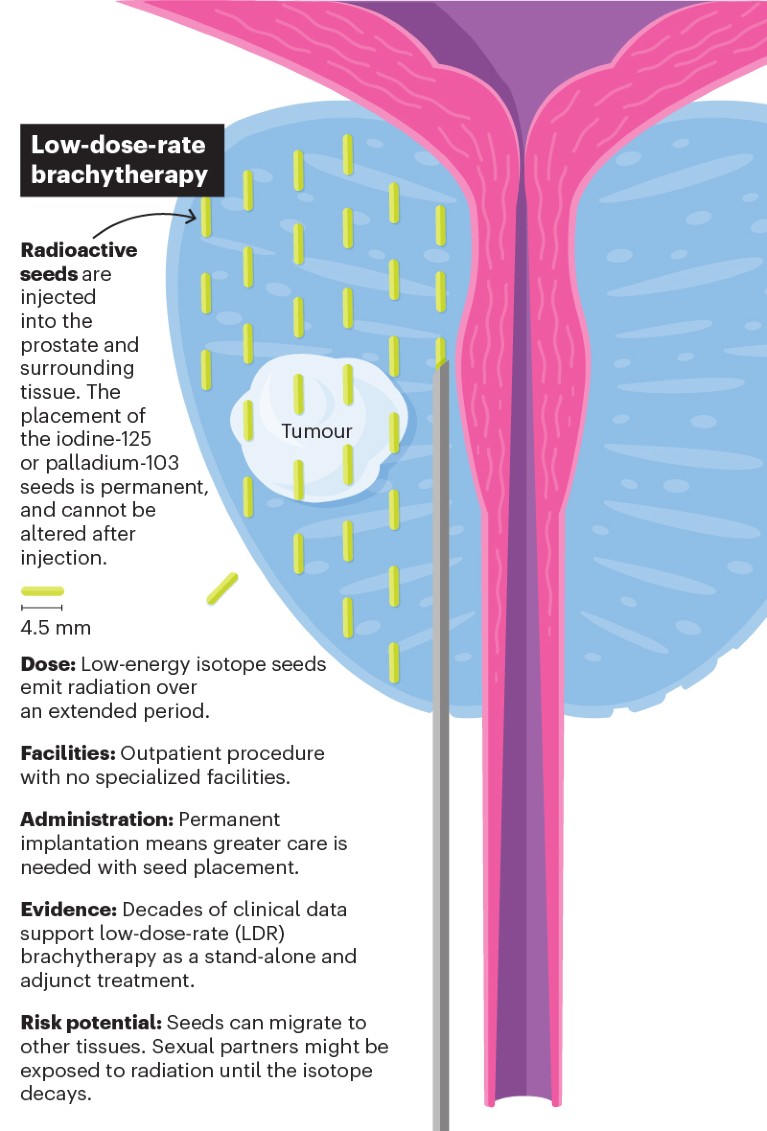
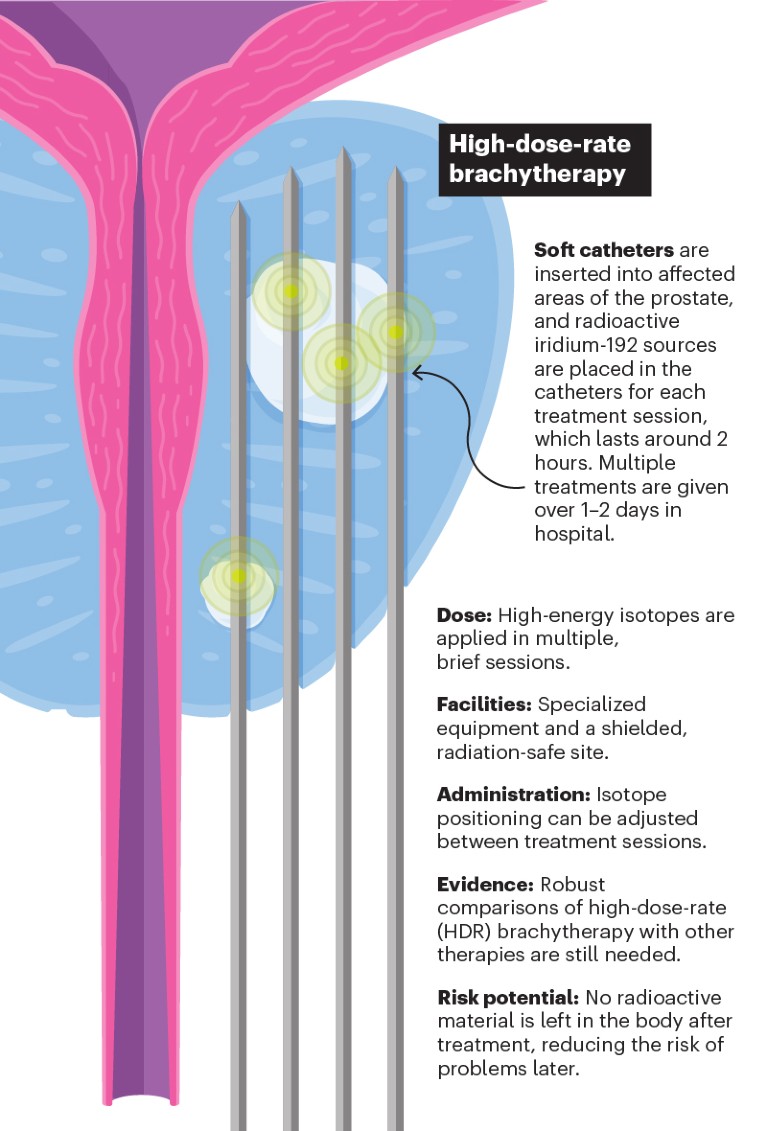
Old therapy, new approach
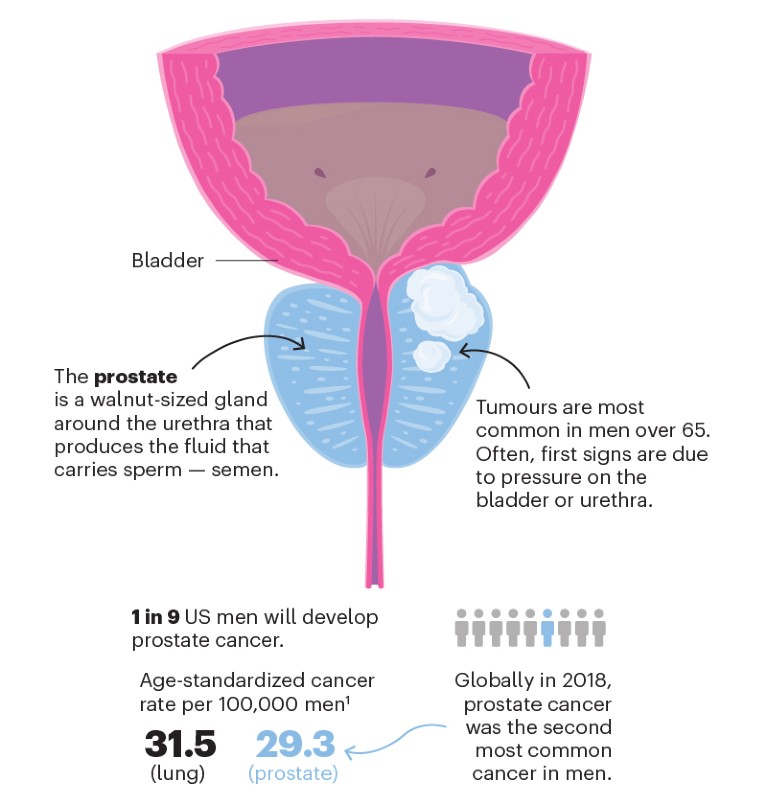
Brachytherapy uses radioactive material to kill cancerous cells. The conventional approach involves permanently implanting radioactive pellets in and around the prostate. In a newer form of brachytherapy, radioactive material is introduced temporarily through removable catheters. This might improve safety and efficacy, although only limited clinical data are available.
Credit: Lucy Reading-Ikkanda
Credit: Lucy Reading-Ikkanda
Credit: Lucy Reading-Ikkanda
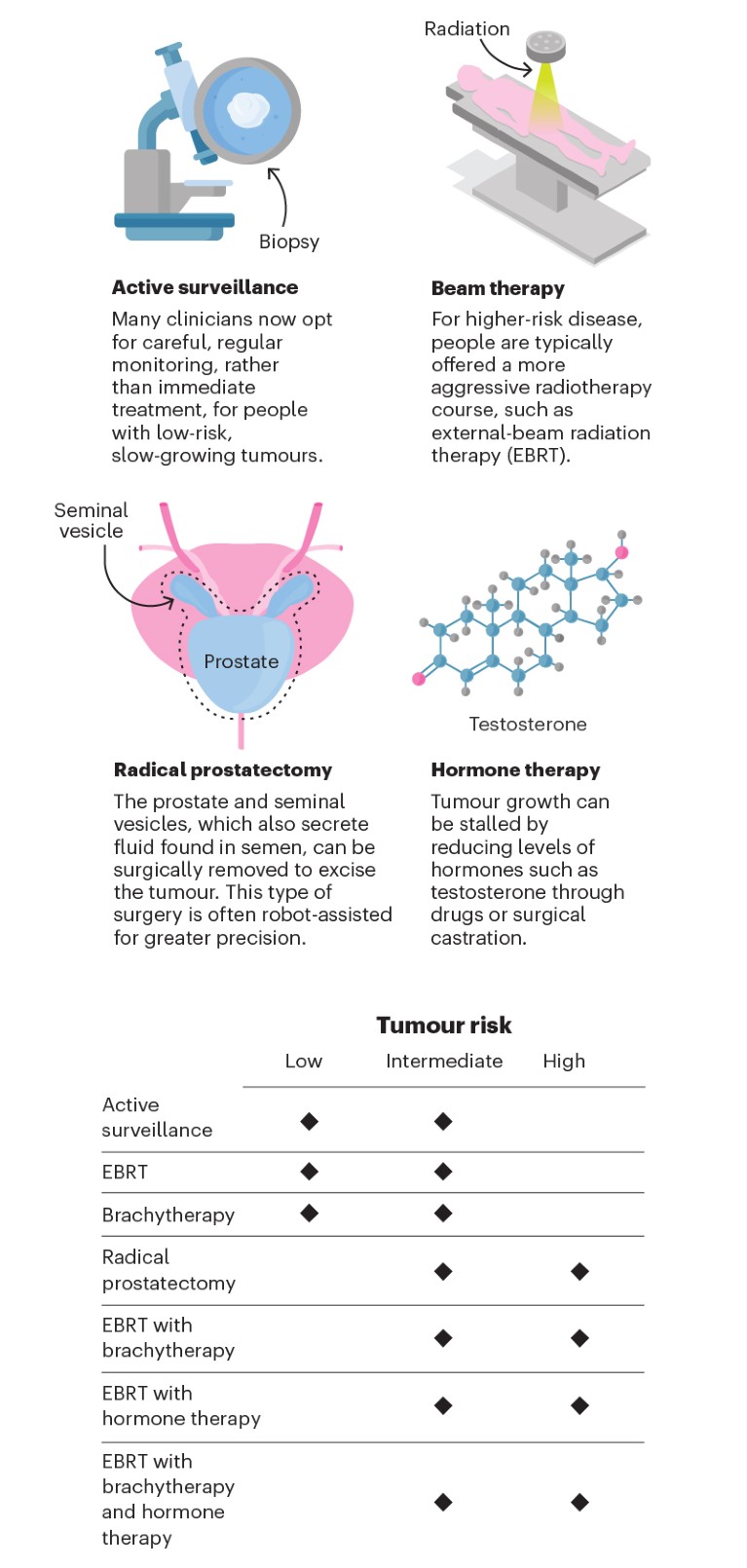
A question of risk
Brachytherapy is one of several treatment options for prostate cancer. Treatment suitability depends on a tumour’s level of risk, determined on the basis of factors such as size and cellular structure. Brachytherapy can be used alone for lower-risk tumours, or to boost more aggressive radiotherapy or hormone therapy in higher-risk cases.
Credit: Lucy Reading-Ikkanda
A valuable option
Randomized controlled trials have shown that brachytherapy has similar benefits as those of other treatments, but can be delivered at a lower cost and, in many cases, with more easily managed side effects.
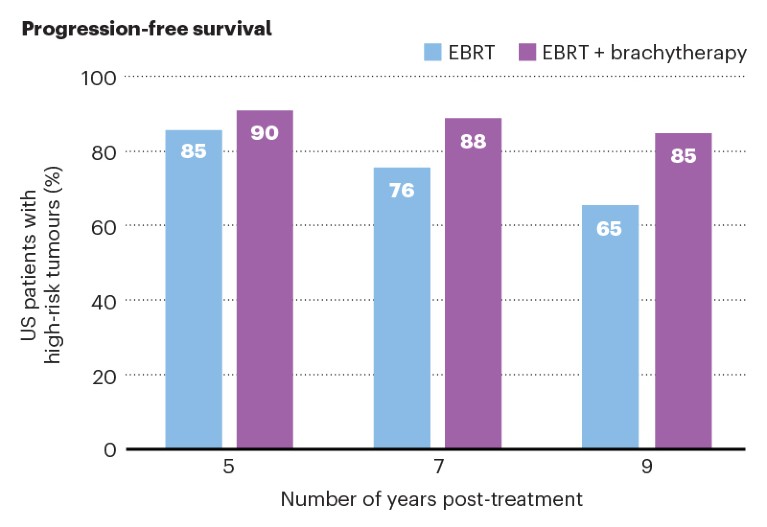
Survival gains In people with low-risk tumours, brachytherapy is as effective (96%) as robotic surgery (97%) at preventing cancer recurrence within two years2. For high-risk disease, combining brachytherapy with EBRT boosts progression-free survival compared with EBRT alone3.
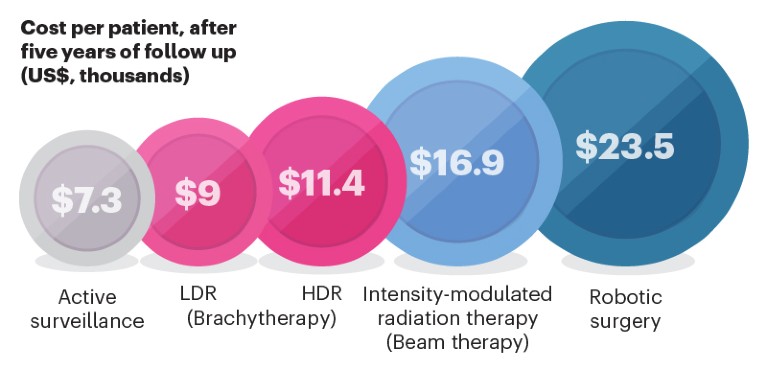
Cost-effective The cost of brachytherapy in US hospitals compares favourably with that of cutting-edge treatments such as advanced forms of beam therapy and robot-assisted surgery4. In Europe, treatment costs are more closely matched.
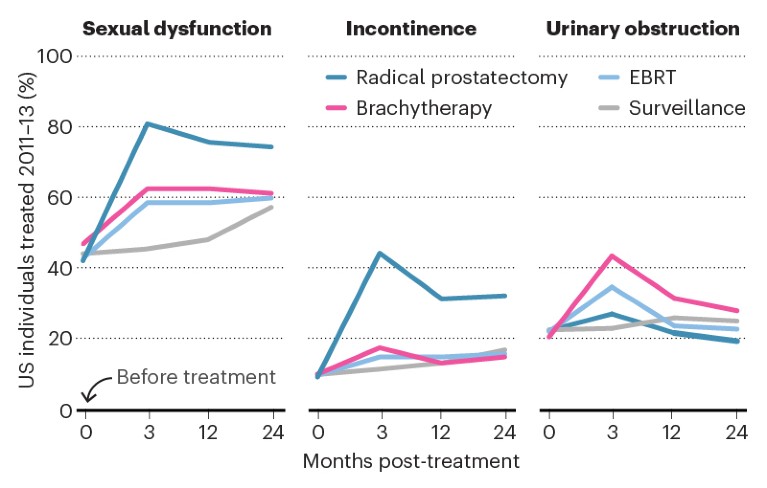
Side-effect selection Compared with surgery, brachytherapy tends to carry a lower risk of causing sexual dysfunction and incontinence. But it is associated with greater rates of urinary-tract obstruction than are other treatments5.
Slide away
Despite its apparent benefits, brachytherapy is struggling to compete with a growing clinical armamentarium. Worldwide, dwindling training opportunities put the future of this technique in jeopardy.
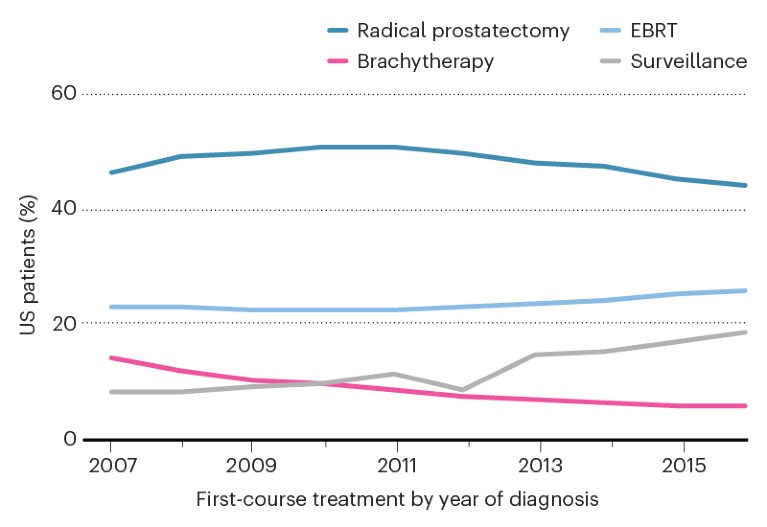
Decreasing use The proportion of US medical facilities performing brachytherapy has been falling each year since 2007, partly because clinicians are delaying treatment for low-risk malignancies in favour of active surveillance. But brachytherapy’s use is also sliding compared EBRT and surgery7.
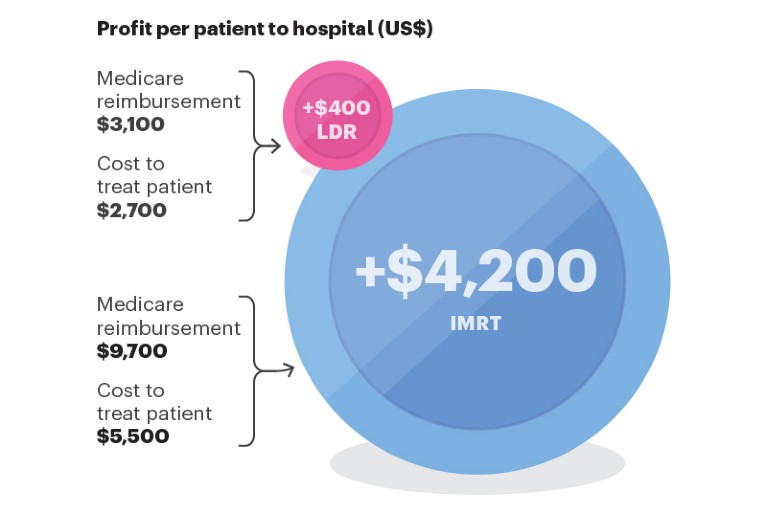
Funding issues In the United States, reimbursement rates by health insurer Medicare for brachytherapy (profit for LDR shown) are closer to the true cost than for other, more costly therapies, such as intensity-modulated radiation therapy (IMRT). This means the other therapies are more profitable8. In Europe, the reimbursement received by some hospitals doesn’t always cover the cost of brachytherapy.
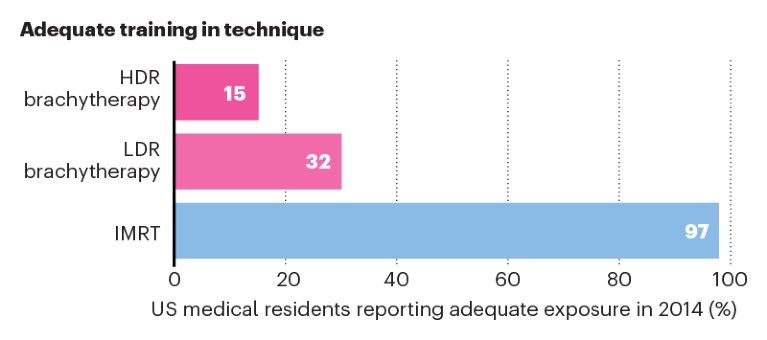
Opportunity cost As brachytherapy’s popularity declines, so do the opportunities for clinicians early in their career to observe and learn the technique. US medical residents increasingly report insufficient opportunity for training in brachytherapy relative to newer therapies9. This could lead to further reductions in access.

 Nature Outline: Prostate cancer
Nature Outline: Prostate cancer
 The declining art of brachytherapy
The declining art of brachytherapy
 Brachytherapy’s fight for survival
Brachytherapy’s fight for survival




