Calls for universal US health coverage under Medicare face challenges, such as the fact that end-stage kidney disease consumes 7% of its budget.Credit: Bill Clark/CQ Roll Call
Everybody Wants to Go to Heaven but Nobody Wants to Die: Bioethics and the Transformation of Health Care in America Amy Gutmann & Jonathan D. Moreno Liveright (2019)
The term ‘bioethics’ was coined in 1926, yet the field itself did not emerge until the 1970s. Although my 1975 university thesis (Prospects for Genetic Therapy in Man) reviewed ethical concerns, it took a further four decades before gene therapy was successful in people. More recently, some developments in biomedical technology have accelerated beyond moral or principled boundaries. Among the most shocking was last November’s revelation that the premature and reckless application of human-embryo genome editing had given rise to twin babies in China. That led to calls for a global moratorium (see Nature 566, 440–442; 2019).
Amy Gutmann and Jonathan Moreno have long been at the heart of bioethics debates, and served together for seven years on Barack Obama’s Presidential Commission for the Study of Bioethical Issues. Their book Everybody Wants to Go to Heaven but Nobody Wants to Die (its title is borrowed from a country-music song) reviews the field’s evolution and status.
To begin, Gutmann and Moreno each recount a personal flashback to an older era of ethically problematic medical care. Gutmann’s grandmother and Moreno’s mother underwent medical amputations; neither had been given crucial information by her doctors, so both were uninformed at the time of crucial therapeutic decisions. The authors then tour ethical dilemmas throughout the human life cycle, ranging from reproductive rights to the right to die.
Brain in a dish, babies by design: what it means to be human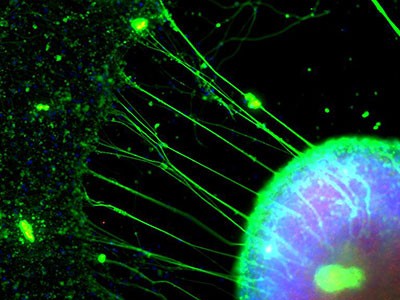
Many of the stops along the way delve into familiar territory — required reading for clinical researchers, and the basis of annual online-testing requirements for conducting clinical research. For instance, the authors cover the infamous, decades-long Tuskegee syphilis study, in which the US Public Health Service withheld penicillin from hundreds of African Americans with the illness. And they discuss the case of Jesse Gelsinger, who died in 1999 from misguided gene therapy intended to treat the rare metabolic disorder ornithine transcarbamylase deficiency.
The authors are not shy about expressing their liberal views, many of which I share. For instance, they declare that health care is a human right, and they believe that people should have the freedom to access safe and legal abortions.
Against a background of calls for “Medicare for All” by several Democratic Party presidential hopefuls, Gutmann and Moreno discuss this government-run, taxpayer-funded health insurance scheme. Covering US citizens aged 65 and older and signed into law in 1965, Medicare was extended in 1972 to include all people with end-stage kidney disease, irrespective of age or demographic. The full costs of dialysis are now footed for more than 500,000 US citizens at a cost of more than US$30 billion a year. And care for end-stage kidney disease consumes approximately 7% of the Medicare budget.
This federal carve-out has fuelled for-profit dialysis centres nationwide. Ultimately, it has caused a lack of financial support for an untold number of people with other conditions, including some with haemophilia or with one of many rare diseases for which treatments are costly and often involve injectable speciality drugs. This demonstrates the problem of providing health care for everyone affected by just one condition, as well as the economic implications of coverage for all in a country that has the highest medical expenditure per person in the world.
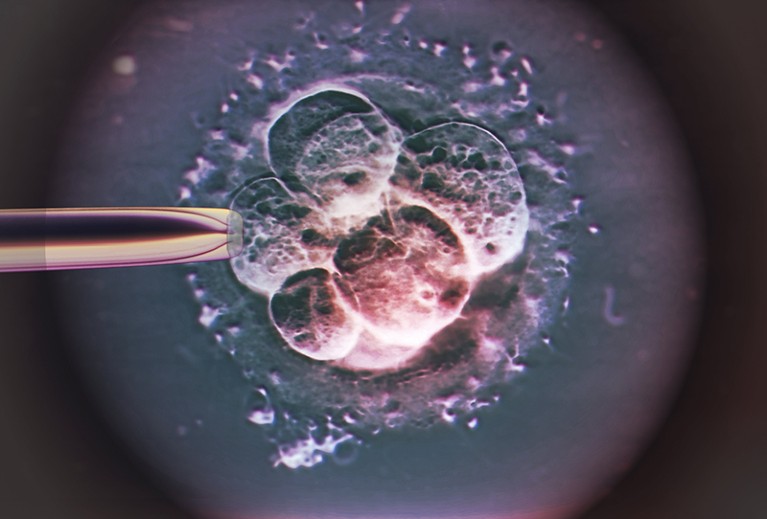
Replacing faulty mitochondrial DNA in embryos is allowed under UK, but not US, law.Credit: Zephyr/Science Photo Library
Despite their vast experience and wisdom, the authors make important errors. One pertains to mitochondrial-replacement therapy. The powerhouses of our cells, mitochondria contain only 0.1% of our DNA, but mutations in that genetic material (known as mtDNA) can be the root cause of rare diseases transmitted from mother to child. To counter this potential when a prospective mother has such mutations, another woman without the mutation can provide donor mtDNA amounting to 0.0005% of the embryo’s genome. Gutmann and Moreno write that, in 2016, the United States gave the green light for male embryos to be given the treatment. In fact, the procedure is still banned by the US Food and Drug Administration, although Britain legalized it in 2015. The authors also erroneously indicate that angiograms — X-rays of blood vessels — can support diagnoses of brain death in people in persistent vegetative states.
A major theme throughout is that patients have more agency and authority today than they once did, and can even co-produce their care, sharing key decisions with their doctors. But the authors’ proclamation that there has been “a collapse of medical paternalism” is off-base. Unfortunately, paternalism is still pervasive. As I noted in my 2014 book, The Patient Will See You Now, some 66% of US doctors will not give patients their office notes, and almost all order routine medical scans without telling the recipient how much exposure to ionizing radiation the tests entail.
There are also key omissions. I was surprised to see no mention of non-invasive prenatal tests, which have accurately identified the potential for fetal chromosomal abnormalities for more than one million prospective parents in the United States. They do not discuss ongoing clinical trials using induced pluripotent stem cells to treat medical conditions such as macular degeneration, Parkinson’s disease or spinal injury. They barely mention the ‘brain in a dish’ approach to neurological research involving human cortical organoids, which is attracting considerable attention from bioethicists. And devoting just a handful of sentences to CRISPR genome editing of human embryos and subsequent births seems remiss.
That’s the way the CRISPR crumbles
Nor do they mention one of the most controversial bioethics incidents in recent years. In 2015, the cognitive psychologist Steven Pinker wrote in the newspaper The Boston Globe: “Biomedical research will always be closer to Sisyphus than a runaway train — and the last thing we need is a lobby of so-called ethicists helping to push the rock down the hill.” Inevitably, bioethicists pushed back at this declaration that they are a kind of guild, a bureaucratic industry entangled in a conflict of interest. It’s a shame that Gutmann and Moreno don’t tackle this frontal assault. The moral compass that bioethicists provide is necessary: all too often, technology is out in front of the deep thinking we need about how it can be best applied.
Indeed, bioethics is often pivotal in educating clinicians about patient care at academic medical centres. That brings me to the concept of casuistry: thinking about ethical problems by assessing a spectrum of cases to which they apply. The book stresses that careful analysis of a case can promote insight.
I experienced this at first hand on my rounds as attending physician in an intensive-care unit. I and my team of medical students and trainees cared for many people facing death. We had to consider ‘do not resuscitate’ orders, and discovered how best to discuss the delicate situation with patients and their families. No one was more thoughtful while weighing in than the bioethicists. When they were absent, there was a sense of loss: we missed their clarity. Whether in the context of an individual patient, a medical-research initiative or the application of new advances, the field of bioethics is essential. We will continue to rely on these professionals for guidance.

 Justice in genomics
Justice in genomics
 Brain in a dish, babies by design: what it means to be human
Brain in a dish, babies by design: what it means to be human
 That’s the way the CRISPR crumbles
That’s the way the CRISPR crumbles