Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Rent or buy this article
Prices vary by article type
from$1.95
to$39.95
Prices may be subject to local taxes which are calculated during checkout
Nature 597, S24-S26 (2021)
doi: https://doi.org/10.1038/d41586-021-02629-w
This article is part of Nature Outlook: Stem cells, an editorially independent supplement produced with the financial support of third parties. About this content.
Updates & Corrections
-
Correction 06 October 2021: An earlier version of this Outlook article misspelt Kharufeh’s name throughout.
References
Rama, P. et al. N. Engl. J. Med. 363, 147–155 (2010).
Hayashi, R. et al. Nature 531, 376–380 (2016).
Gouveia, R. M. & Connon, C. J. Trans. Vis. Sci. Tech. 9, 5 (2020).
Isaacson, A., Swioklo, S. & Connon, C. J. Exp. Eye Res. 173, 188–193 (2018).
Oswald, J., Kegeles, E., Minelli, T., Volchkov, P. & Baranov, P. Mol. Ther. 21, 180–198 (2021).

 Stem cells
Stem cells
 Stem cells: highlights from research
Stem cells: highlights from research
 The promise and potential of stem cells in Parkinson’s disease
The promise and potential of stem cells in Parkinson’s disease
 Stem cells and spinal-cord injuries: an intricate issue
Stem cells and spinal-cord injuries: an intricate issue
 The chimaera challenge
The chimaera challenge
 The next frontier for human embryo research
The next frontier for human embryo research
 Why stem cells might save the northern white rhino
Why stem cells might save the northern white rhino
 Stem-cell start-ups seek to crack the mass-production problem
Stem-cell start-ups seek to crack the mass-production problem
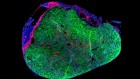
 The rise of the assembloid
The rise of the assembloid