- NEWS AND VIEWS
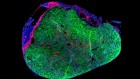
A map of β-cell differentiation pathways supports cell therapies for diabetes
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Rent or buy this article
Prices vary by article type
from$1.95
to$39.95
Prices may be subject to local taxes which are calculated during checkout
Nature 569, 342-343 (2019)
doi: https://doi.org/10.1038/d41586-019-01211-9
References
Veres, A. et al. Nature 569, 368–373 (2019).
Rezania, A. et al. Nature Biotechnol. 32, 1121–1133 (2014).
Pagliuca, F. W. et al. Cell 159, 428–439 (2014).
Nair, G. G. et al. Nature Cell Biol. 21, 263–274 (2019).
Velazco-Cruz, L. et al. Stem Cell Rep. 12, 351–365 (2019).
Bruin, J. E. et al. Stem Cell Rep. 5, 1081–1096 (2015).
Haghverdi, L., Büttner, M., Wolf, F. A., Buettner, F. & Theis, F. J. Nature Methods 13, 845–848 (2016).
Schiebinger, G. et al. Cell 176, 928–943 (2019).
Fischer, D. S. et al. Nature Biotechnol. 37, 461–468 (2019).

 Read the paper: Charting cellular identity during human in vitro β-cell differentiation
Read the paper: Charting cellular identity during human in vitro β-cell differentiation
 Peptide secretion triggers diabetes
Peptide secretion triggers diabetes
 Location matters for insulin-producing cells
Location matters for insulin-producing cells