- OUTLOOK
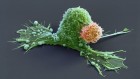
Scientists are harnessing viruses to treat tumours
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Rent or buy this article
Prices vary by article type
from$1.95
to$39.95
Prices may be subject to local taxes which are calculated during checkout
Nature 587, S60-S62 (2020)
doi: https://doi.org/10.1038/d41586-020-03226-z
This article is part of Nature Outlook: Multiple myeloma, an editorially independent supplement produced with the financial support of third parties. About this content.
References
Yarde, D. N. et al. Exp. Hematol. 41, 1038–1049 (2013).
Jelinek, T. et al. Front. Immunol. 9, 2431 (2018).
Thirukkumaran, C. M. et al. Blood Adv. 3, 797–812 (2019).

 Outlook: Multiple myeloma
Outlook: Multiple myeloma
 Will the reclassification of multiple myeloma change how people are treated?
Will the reclassification of multiple myeloma change how people are treated?
 Burning questions about smouldering myeloma
Burning questions about smouldering myeloma
 The screening imperative for multiple myeloma
The screening imperative for multiple myeloma
 How researchers are addressing the racial imbalance in multiple myeloma
How researchers are addressing the racial imbalance in multiple myeloma
 Immunotherapies target multiple myeloma
Immunotherapies target multiple myeloma
 Research round-up: Multiple myeloma
Research round-up: Multiple myeloma