
Staying active into old age can extend health.Credit:Barbara Alper/Getty
Lifespan: Why We Age — and Why We Don’t Have To David A. Sinclair and Matthew D. LaPlante Atria (2019)
Elderhood: Redefining Ageing, Transforming Medicine, Reimagining Life Louise Aronson Bloomsbury (2019)
This year, people over 65 began to outnumber those under 5 for the first time in history. Like climate change, the ageing of humanity is indisputable. Yet the implications of that, and remedies for it, are subject to considerable debate. Now, two books with very different perspectives seek to address how to prepare for this ‘grey tsunami’.
Lifespan, by geneticist David Sinclair and journalist Matthew LaPlante, provides a vision of a not-too-distant future in which living beyond 120 will be commonplace. Physician Louise Aronson’s Elderhood focuses, by contrast, on the often bewildering and sometimes dehumanizing landscape of current geriatric care. Both books wrestle with the complexities of the coming demographic shift. Countries such as the United States — already devoting more than one-third of its health-care dollars to people over 65 — will have to come to terms with an iller, older population. But their solutions are distinct. For Sinclair and LaPlante, the answer lies in understanding and leveraging why we age; for Aronson, in re-evaluating and re-orienting how we view and treat older people.
Age as disease
Lifespan is entertaining and fast-paced — a whirlwind tour of the recent past and a near future that will see 90 become the new 70. In a succession of colourfully titled chapters (‘The demented pianist’, ‘A better pill to swallow’), Sinclair and LaPlante weave a masterful narrative of how we arrived at this crucial inflection point. Among the historical figures evoked are a sixteenth-century Venetian proponent of caloric restriction, Luigi Cornaro, and the twentieth-century ‘father of information theory’, Claude Shannon.
The authors detail how we might alter the trajectory of human ageing by extrapolating from Sinclair’s own research on key signalling molecules such as NAD+ and the proteins called sirtuins, which alter the lifespans of yeast, certain worms and mice. They predict the emergence of drugs that will modulate these and other molecules known to be involved in longevity pathways, or destroy harmful senescent cells that accumulate as we age and help to fuel disease. Sinclair and LaPlante claim that some of these drugs might already be here. The effects of the widely prescribed diabetes drug metformin and the immune modulator rapamycin, for instance, seem to mimic beneficial strategies — the equivalent of (respectively) exercising more and eating less, in pill form.
Defining ageing as a disease is central to their approach. If we treat age medically, as we do heart disease or cancer, they argue, innovative therapies will emerge more rapidly. That mirrors the increasingly popular ‘geroscience hypothesis’, which posits that therapies targeting the fundamental biology of ageing will help to slow or prevent chronic diseases that plague older people, such as type 2 diabetes and dementia. Sinclair’s argument, based on decades in the lab, is that there is no immutable biological tenet that limits how long, or how well, we can live.
Sinclair and LaPlante examine the economics of extending lives on a crowded, resource-limited planet, and the ethics of tinkering with the supposed natural order. But they also speculate on some inadvertent, potentially positive effects. Knowing you were going to meet your great-great-grandchildren, for instance, might make you a more accountable steward of the present. If many generations lived and worked together, we might all become more empathetic — as Sinclair puts it, “more human”. At a time of political, economic and environmental uncertainty, that could be ever more important.
If Lifespan is a lively sprint into the future of ageing, Elderhood is a contemplative walk in its here and now. Since the early 1990s, Aronson has worked as a geriatrician at the University of California, San Francisco. Her exquisitely written book mixes vignettes about her patients (remarkably, she still makes house calls) with lessons learnt from caring for her elderly parents and insights from her own experience of ageing.
Many of her stories reveal cracks in the US health-care system. We learn, for instance, about Neeta, a frail patient with mild dementia who breaks her hip. After surgery, Neeta is transferred to a less-than-stellar care home where she becomes agitated, is sedated, develops bedsores and spirals into hospice care. We also learn of Aronson’s personal frustrations. In one instance, when physicians in a busy accident and emergency department were too distracted, she had to perform a rectal examination on her own father to demonstrate that he was bleeding internally.
Essential stage
Meshed with these very human tales are a wealth of social, cultural and historical perspectives. At the start of the book, Aronson tells of an encounter with Guy Micco, a physician teaching at the University of California, Berkeley. Micco asked a class to write down associations with the word ‘old’: concepts such as weak and frail predominated. The word ‘elder’, by contrast, elicited terms including respect, experience and knowledge. To Aronson, part of the problem is that we adhere to a utilitarian, late-nineteenth-century concept of the body as a machine. Viewed through that industrial lens, being ‘old’ is no longer the apex of life experience. It is a loss of function and, by extension, of intrinsic worth.
Longevity examined: an ancient Greek’s very modern views on ageing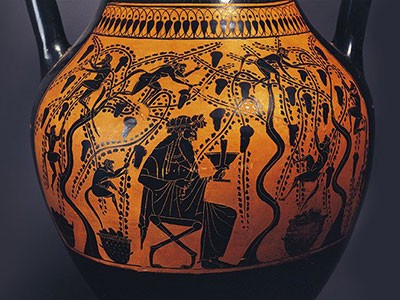
Aronson sees life as a three-act drama: childhood, adulthood and elderhood, the latter subdivided into senior, old, elderly and aged. Each act builds on the one before, and is essential. Aronson notes that emphasizing only the vicissitudes of elderhood is like saying that youth is defined by acne. In fact, in old age we might know ourselves better than ever and obtain more overall life satisfaction. Aronson conceives of anti-ageing not as Sinclair and LaPlante see it — as a bid to medically ‘cure’ the condition — but as battling the many “discriminatory beliefs and policies” affecting the elderly. In her view, the very idea of ‘curing’ ageing is ageist; such a concept is not invoked for any other life stage.
Indeed, in Aronson’s eyes, the worst offender might be the medical system itself. She sees it as failing both patient and physician. It lacks nuance on subtle but important differences in life phases, and focuses on “diseases and organs rather than people and lives”. For instance, she notes that many over-the-counter medicines are not tested on older people, adding risk to prescribing them. She advocates a new paradigm: a re-balancing act in which technology has a role but the focus returns to care. Unlike the high-tech, algorithmic march of modern medicine, her idea of truly ‘personalized medicine’ incorporates the patient’s past experiences and current expectations. This integrative, humanistic model of geriatrics is rare. One can only hope its practices are adopted swiftly.
What are we to conclude? Is ageing a disease that can be eradicated by science, or the natural third act of life, threatened by over-medicalization? Viewpoints will undoubtedly be as variable as experience and temperament. There might be some wisdom in simply following an adage attributed to seventeeth-century philosopher Francis Bacon: “old age is always 15 years older than I am”.


 Longevity examined: an ancient Greek’s very modern views on ageing
Longevity examined: an ancient Greek’s very modern views on ageing
 Extending the healthspan
Extending the healthspan
 Ageing more gracefully
Ageing more gracefully







