As data accumulate that, in some places, people of colour are much more likely than white people to become ill and die of COVID-19, more discussions are grasping at factors beyond race to explain why. I’m used to this. When my book on environmental racism came out last year, one of the most common questions I received concerned alternative explanations for the greater ill health of minority ethnic groups. Surely, I was asked, the issue is not race, but poverty?
Poverty is a risk factor for becoming unwell. But racial disparities in exposure to environmental pollutants are greater factors that remain even after controlling for income. African Americans who earn US$50,000–60,000 annually — solidly middle class — are exposed to much higher levels of industrial chemicals, air pollution and poisonous heavy metals, as well as pathogens, than are profoundly poor white people with annual incomes of $10,000. The disparity exists across both urban and rural areas.
We need to take a longer, harder look at environmental racism — systems that produce and perpetuate inequalities in exposure to environmental pollutants. These can persist even in the absence of malevolent actors. The main culprits include indifference and ignorance, inadequate testing of industrial chemicals, racism, housing discrimination, corporate greed and lax legislation from, in the United States, a weakened Environmental Protection Agency. To combat these, society must actively take responsibility. By anticipating the outsized environmental assaults that people of colour face, we can act to protect lives during the current pandemic and future outbreaks.
The architecture of inequality
It’s true that pathogens are democratic by nature. It’s also true that marginalized minority ethnic groups have increased exposure to environmental pollution and reduced access to health care. All this creates physical and social vulnerabilities that leave people of colour less able to resist and survive infections such as the coronavirus. This is not only a problem in the United States. In April, the UK Intensive Care National Audit and Research Centre estimated that 35% of people in intensive care with COVID-19 are black, Asian or members of other minority ethnic groups, nearly triple their proportion in the UK population. The first ten physicians in the United Kingdom known to have died from COVID-19 were also from black, Asian or minority ethnic groups. Crowded housing and working conditions have been suggested as a reason for the disparity. Only 2% of white people in the United Kingdom live in crowded conditions, but 30% of Bangladeshi, 16% of Pakistani and 15% of black African households are overcrowded. Black and minority ethnic people are also more likely to live in ‘deprived’ areas that are closer to sources of industrial pollution — from lead-tainted water in Flint, Michigan, to nerve gas, arsenic and polychlorinated biphenyls in Anniston, Alabama.
How to address the coronavirus’s outsized toll on people of colour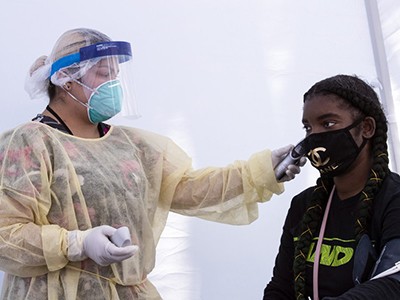
Black and minority ethnic populations are also more likely to live in neighbourhoods where they are exposed to high levels of lead and to air pollution. Greater exposure to air pollution has long been tied to shorter life expectancy. It can exacerbate heart diseases, trigger hypertension and compromise immune systems. A preliminary study published on a preprint server (Wu, X. et al. Preprint at medRxiv https://doi.org/10/ggrpcj; 2020) linked exposure to an increased likelihood of dying from COVID-19. Poor access to nutritious food makes matters worse. The term food deserts is often used for neighbourhoods that lack grocery stores and other vendors of fresh produce. I prefer ‘food swamp’ because such neighbourhoods are often teeming with places selling junk food, alcohol and tobacco. This foments obesity and nutritional deficiencies, which magnify the harms of environmental pollution. Vitamin C, calcium, and iron in the diet prevent the absorption of lead, a poisonous metal. A similar argument can be made about access to green spaces and exercise facilities.
Data on child deaths are a call for justice
To mitigate and prevent these and other inequalities, we need to collect and disseminate better data. Authorities need to document race, and not assume relevant information can be captured by socio-economic status. The US Centers for Disease Control and Prevention agreed to report deaths by race and ethnicity only when put under pressure, and several weeks after the first US death. As of 16 May, only 40 states were reporting the race of people who had died of COVID-19, and only 3 were reporting race for people who received COVID-19 tests.
In the 1990s, health scholars and practitioners were caught unaware by the higher rates of HIV infection and mortality in communities of colour. The pattern is being repeated in deaths from COVID-19. Policymakers need to recognize this and target interventions — perhaps by increasing testing for vulnerable populations. We need to look beyond blame-shifting assumptions that genetic differences or lifestyle ‘choices’ can explain medical disparities. Risks such as where a person lives or what they eat often reflect realities that lie beyond that person’s control. Social distancing is impossible for someone who lives in a crowded flat and must work cheek by jowl in a meat-packing plant.
Instead, treatment and research must be designed using information about differences in access to health care and exposure. This approach will help everyone: as Tedros Adhanom Ghebreyesus, head of the World Health Organization, says: “No one is safe until everyone is safe.” Most of all, we must remember that if we don’t confront environmental racism directly, we cannot overcome it.


 How to address the coronavirus’s outsized toll on people of colour
How to address the coronavirus’s outsized toll on people of colour
 Data on child deaths are a call for justice
Data on child deaths are a call for justice
 The architecture of inequality
The architecture of inequality



