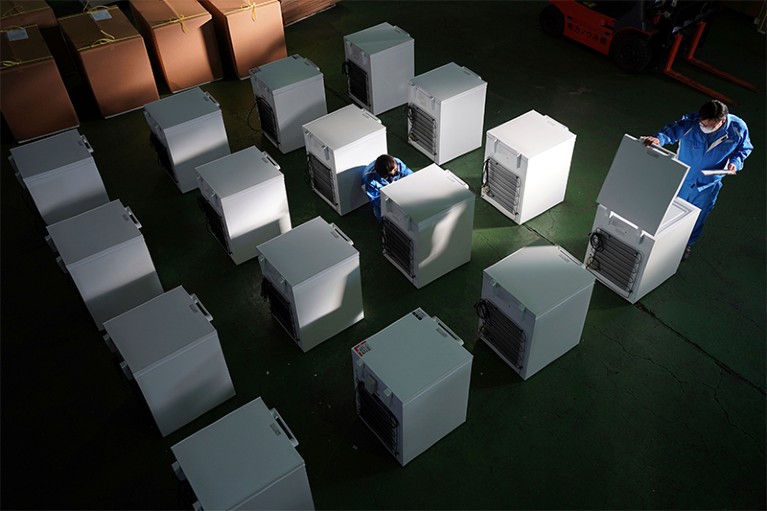
Ultralow-temperature freezers, used for storing certain COVID-19 vaccines, await shipment from a warehouse in Sagamihara, Japan.Credit: Eugene Hoshiko/AP/Shutterstock
Close to 7 billion doses of COVID-19 vaccines had been administered worldwide by the end of October, potentially saving the lives of millions of people. Little wonder that vaccine research and development leaders say that increasing numbers of early-career researchers are interested in the field. Nature spoke to scientists and engineers about what it takes to research, produce and deliver new vaccines. Here’s their advice.
Train broadly
Early efforts to develop COVID-19 vaccines received a major boost when key details of the 3D structure of the SARS-CoV-2 spike protein were published by Jason McLellan, a structural biologist at the University of Texas at Austin, and his colleagues1.
McLellan had previously worked on the Middle East respiratory syndrome coronavirus (MERS-CoV), first seen in Saudi Arabia in 2012. Like SARS-CoV-2, MERS-CoV is studded with spike proteins that change shape when they fuse with host cells. With their key role in infection, these proteins make an obvious candidate on which to base vaccines. However, coronavirus spikes are, in their natural form, liable to change out of the pre-fusion shape that would make them useful in vaccines. McLellan and his postdoctoral researcher Nianshuang Wang solved this problem by tweaking the pre-fusion MERS-CoV spike to produce a stable version that they called the 2P mutation2.
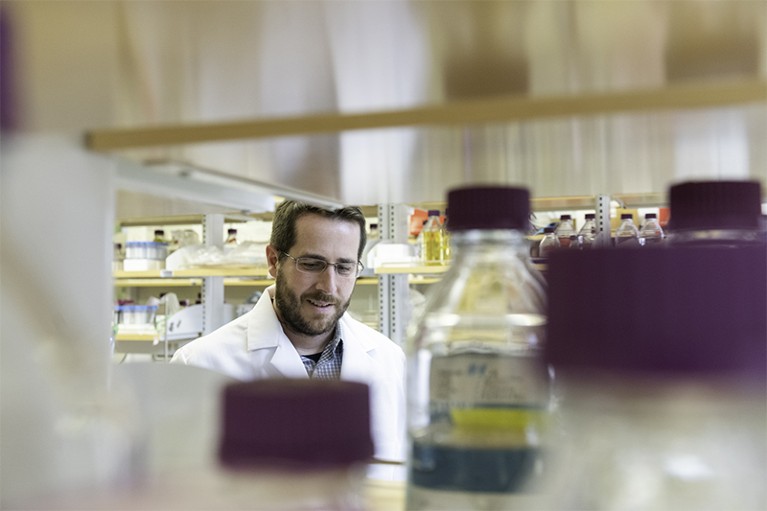
Jason McLellan helped to determine key parts of the structure of SARS-CoV-2.Credit: Vivian Abagiu/University of Texas at Austin
When virologist Yong-Zhen Zhang at Fudan University in Shanghai, China, published the genetic sequence of SARS-CoV-2 on 10 January 2020 (see go.nature.com/3essufb), McLellan and his colleagues pinpointed where in the sequence to make the same 2P mutation to produce a stable version of the SARS-CoV-2 spike. Their manuscript provided vaccine developers with a potential direction: the COVID-19 vaccines made by Moderna in Cambridge, Massachusetts; BioNTech in Mainz, Germany, and Pfizer in New York City; Johnson & Johnson in New Brunswick, New Jersey; and Novavax in Gaithersburg, Maryland, are all based on this stabilized spike.
Part of Nature Career Guide: Vaccines
Vaccinology of this kind, involving the use of 3D structural information, has been made possible by advances in techniques such as X-ray crystallography and cryogenic electron microscopy.
“It’s a really exciting time to be in the field,” says McLellan. “A lot of companies are hiring. I’ve had companies contacting me to ask if we can recommend people in the field or if anyone in my lab can help them with their vaccine antigen design.”
McLellan says that those seeking to break new ground might do well to gain expertise in more than one field. “I’d say don’t overspecialize. Vaccine design requires an understanding of structural biology, protein chemistry, vaccinology, virology and immunology. If you’re a virology or immunology PhD, for example, you could go on to a postdoc in structural biology and protein design. You want to train broadly.”
Persevere through setbacks
After completing a PhD in 2002 on a chicken coronavirus, viral immunologist Lisa Ng started studying hepatitis B at the Genome Institute of Singapore. But her change of focus did not last long. In March 2003, a coronavirus was revealed to be the cause of the severe acute respiratory syndrome (SARS) pandemic spreading across the Chinese mainland, Hong Kong, Vietnam, Canada and Singapore — causing panic, quarantines and 774 deaths.
Ng was reassigned to a team working to develop a reliable polymerase chain reaction (PCR) test for SARS. Working long hours under pressure, the group did so in two months.

Lisa Ng works to advance immunological understanding of a range of viral infections, from SARS-CoV-2 to Zika, dengue, Ebola and Chikungunya.Credit: Corporate Communications, A*STAR
It would not be the last time that she experienced a sudden increase in demand for her expertise in the mechanisms of coronavirus replication and host immune responses. “I was in the right place at the right time,” she says.
Lessons learnt from doing research amid a humanitarian crisis
In 2007, Ng went on to start her own group at the Singapore Immunology Network. She and her team work to advance immunological understanding of viral infections, such as Zika, dengue, Ebola and Chikungunya, that are endemic in tropical regions. In April, she was appointed to lead the A*STAR Infectious Diseases Labs, a research institute set up that month that collaborates internationally to stop emerging infectious diseases from causing widespread health and economic harm.
Since 2020, Ng has refocused her own group’s expertise on the race to better understand and combat SARS-CoV-2. She has, for example, identified specific antibodies in the blood of people who have recovered from COVID-19 that can eliminate the virus and offer protection against infection3.
Ng warns those thinking about focusing their careers on vaccine science to do so only if they are genuinely committed. “You need to really have a passion and the interest level to enjoy it. You need to do what you like, not what is fashionable.”
She adds that early-career researchers who can shrug off setbacks will be better placed to take advantage of opportunities when they arise. “I still get annoyed when my manuscript isn’t accepted for publication in my preferred journal, but it is important to be resilient. Don’t throw in the towel too quickly. Remember that some days your story will suddenly end up in a very nice place when you are least expecting it.”
Seek perspectives beyond your field
The pandemic has shown how getting vaccines through clinical trials can sometimes be just part of the battle: the doses, when approved, then have to be produced in volume.
“The demand is huge and urgent,” says Zoltán Kis, a bioprocess engineer at the University of Sheffield, UK. “There was no dedicated capacity to make vaccines against an unknown ‘disease X’ before the pandemic. For new technologies like RNA vaccines, there is a lack of technical experts and raw-material supply chains to scale up production. Even for conventional vaccines, there isn’t the spare capacity needed without disrupting the production of other life-saving vaccines.”

Zoltán Kis uses bioprocess engineering to develop cost-effective methods for increasing production of RNA-based vaccines, while ensuring quality and consistency.Credit: Timm Cleasby
As vaccines progress from preclinical research, through clinical trials and on to commercial production, increasingly large batches are needed. As this scale-up progresses, process engineers must develop cost-effective methods that increase production and minimize waste, while ensuring quality and consistency. Mass-production methods used for vaccines generally bear little resemblance to those used in laboratories.
Until earlier this year, Kis had worked at the Future Vaccine Manufacturing Research Hub at Imperial College London, investigating how to improve vaccine production and distribution in developing countries. He moved to Sheffield in September, to set up a group focused on producing RNA-based vaccines by combining automated physical processes with computer modelling.
The tangled history of mRNA vaccines
In research published in April4, Kis and his colleagues outlined how such vaccines could be developed using a methodology called Quality by Design. The approach, developed in the 1990s, has been used by the European Medicines Agency and the US Food and Drug Administration to assess drug development. It involves focusing clearly on the relationships between the most important attributes of a product, and on the design features and production-process parameters required to achieve these.
Kis also thinks it should be possible to apply ‘digital twin’ techniques to vaccine production. A digital twin is a virtual representation of a physical process — in this case, the preparation of a vaccine batch.
This would involve gathering data on variables such as pH levels and temperature, to produce virtual models that enable real-time quality control. It’s an approach that is already in use in other, simpler processes, but Kis thinks it has huge potential in vaccine production. “If you then have a predictive model, you can work out what will happen in the next five to ten minutes and make changes to prevent a loss of quality before it occurs,” he says.
Bioprocess engineering requires operating at the interfaces of disciplines, and can involve roles in industry, academia, regulatory bodies and non-governmental organizations. Kis advises those starting out in the field to seek out the perspectives of people in other disciplines. “It’s important to be able to bridge the gap between the deep, specific research in one area we might be doing and the big picture,” he says.
During a pandemic, virologists and immunologists are more likely to make headlines than are process engineers. That’s not something that worries Kis, who enjoys the challenges and opportunities presented by his work. “The RNA platform, combined with real-time monitoring, advance modelling and automation, could be a game changer in how we make vaccines,” he says. “There’s a lot of scope for innovation, and interesting problems to solve. The potential end result of quick and efficient production of vaccines for a variety of diseases is at least as exciting.”
Where business meets technology
Developing vaccines to combat diseases is a crucial endeavour. There is, however, little point in doing so if they cannot be delivered safely, and in timely and trustworthy ways, to those who need them.
COVID-19 has presented those charged with running vaccine supply chains with a series of complex problems. “You’ve got a new set of players handling extreme volumes in short periods of time,” says Jonathan Wright, a global managing partner at IBM, the US-based technology multinational, who has previously worked in supply-chain management for the multinational companies ExxonMobil, Accenture and Ernst & Young.

Jonathan Wright and his colleagues designed a distribution system that enables manufacturers, distributors, suppliers and customers to share information on batches of vaccines.Credit: IBM
The right number of doses need to reach the right people at the right time; batches must be kept at the appropriate temperatures; bottlenecks in materials must be avoided; and users need to know that supplies are genuine. “Trust and authenticity are important in the supply chains for bags and fashion items,” he says. “When you’re injecting something into someone’s arm, or that of their children, they become absolutely critical.”
That’s one of the reasons that Wright and his colleagues at IBM used ‘blockchain technology’ when designing a vaccine-distribution system. In their Vaccine Accountability Network platform, data on batches of vaccine are gathered and added to a decentralized digital ledger that is constantly updated as supplies proceed through the supply chain.
The Internet of Things comes to the lab
Packages, or blocks, of data on variables such as production date and storage temperature, are shared between manufacturers, distributors, suppliers and customers. New blocks, created when new information is added, include the data from previous blocks, so forming a chain. The blockchain ensures that records can’t be altered retrospectively, providing improved security and confidence in the authenticity of the data. Artificial intelligence (AI) is used to identify any early signs of disruption, to prioritize ordering on the basis of need and to manage inventories.
Companies involved in vaccine and other supply chains need technology specialists who understand the business potential of technologies such as blockchain, AI, advanced automation and the Internet of Things — a vision of the future in which everyday objects, from toasters to traffic lights, collect and share information online. “One of the biggest challenges faced by large corporations is that business people often don’t understand technology, and technologists often don’t understand business,” says Wright. “The people I want working for me really understand that interface, because the more we can get people to operate at that intersection, the more we will drive innovation.”
Communicate with non-scientists
Sometimes, the old ways are the best, says Maria Elena Bottazzi, co-director of the Texas Children’s Hospital Center for Vaccine Development at Baylor College of Medicine, Houston. Although some of the vaccines rapidly rolled out to protect people from COVID-19 are based on cutting-edge viral vector and messenger RNA technologies, not enough doses of them can be produced for everyone.
“Yes, we need innovation,” says Bottazzi. “But the novel vaccine technologies are not even close to being deployed at scale outside high-income countries. Even if we waived the intellectual-property rights tomorrow, we don’t have the infrastructure to make the billions of doses we need to vaccinate the world.”

Maria Elena Bottazzi leads a team whose COVID-19 vaccine is in a phase III trial in India.Credit: Baylor College of Medicine
When Bottazzi and her colleagues set out to make a SARS vaccine in 2011, they went for recombinant protein technology that had been in use since the 1980s. Their yeast-expressed candidate, based on the receptor-binding domain of the SARS-CoV spike protein, was thermally stable and could be easily scaled up, making it ideal for manufacture in low- and middle-income countries5.
In early 2020, the group adapted its earlier work to produce a COVID-19 vaccine technology6. The result is Corbevax, now being tested in a phase III trial in India — where more than 10,000 cases and hundreds of deaths are being reported every day. The Indian government has pre-ordered 300 million doses. Bottazzi says that Corbevax will cost less than US$2 a dose. By comparison, the reported costs of BioNTech–Pfizer and Moderna vaccines are around $23 and $30 a dose, respectively.
Bottazzi was born in Italy but grew up in Honduras, where she experienced at first hand the burden of tropical diseases, especially on rural populations. This “wake-up call”, as she describes it, inspired her early education and training in microbiology and immunology. Alongside her academic focus, Bottazzi studied business and management. Today, she co-leads work at the Texas Children’s Hospital Center to develop vaccines for Chagas disease, hookworm and schistosomiasis.
Those who want to succeed in vaccine science must learn to communicate better with non-scientists, says Bottazzi. “We are taught to write grant applications and manuscripts. But we have to get out of the cocoons of our labs, stop speaking in complex terminology and learn to engage effectively with funders, policymakers, industry and general audiences.”
Bottazzi is both thrilled by, and nervous at, reports from India suggesting Corbevax could be rolled out before the end of the year. “It’s an amazing feeling,” she says. “It’s also quite a stressful feeling because the closer we get, the more eager we are to continue contributing.”

 How to get a job in vaccine development
How to get a job in vaccine development
 Lessons learnt from doing research amid a humanitarian crisis
Lessons learnt from doing research amid a humanitarian crisis
 The tangled history of mRNA vaccines
The tangled history of mRNA vaccines








