p53 the VIP
The p53 protein is involved in a dizzying array of healthy physiological functions. In many cases, p53 controls these functions by regulating gene expression. p53 directly regulates more than 300 genes with many more indirectly affected1.

Infographic: Lucy Reading-Ikkanda
Centre of attention
The gene that produces p53 (known as TP53) is the most well-studied gene in the human genome, having been cited in more than 10,000 papers since its discovery in 19792.

Source: NCBI-NLM as of 25 January 2022; Infographic: Lucy Reading-Ikkanda
A healthy function
Healthy cells express low levels of p53. The protein is normally trapped in an inhibited state, and these inactive p53 molecules are swiftly broken down. Inactive p53 molecules have an average half-life of just nine minutes3.

Infographic: Lucy Reading-Ikkanda
A regulatory protein called MDM2 keeps p53 in its inactive state. Under normal conditions, MDM2 adds chemical modifications to p53 that mark it for destruction by the cell.

Infographic: Lucy Reading-Ikkanda
Various cellular stressors can cause MDM2 to separate from p53. When this happens, p53 is shuttled from the cytoplasm into the nucleus. Many of these stress triggers are directly linked to cancer.

Infographic: Lucy Reading-Ikkanda
Inside the nucleus, four molecules of p53 assemble into a tetramer that binds to specific response-element sequences in DNA.

Infographic: Lucy Reading-Ikkanda
The target genes can produce a range of responses, depending on the severity of the stress. For mild stress, p53 might put cell division on hold while it triggers DNA repair, or tunes cellular metabolic activity. For severe stress, p53 can put cells into a state of permanent growth arrest or trigger cell death through apoptosis.

Infographic: Lucy Reading-Ikkanda
Broken or blocked
The function of p53 can be lost owing to mutations in the TP53 gene, or because of the dysfunction of proteins that regulate p53. In either case, these problems give cancer the green light to progress.
Tumours with mutant p53. The TP53 gene is mutated in more than 50% of tumours4. Around 80% of p53 mutations affect amino acids in the protein’s DBD, causing it to misfold and also interfering with the recognition of target genes4. Even one mutated copy of TP53 can fuel tumour formation, given that a defective p53 protein combined with other, normal p53 proteins will form a non-functional tetramer. Some studies suggest that mutant p53 also inflicts damage by accumulating as aggregates of misfolded proteins5.

Infographic: Lucy Reading-Ikkanda
Tumours with wild-type p53. Even if TP53 is not mutated, p53 function can still be disrupted. For example, some tumours produce excessive MDM2 that keeps p53 trapped in an inactive state.

Infographic: Lucy Reading-Ikkanda
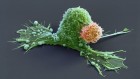
Cancer set loose
Loss of p53 function can promote tumorigenesis and cancer progression in several ways.

Infographic: Lucy Reading-Ikkanda
A chance of treatment
Even after 40 years of research, clinicians still lack drugs that can specifically target tumours with p53 dysfunction. But several promising therapeutic strategies are now undergoing trials.
Tumours with mutant p53. Some small-molecule drugs can bind mutant p53 in a way that restores normal folding. Several such drugs are now in preclinical or early-stage clinical development6. However, this approach requires therapy to be tailored to each patient’s particular TP53 mutation.

Infographic: Lucy Reading-Ikkanda
Tumours with wild-type p53. Drugs that block MDM2’s ability to inhibit p53 might offer a solution for tumours that produce an excess of MDM27. Multiple companies currently have such candidate drugs in clinical trials.

Infographic: Lucy Reading-Ikkanda
Potent partners
The p53-oriented drugs tested so far have shown minimal or modest efficacy on their own. But by helping to normalize p53 function, these drugs could be used in combination with existing therapeutic strategies to give them a boost.
Apoptosis inducers. There are multiple proteins that tumour cells can exploit to inhibit cell death. Restoring p53 function drives the degradation of one of these, known as MCL-1. Combining this treatment with drugs that knock out similar proteins, such as BCL-2, might therefore promote apoptosis more effectively than either treatment alone.
Immune-cell activators. The loss of p53 function puts tumours into an immunosuppressed state. Restoring normal function could prime tumours to respond to drugs such as the checkpoint inhibitor pembrolizumab.

 p53: an anticancer protein’s chequered past and promising future
p53: an anticancer protein’s chequered past and promising future
 Video: Guardian of the genome
Video: Guardian of the genome