccines so far are those for COVID-19; it is not yet clear whether mRNA vaccines will prove useful against diseases that must be tackled as a matter of routine in Africa, such as malaria and tuberculosis. Ultimately, however, decisions over the prioritization of manufacturing capacity and vaccine platforms are for governments in Africa and other underserved regions to make.
Also, so far, the partnerships involving the major COVID-19 vaccine manufacturers, such as Moderna, have sidestepped licensing their technology to third parties through the mRNA vaccine technology transfer hub. The hub was established by the WHO and other partners in June 2021 in Cape Town, South Africa, specifically to try to encourage licensing and the sharing of technology and technical know-how with local vaccine producers. However, Afrigen Biologics, a South African company, is working with the hub to develop a vaccine based on the Moderna vaccine.
The World Bank can help to support vaccine manufacturing in Africa and elsewhere by creating mechanisms to mobilize surge finance in future pandemics. It could also work with regional entities, such as the Africa CDC, to bolster pooled-procurement mechanisms such as the African Vaccine Acquisition Trust, a centralized vaccine-purchasing agent that acts on behalf of the African Union.
Governments should also support efforts at the World Trade Organization to limit or eliminate the use of export restrictions on vaccines and other essential medical supplies during pandemics.
Lastly, the governments of wealthy countries and the academic and philanthropic funders of vaccine research and development can include provisions in their licensing agreements and guidelines to require or encourage the transfer of pandemic-relevant technology to qualified producers in underserved regions. Such funders can also work with recipient nations to provide training, perhaps through exchange programmes with vaccine manufacturers overseas, to help ensure that production meets international regulatory standards.
Many movies and novels about deadly disease outbreaks end the same way: with people lining up gratefully to receive a cure or vaccine that scientists have raced to discover. The response to COVID-19 has lost that plot. But is not too late to change the narrative and ensure that global vaccination efforts better match the remarkable achievement of vaccine science.


 Two years of COVID-19 in Africa: lessons for the world
Two years of COVID-19 in Africa: lessons for the world
 Let Africa into the market for COVID-19 diagnostics
Let Africa into the market for COVID-19 diagnostics
 COVID-19: talk of ‘vaccine hesitancy’ lets governments off the hook
COVID-19: talk of ‘vaccine hesitancy’ lets governments off the hook
 How COVID vaccines shaped 2021 in eight powerful charts
How COVID vaccines shaped 2021 in eight powerful charts








