People in Mombasa, Kenya, hold empty boxes of antiretrovirals in an April protest over drug shortages caused by the COVID-19 pandemic.Credit: AP/Shutterstock
As scientists and clinical practitioners working in hospitals and laboratories across South Africa, we’ve seen at first hand the devastation that COVID-19 has brought to the country. Many of our colleagues (including leading scientists and health-care professionals) have died. We have also seen how much harder it has become for people with HIV to get treatment and monitoring, which has meant more people being admitted to hospital with serious illnesses such as tuberculosis and cryptococcal meningitis.
As the world shifts gear in the COVID-19 pandemic — from tackling the immediate crisis to a long-term public-health response — we urge governments, health ministries, researchers and other stakeholders worldwide to devote more of their resources and attention to the interactions between COVID-19 and HIV.
Various studies from before the rollout of COVID-19 vaccines show that people with HIV are 30–50% more likely to die from COVID-19. What’s more, a failure to tackle the pandemic with sufficient urgency in countries with high rates of uncontrolled advanced HIV could lead to the emergence of variants of the coronavirus SARS-CoV-2 that spread more easily between people or render the vaccines less effective. Conversely, both diseases could be curbed more effectively if they are tackled simultaneously, with public-health responses strengthened by the lessons learnt from both.
Risk analysis
In 2020, the World Health Organization (WHO) created a platform for standardized clinical data obtained from people with suspected or confirmed COVID-19. A preliminary analysis of these data from 37 countries (most of which come from South Africa) revealed that, controlling for other factors, people with HIV were 30% more likely to die from COVID-19 among those hospitalized with the disease1.
In a more detailed analysis2 of hospitalized cases in South Africa, only people with HIV at an advanced stage were more likely to die from COVID-19. People in this group are severely immunocompromised: individuals have a blood count of fewer than 200 CD4 T cells per microlitre, compared with 500–1,500 cells per microlitre in people without HIV. (CD4 T cells are white blood cells crucial for fighting infection.) In a population-based analysis of around 3.5 million people from the Western Cape Province of South Africa (around 500,000 of whom were HIV-positive), people with HIV were twice as likely to die from COVID-193. But for those with uncontrolled or advanced HIV, the risk of dying from COVID‑19 was almost four times higher3.
Other reports over the past year from various countries indicate that people with weakened immune systems can be infected with SARS-CoV-2 for several weeks or months. (By contrast, those who are otherwise healthy take, on average, around two weeks to clear an infection.) Such prolonged infections have mainly been documented in people receiving cancer chemotherapy and other immunosuppressive agents. But they have also been seen in people with advanced uncontrolled HIV.

A person living with HIV (right) talks to a worker at a mobile clinic in Johannesburg, South Africa, during the COVID-19 pandemic.Credit: Bram Janssen/AP/Shutterstock
Some researchers have proposed that prolonged infection could explain the emergence of SARS-CoV-2 ‘variants of concern’ (VOCs)4. Such variants are more transmissible than the originally identified SARS-CoV-2, or are able to partially evade the immune responses that arise from infection or vaccination. We described a case from South Africa in June in which SARS‑CoV-2 persisted in a person with advanced uncontrolled HIV for more than six months5.Repeated genomic sequencing revealed significant step changes in the evolution of SARS-CoV-2, and some of the variants emerging had similar mutations to those observed in three of the VOCs.
In short, it is plausible that a prolonged COVID-19 infection in someone who is immunocompromised could lead to the emergence of a variant that is more transmissible even than the Delta variant, or that renders current COVID-19 vaccines less effective.
HIV crisis
Sub-Saharan Africa is home to two out of every three people living with HIV worldwide. Last year, 19.5 million people in sub-Saharan Africa received antiretroviral therapy, a cocktail of drugs that stop HIV from making copies of itself and so lessen the damage the virus causes to the immune system. This is up from 12.1 million people 5 years ago. The increase is largely thanks to a stronger commitment by African governments to tackle the HIV crisis; agreements with antiretroviral-therapy producers to reduce prices; and more funds provided by organizations such as the US President’s Emergency Plan for AIDS Relief (PEPFAR) and the Global Fund to Fight AIDS, Tuberculosis and Malaria.
COVID vaccines to reach poorest countries in 2023 — despite recent pledges
Nevertheless, 8 million people with HIV in sub-Saharan Africa (around 21% of the 37.7 million people affected worldwide) are not receiving effective antiretroviral therapy. Some people have difficulty accessing clinics to obtain treatment. Others might not have been diagnosed. Yet others might be unaware of the testing and treatment options available, or resist contact with health-care providers because they fear stigmatization, among other reasons.
What’s more, the COVID-19 pandemic is continuing to cause significant disruption to HIV treatment and prevention programmes.
Part of the problem is strained health-care systems. More than 1,300 health-care workers died from COVID-19 between March 2020 and August 2021 in South Africa alone. Thousands more could leave the profession because of the impact of COVID-19 on their physical and mental health, according to a report by the International Council of Nurses. Overseas funding for HIV has also declined. For instance, the UK government slashed international aid spending this year, leading to funding cuts of more than 80% for key organizations involved in the global response to HIV, including the Joint United Nations Programme on HIV/AIDS (UNAIDS).
Key testing and prevention services declined in 13 countries supported by the Global Fund between 2019 and 2020. Of these, 12 are in Africa. Compared with 2019, HIV testing, for instance, dropped by 22%; voluntary medical male circumcision, which reduces female-to-male sexual transmission of HIV by 60%, dropped by 27%; and the number of mothers receiving medicine to prevent the transmission of HIV to their babies dropped by 4.5%6.
Meanwhile, Africa is being completely left behind as COVID-19 diagnostics, therapeutics and vaccines are deployed throughout much of the rest of the world. By mid-November, more than 40% of people globally had been fully vaccinated. In Africa, it was less than 7% (see ‘Left behind’). In Africa, as elsewhere, older age groups are being prioritized for vaccination, as is appropriate. But this means further delays to vaccinating Africa’s main immunocompromised population. Around 80% of people with HIV across the continent are under 50 years old7.
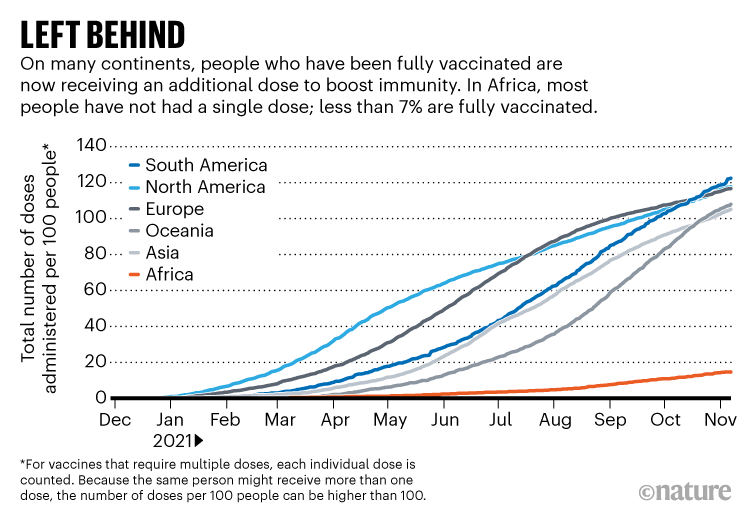
Source: Our World In Data
The initial aim of COVAX, an initiative launched in April 2020 by various groups, including the WHO, to distribute vaccines to low- and middle-income countries, was to make two billion vaccine doses available by the end of 2021. By mid-November, in large part because of donor countries’ failure to deliver on their commitments, only 507 million doses had been delivered.
All these factors together make sub-Saharan Africa especially vulnerable to continued and potentially worsening devastation from COVID-19 and HIV. They will also negatively affect the rest of Africa and the wider world.
Two birds, one stone
We urge stakeholders to commit to four goals.
Vaccinate Africa. For people living with HIV, protection from COVID-19 requires a renewed commitment to vaccine equity between countries. This must come from high-income nations and multilateral initiatives such as COVAX8. Over and above the ethical arguments to address vaccine nationalism and reduce deaths globally, the available data strongly indicate that vaccinating people in Africa will help to reduce transmission rates globally, limit the emergence of new variants and accelerate global control of the pandemic9.
Prioritize research. Several gaps in knowledge around the interaction of COVID-19 and HIV urgently need addressing to inform the long-term public-health response.
More clinical and basic studies could reveal whether prolonged SARS-CoV-2 infections are routine in people with advanced uncontrolled HIV or extremely rare — and whether such infections still occur after people have been vaccinated. Studying the interaction between COVID-19 and HIV must not detract from promptly providing individuals with proper care — in particular, antiretroviral therapies, or new types of antiretroviral treatment if previous ones have not worked.
Victories against AIDS have lessons for COVID-19
Although COVID-19 vaccines have been shown to be safe in people living with HIV, there are some uncertainties when it comes to COVID-19 vaccination strategies.
Overall, people living with HIV represent less than 1% of the participants in the phase III COVID-19 vaccine trials conducted by Pfizer–BioNTech, Moderna, AstraZeneca and Johnson & Johnson. (These have all reported safety and efficacy results, but participant follow-up is ongoing.) In fact, our own investigation found that, for some of the vaccines now being rolled out in Africa (such as Sinopharm, Sinovac and Sputnik), people living with HIV were excluded from the phase III trials.
Individuals on antiretroviral therapy who have well-controlled HIV seem to have immune responses to COVID-19 vaccination that are similar to those of people without HIV10,11. But several observational studies suggest that immune responses to COVID-19 vaccination might be blunted in people with low CD4 T-cell counts12.This is consistent with what we know about how the immune systems of people living with HIV respond to other vaccines13.
Clinical-trial data suggest that an additional COVID-19 vaccine dose might enhance the immune response in other immunocompromised groups14. These include people who have had an organ transplant and are receiving treatment to suppress their immune systems.
International guidelines, such as those from the British HIV Association and the US Centers for Disease Control and Prevention, already recommend that health-care providers give an additional dose to people with advanced uncontrolled HIV. But governments of low- and middle-income countries might well demand stronger scientific evidence before they fund the distribution of additional doses to immunocompromised populations. Also, it is not yet clear which subgroups of people living with HIV might benefit, or what the optimal timing of the additional vaccine dose might be, particularly in people starting or restarting antiretroviral therapy.
African nations missing from coronavirus trials
As vaccines are rolled out in countries that have high rates of HIV, governments, with leadership from organizations such as the WHO and the Africa Centres for Disease Control and Prevention, must support surveillance and monitoring systems for evaluating the effectiveness of COVID-19 vaccines in people living with HIV.
Maintain HIV services. Governments, departments of health and organizations such as PEPFAR and the Global Fund need to take steps now to ensure that the progress made over the past few years to control the HIV pandemic does not go into reverse.
Across sub-Saharan Africa, health-care providers have used various approaches to try to protect essential health services from disruptions caused by the COVID-19 pandemic. Examples in HIV programmes include providing people with several months’ worth of antiretroviral therapy instead of one- or two-months’ supply; providing antiretroviral therapies or ways to check CD4 T-cell levels at people’s homes or at community centres; and online appointments with physicians15. Care providers and others can use the experiences of the past two years to map out how best to scale up effective strategies in the future.
In the longer term, stakeholders could also apply some of the innovations in the global COVID-19 response to HIV. Extraordinary achievements, for instance, in the tracking of cases and deaths, in genomic surveillance and in data sharing have demonstrated the degree to which ‘knowing your epidemic’ in near-real time can help to guide a public-health response at local, national and global scales.
In fact, besides impressive global collaboration, the scientific response to COVID-19 has strengthened local and regional collaboration across Africa, including in clinical research, in the trials of vaccines and therapeutics, and in epidemiology and genomics16–18. The scientific community globally should support these networks and expand their scope to help address HIV as well as the other public-health priorities in Africa — tuberculosis, malaria and neglected tropical diseases.
Integrate health systems. Governments, departments of health and HIV programmes need to find better ways to integrate COVID‑19 and HIV services. Providing COVID-19 vaccination at clinics and centres that currently offer testing and antiretroviral therapies for HIV could help to ensure that people with advanced or uncontrolled HIV are prioritized for COVID-19 vaccination, including any additional doses that might be recommended.
Similarly, people living in countries that have high rates of HIV should be offered HIV testing whenever they receive a COVID-19 vaccine. Currently, the WHO recommends that people in these countries are offered HIV testing whenever they have any contact with the health system. (In practice, this happens patchily.) Thus, providing people with prevention and care for COVID-19 provides an opportunity to boost care and treatment for HIV.
Ultimately, sustained efforts to ensure that people with HIV are diagnosed, given antiretroviral treatment and then followed up to ensure that their viral load is being suppressed (see ‘Africa’s HIV treatment gap’) are crucial to reducing the burden of advanced HIV in the population — and so limiting the potential for cases of prolonged infection from SARS-CoV-2. Encouragingly, in our case study from South Africa, the individual cleared the SARS-CoV-2 infection three weeks after being given effective HIV treatment5.
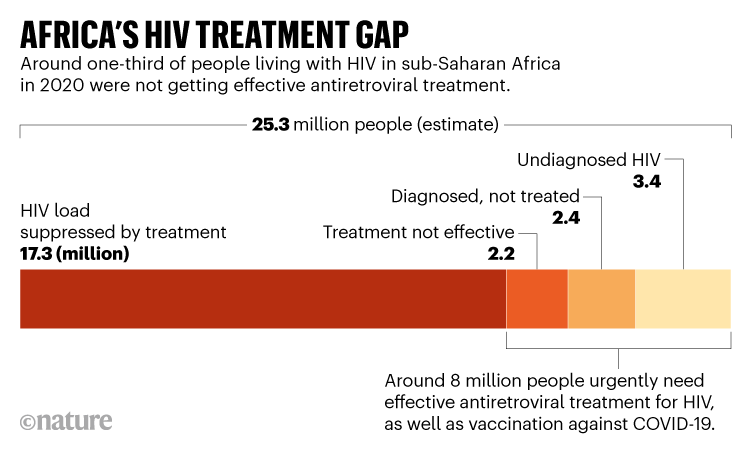
Source: UNAIDS (2020 data)
Avoid stigmatization
What the past year has shown is that early — and ongoing — complacency about how the COVID-19 pandemic is playing out in Africa is misplaced.
Comparing only cases and deaths across countries or continents with different demographics, and obtained using different testing strategies and reporting systems, can give a misleading picture19. A rolling analysis of excess deaths in South Africa, for instance, indicates that deaths from COVID‑19 could be between two and three times higher than reported deaths, and that South Africa has been one of the hardest-hit countries in the world (see go.nature.com/3r6dt3j). Certainly, a 30–50% increased chance of death from COVID-19 for a young sector of the population that makes up most of the workforce could have devastating consequences in the long term.
On the flip side, an obvious risk of drawing attention to the interactions between SARS-CoV-2 and HIV is increasing the stigmatization of people living with HIV. It could also encourage the application of unfair public-health measures (such as travel restrictions) to countries with high rates of HIV.
The United States banned non-citizens who had tested positive for HIV from entering the country for 22 years. (The ban was lifted only in 2010.) And many other countries, such as Australia and New Zealand, still refuse to give citizenship to people with HIV, even though effective antiretroviral treatments are now available.
The best way for governments to protect their citizens is not by further stigmatizing those infected with HIV; it is by quickly providing vaccines to protect the world’s most vulnerable. Only global solidarity — not discrimination, blockage or the hoarding of resources — will end the COVID-19 pandemic.

 Victories against AIDS have lessons for COVID-19
Victories against AIDS have lessons for COVID-19
 COVID vaccines to reach poorest countries in 2023 — despite recent pledges
COVID vaccines to reach poorest countries in 2023 — despite recent pledges
 African nations missing from coronavirus trials
African nations missing from coronavirus trials
 Ebola prepared these countries for coronavirus — but now even they are floundering
Ebola prepared these countries for coronavirus — but now even they are floundering







